J Cerebrovasc Endovasc Neurosurg.
2014 Jun;16(2):112-118. 10.7461/jcen.2014.16.2.112.
Pipeline Embolization Device for Giant Internal Carotid Artery Aneurysms: 9-Month Follow-Up Results of Two Cases
- Affiliations
-
- 1Department of Neurosurgery, Stroke Center, College of Medicine, Yonsei University Severance Hospital, Seoul, Korea. leejw@yuhs.ac
- 2Department of Radiology, Stroke Center, College of Medicine, Yonsei University Severance Hospital, Seoul, Korea.
- KMID: 1963179
- DOI: http://doi.org/10.7461/jcen.2014.16.2.112
Abstract
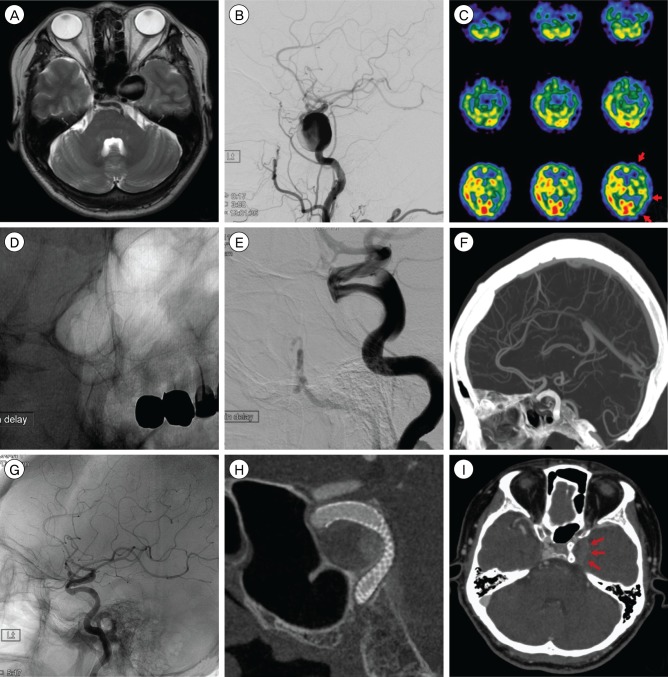
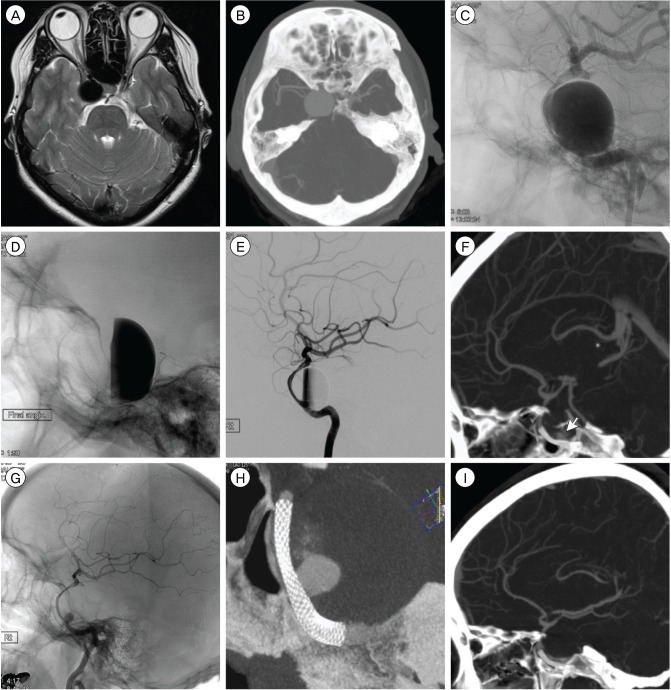
- The pipeline(TM) embolization device (PED) is a braided, tubular, bimetallic endoluminal implant used for occlusion of intracranial aneurysms through flow disruption along the aneurysm neck. The authors report on two cases of giant internal carotid artery aneurysm treated with the PED. In the first case, an aneurysm measuring 26.4 mm was observed at the C3-C4 portion of the left internal carotid artery in a 64-year-old woman who underwent magnetic resonance imaging (MRI) for dizziness and diplopia. In the second case, MRI showed an aneurysm measuring 25 mm at the C4-C5 portion of the right internal carotid artery in a 39-year-old woman with right ptosis and diplopia. Each giant aneurysm was treated with deployment of a PED (3.75 mm diameter/20 mm length and 4.5 mm diameter/25 mm length, respectively). Nine months later, both cases showed complete radiological occlusion of the giant intracranial aneurysm and sac shrinkage. We suggest that use of the PED can be a therapeutic option for giant intracranial aneurysms.
