Cancer Res Treat.
2017 Jul;49(3):748-758. 10.4143/crt.2016.303.
Effects of Postoperative Radiotherapy on Leptomeningeal Carcinomatosis or Dural Metastasis after Resection of Brain Metastases in Breast Cancer Patients
- Affiliations
-
- 1Proton Therapy Center, Research Institute and Hospital, National Cancer Center, Goyang, Korea. jane2000md@gmail.com
- 2Department of Radiation Oncology, Yonsei University College of Medicine, Seoul, Korea. cosuh317@yuhs.ac
- 3Neuro-Oncology Clinic, Research Institute and Hospital, National Cancer Center, Goyang, Korea.
- 4Department of Neurosurgery, Yonsei University College of Medicine, Seoul, Korea.
- 5Department of Neurology, Research Institute and Hospital, National Cancer Center, Goyang, Korea.
- 6Center for Breast Cancer, Research Institute and Hospital, National Cancer Center, Goyang, Korea.
- KMID: 2388320
- DOI: http://doi.org/10.4143/crt.2016.303
Abstract
- PURPOSE
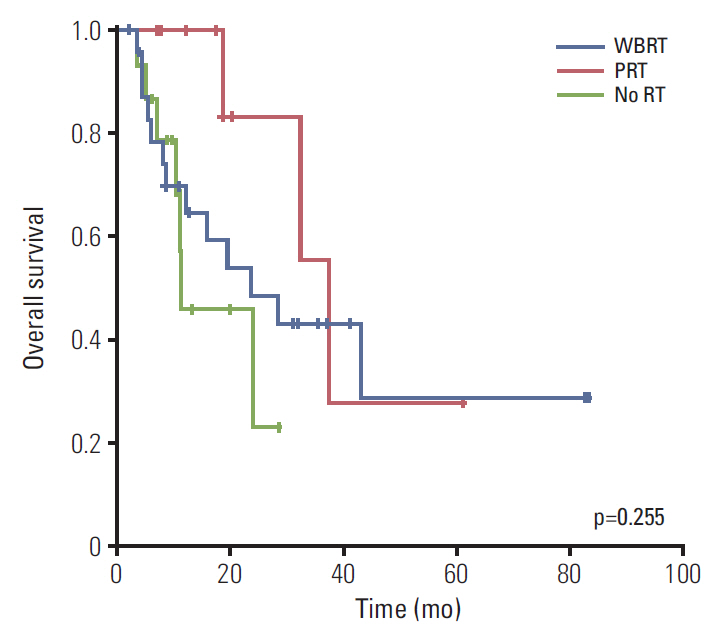
In this retrospective study, we compared the incidence of leptomeningeal carcinomatosis or dural metastasis (LMCDM) in patients who received whole brain radiotherapy (WBRT), partial radiotherapy (PRT), or no radiotherapy (RT) following resection of brain metastases from breast cancer.
MATERIALS AND METHODS
Fifty-one patients with breast cancer underwent surgical resection for newly diagnosed brain metastases in two institutions between March 2001 and March 2015. Among these, 34 received postoperative WBRT (n=24) or PRT (n=10) and 17 did not.
RESULTS
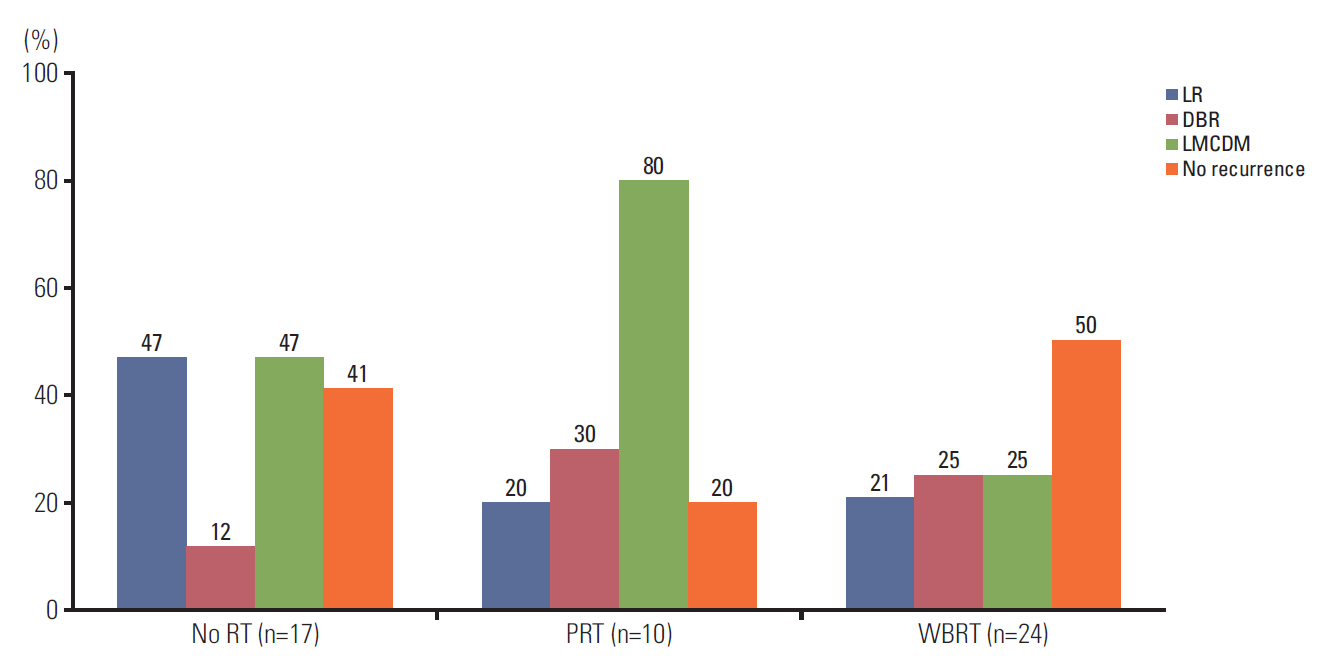
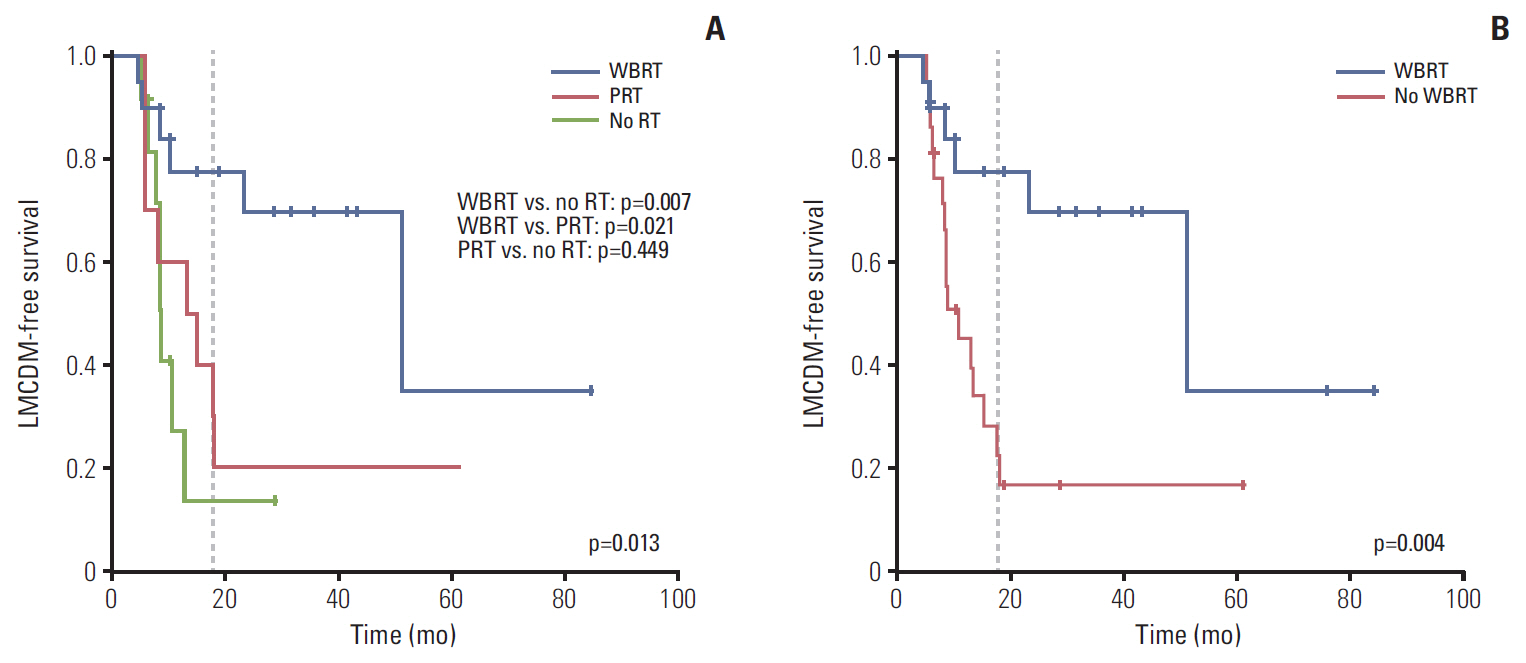
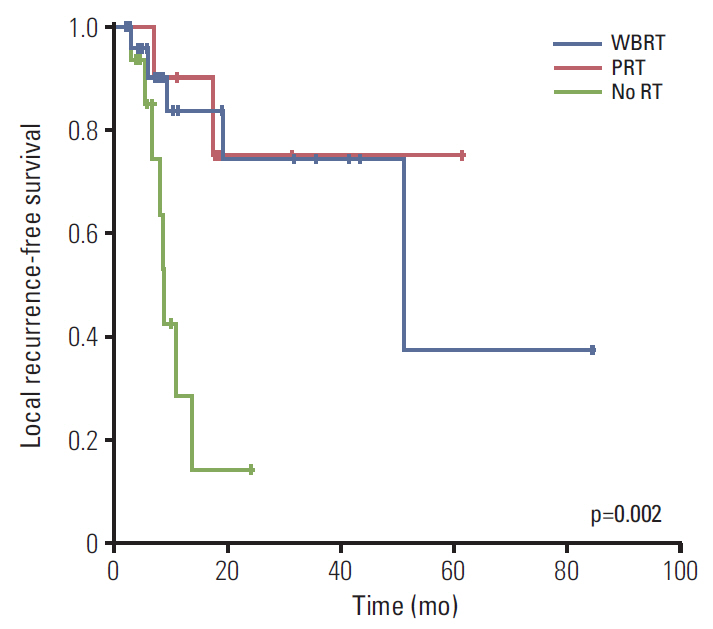
With a median follow-up of 12.4 months (range, 2.3 to 83.6 months), 22/51 patients developed LMCDM at a median of 8.6 months (range, 4.8 to 51.2 months) after surgery. The 18-months LMCDM-free survival (LMCDM-FS) rates were 77.5%, 30.0%, and 13.6%, in the WBRT, PRT, and no RT groups, respectively (p=0.013). The presence of a tumor adjacent to cerebrospinal fluid flow and no systemic treatment after treatment for brain metastases were also associated with poor LMCDM-FS rate. Multivariate analysis showed that WBRT compared to PRT (p=0.009) and systemic treatment (p < 0.001) were independently associated with reduced incidence of LMCDM.
CONCLUSION
WBRT improved LMCDM-FS rate after resection of brain metastases compared to PRT in breast cancer patients.