MeSH Terms
Figure
Cited by 1 articles
-
Delayed Ischemic Stroke after Flow Diversion of Large Posterior Communicating Artery Aneurysm
Si On Kim, Yeon Gu Chung, Yu Sam Won, Myung Ho Rho
J Cerebrovasc Endovasc Neurosurg. 2016;18(1):19-26. doi: 10.7461/jcen.2016.18.1.19.
Reference
-
1. Augsburger L, Farhat M, Reymond P, Fonck E, Kulcsar Z, Stergiopulos N, et al. Effect of flow diverter porosity on intraaneurysmal blood flow. Klin Neuroradiol. 2009; 8. 19(3):204–214. PMID: 19705075.
Article2. Barrow DL, Alleyne C. Natural history of giant intracranial aneurysms and indications for intervention. Clin Neurosurg. 1995; 42:214–244. PMID: 8846594.3. Berenstein A, Song JK, Niimi Y, Namba K, Heran NS, Brisman JL, et al. Treatment of cerebral aneurysms with hydrogel-coated platinum coils (HydroCoil): early single-center experience. AJNR Am J Neuroradiol. 2006; 10. 27(9):1834–1840. PMID: 17032853.4. Fiorella D, Albuquerque FC, Deshmukh VR, McDougall CG. Usefulness of the Neuroform stent for the treatment of cerebral aneurysms: results at initial (3-6-mo) follow-up. Neurosurgery. 2005; 6. 56(6):1191–1201. discussion 1201-2. PMID: 15918935.
Article5. Fischer S, Vajda Z, Aguilar Perez M, Schmid E, Hopf N, Bazner H, et al. Pipeline embolization device (PED) for neurovascular reconstruction: initial experience in the treatment of 101 intracranial aneurysms and dissections. Neuroradiology. 2012; 4. 54(4):369–382. PMID: 21881914.
Article6. Fujita K, Yamashita H, Masumura M, Nishizaki T, Tamaki N, Matsumoto S. [Natural history of giant intracranial aneurysms]. No Shinkei Geka. 1988; 3. 16(3):225–231. Japanese. PMID: 3287205.7. Gruber A, Killer M, Bavinzski G, Richling B. Clinical and angiographic results of endosaccular coiling treatment of giant and very large intracranial aneurysms: a 7-year, single-center experience. Neurosurgery. 1999; 10. 45(4):793–803. discussion 803-4. PMID: 10515473.
Article8. Hauck EF, Welch BG, White JA, Replogle RE, Purdy PD, Pride LG, et al. Stent/coil treatment of very large and giant unruptured ophthalmic and cavernous aneurysms. Surg Neurol. 2009; 1. 71(1):19–24. discussion 24. PMID: 18423540.
Article9. Hirsch JA, Chandra RV, Leslie-Mazwi TM. Pipeline, aneurysms and the FDA. J Neurointerv Surg. 2012; 7. 4(4):314. author reply 314. PMID: 22442403.
Article10. Hu YC, Deshmukh VR, Albuquerque FC, Fiorella D, Nixon RR, Heck DV, et al. Histopathological assessment of fatal ipsilateral intraparenchymal hemorrhages after the treatment of supraclinoid aneurysms with the Pipeline Embolization Device. J Neurosurg. 2014; 2. 120(2):365–374. PMID: 24320006.
Article11. Kallmes DF, Ding YH, Dai D, Kadirvel R, Lewis DA, Cloft HJ. A new endoluminal, flow-disrupting device for treatment of saccular aneurysms. Stroke. 2007; 8. 38(8):2346–2352. PMID: 17615366.
Article12. Kallmes DF, Ding YH, Dai D, Kadirvel R, Lewis DA, Cloft HJ. A second-generation, endoluminal, flow-disrupting device for treatment of saccular aneurysms. AJNR Am J Neuroradiol. 2009; 6. 30(6):1153–1158. PMID: 19369609.