MeSH Terms
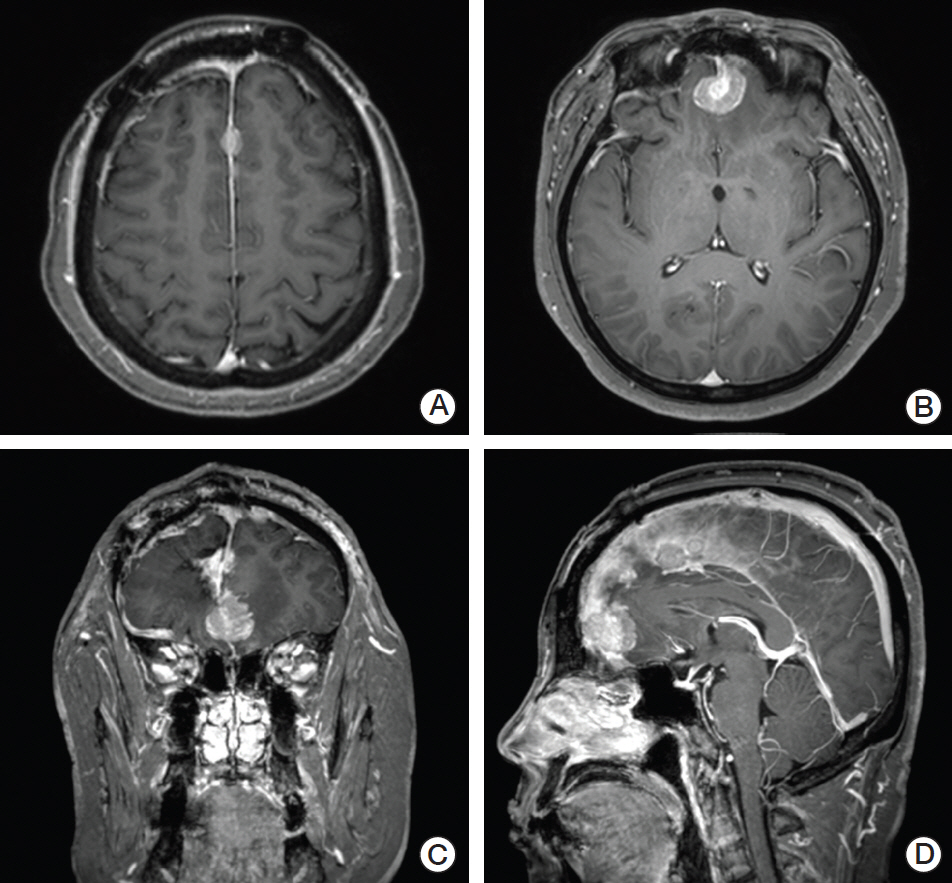
Figure
Cited by 1 articles
-
Revisiting the Role of Surgical Resection for Brain Metastasis
Joonho Byun, Jong Hyun Kim
Brain Tumor Res Treat. 2023;11(1):1-7. doi: 10.14791/btrt.2022.0028.
Reference
-
References
1. Barnholtz-Sloan JS, Sloan AE, Davis FG, Vigneau FD, Lai P, Sawaya RE. Incidence proportions of brain metastases in patients diagnosed (1973 to 2001) in the Metropolitan Detroit Cancer Surveillance System. J Clin Oncol. 2004; 22:2865–72.
Article2. Noordijk EM, Vecht CJ, Haaxma-Reiche H, Padberg GW, Voormolen JH, Hoekstra FH, et al. The choice of treatment of single brain metastasis should be based on extracranial tumor activity and age. Int J Radiat Oncol Biol Phys. 1994; 29:711–7.
Article3. Patchell RA, Tibbs PA, Walsh JW, Dempsey RJ, Maruyama Y, Kryscio RJ, et al. A randomized trial of surgery in the treatment of single metastases to the brain. N Engl J Med. 1990; 322:494–500.
Article4. Kocher M, Soffietti R, Abacioglu U, Villa S, Fauchon F, Baumert BG, et al. Adjuvant whole-brain radiotherapy versus observation after radiosurgery or surgical resection of one to three cerebral metastases: results of the EORTC 22952-26001 study. J Clin Oncol. 2011; 29:134–41.5. Patchell RA, Tibbs PA, Regine WF, Dempsey RJ, Mohiuddin M, Kryscio RJ, et al. Postoperative radiotherapy in the treatment of single metastases to the brain: a randomized trial. JAMA. 1998; 280:1485–9.