Article13. Kan P, Siddiqui AH, Veznedaroglu E, Liebman KM, Binning MJ, Dumont TM, et al. Early postmarket results after treatment of intracranial aneurysms with the pipeline embolization device: a U.S. multicenter experience. Neurosurgery. 2012; 12. 71(6):1080–1087. discussion 1087-8. PMID: 22948199.14. Lieber BB, Stancampiano AP, Wakhloo AK. Alteration of hemodynamics in aneurysm models by stenting: influence of stent porosity. Ann Biomed Eng. 1997; May-Jun. 25(3):460–469. PMID: 9146801.15. Lubicz B, Collignon L, Raphaeli G, De Witte O. Pipeline flow-diverter stent for endovascular treatment of intracranial aneurysms: preliminary experience in 20 patients with 27 aneurysms. World Neurosurg. 2011; Jul-Aug. 76(1-2):114–119. PMID: 21839962.
Article16. Lylyk P, Miranda C, Ceratto R, Ferrario A, Scrivano E, Luna HR, et al. Curative endovascular reconstruction of cerebral aneurysms with the pipeline embolization device: the Buenos Aires experience. Neurosurgery. 2009; 4. 64(4):632–642. discussion 642-3. PMID: 19349825.17. McAuliffe W, Wycoco V, Rice H, Phatouros C, Singh TJ, Wenderoth J. Immediate and midterm results following treatment of unruptured intracranial aneurysms with the pipeline embolization device. AJNR Am J Neuroradiol. 2012; 1. 33(1):164–170. PMID: 21979492.
Article18. Murayama Y, Nien YL, Duckwiler G, Gobin YP, Jahan R, Frazee J, et al. Guglielmi detachable coil embolization of cerebral aneurysms: 11 years' experience. J Neurosurg. 2003; 5. 98(5):959–966. PMID: 12744354.
Article19. Murthy SB, Shah S, Venkatasubba Rao CP, Bershad EM, Suarez JI. Treatment of unruptured intracranial aneurysms with the pipeline embolization device. J Clin Neurosci. 2014; 1. 21(1):6–11. PMID: 24055205.
Article20. Nelson PK, Lylyk P, Szikora I, Wetzel SG, Wanke I, Fiorella D. The pipeline embolization device for the intracranial treatment of aneurysms trial. AJNR Am J Neuroradiol. 2011; 1. 32(1):34–40. PMID: 21148256.
Article21. Piotin M, Blanc R, Spelle L, Mounayer C, Piantino R, Schmidt PJ, et al. Stent-assisted coiling of intracranial aneurysms: clinical and angiographic results in 216 consecutive aneurysms. Stroke. 2010; 1. 41(1):110–115. PMID: 19959540.22. Saatci I, Yavuz K, Ozer C, Geyik S, Cekirge HS. Treatment of intracranial aneurysms using the pipeline flow-diverter embolization device: a single-center experience with long-term follow-up results. AJNR Am J Neuroradiol. 2012; 9. 33(8):1436–1446. PMID: 22821921.
Article23. Sadasivan C, Lieber BB, Cesar L, Miskolczi L, Seong J, Wakhloo AK. Angiographic assessment of the performance of flow divertors to treat cerebral aneurysms. Conf Proc IEEE Eng Med Biol Soc. 2006; 1:3210–3213. PMID: 17946555.
Article24. Seshadhri S, Janiga G, Beuing O, Skalej M, Thevenin D. Impact of stents and flow diverters on hemodynamics in idealized aneurysm models. J Biomech Eng. 2011; 7. 133(7):071005. PMID: 21823744.
Article25. Sluzewski M, Menovsky T, van Rooij WJ, Wijnalda D. Coiling of very large or giant cerebral aneurysms: long-term clinical and serial angiographic results. AJNR Am J Neuroradiol. 2003; 2. 24(2):257–262. PMID: 12591644.26. Szikora I, Berentei Z, Kulcsar Z, Marosfoi M, Vajda ZS, Lee W, et al. Treatment of intracranial aneurysms by functional reconstruction of the parent artery: the Budapest experience with the pipeline embolization device. AJNR Am J Neuroradiol. 2010; 6. 31(6):1139–1147. PMID: 20150304.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Treatment for Giant Fusiform Aneurysm Located in the Cavernous Segment of the Internal Carotid Artery Using the Pipeline Embolization Device
- Balloon Anchor Technique for Pipeline Embolization Device Deployment Across the Neck of a Giant Intracranial Aneurysm
- Flow diverter stenting for intracranial aneurysms in the pediatric population: Two case reports and literature review
- Quantitative Computed Tomographic Volumetry after Treatment of a Giant Intracranial Aneurysm with a Pipeline Embolization Device
- Microsurgical Strategies Following Failed Endovascular Treatment with the Pipeline Embolization Device: Case of a Giant Posterior Cerebral Artery Aneurysm