Article6. Choi CY, Chang SD, Gibbs IC, Adler JR, Harsh GR 4th, Lieberson RE, et al. Stereotactic radiosurgery of the postoperative resection cavity for brain metastases: prospective evaluation of target margin on tumor control. Int J Radiat Oncol Biol Phys. 2012; 84:336–42.
Article7. Robbins JR, Ryu S, Kalkanis S, Cogan C, Rock J, Movsas B, et al. Radiosurgery to the surgical cavity as adjuvant therapy for resected brain metastasis. Neurosurgery. 2012; 71:937–43.
Article8. Patel KR, Prabhu RS, Kandula S, Oliver DE, Kim S, Hadjipanayis C, et al. Intracranial control and radiographic changes with adjuvant radiation therapy for resected brain metastases: whole brain radiotherapy versus stereotactic radiosurgery alone. J Neurooncol. 2014; 120:657–63.
Article9. Hsieh J, Elson P, Otvos B, Rose J, Loftus C, Rahmathulla G, et al. Tumor progression in patients receiving adjuvant whole-brain radiotherapy vs localized radiotherapy after surgical resection of brain metastases. Neurosurgery. 2015; 76:411–20.
Article10. Sperduto PW, Kased N, Roberge D, Xu Z, Shanley R, Luo X, et al. Effect of tumor subtype on survival and the graded prognostic assessment for patients with breast cancer and brain metastases. Int J Radiat Oncol Biol Phys. 2012; 82:2111–7.
Article11. Dawood S, Gonzalez-Angulo AM, Albarracin C, Yu TK, Hortobagyi GN, Buchholz TA, et al. Prognostic factors of survival in the trastuzumab era among women with breast cancer and brain metastases who receive whole brain radiotherapy: a single-institution review. Cancer. 2010; 116:3084–92.12. Ahn JH, Lee SH, Kim S, Joo J, Yoo H, Lee SH, et al. Risk for leptomeningeal seeding after resection for brain metastases: implication of tumor location with mode of resection. J Neurosurg. 2012; 116:984–93.
Article13. Dosoretz DE, Blitzer PH, Russell AH, Wang CC. Management of solitary metastasis to the brain: the role of elective brain irradiation following complete surgical resection. Int J Radiat Oncol Biol Phys. 1980; 6:1727–30.
Article14. Norris LK, Grossman SA, Olivi A. Neoplastic meningitis following surgical resection of isolated cerebellar metastasis: a potentially preventable complication. J Neurooncol. 1997; 32:215–23.15. Brennan C, Yang TJ, Hilden P, Zhang Z, Chan K, Yamada Y, et al. A phase 2 trial of stereotactic radiosurgery boost after surgical resection for brain metastases. Int J Radiat Oncol Biol Phys. 2014; 88:130–6.
Article16. Chang EL, Wefel JS, Hess KR, Allen PK, Lang FF, Kornguth DG, et al. Neurocognition in patients with brain metastases treated with radiosurgery or radiosurgery plus whole-brain irradiation: a randomised controlled trial. Lancet Oncol. 2009; 10:1037–44.
Article17. Regine WF, Huhn JL, Patchell RA, St Clair WH, Strottmann J, Meigooni A, et al. Risk of symptomatic brain tumor recurrence and neurologic deficit after radiosurgery alone in patients with newly diagnosed brain metastases: results and implications. Int J Radiat Oncol Biol Phys. 2002; 52:333–8.18. Wolfson AH, Bae K, Komaki R, Meyers C, Movsas B, Le Pechoux C, et al. Primary analysis of a phase II randomized trial Radiation Therapy Oncology Group (RTOG) 0212: impact of different total doses and schedules of prophylactic cranial irradiation on chronic neurotoxicity and quality of life for patients with limited-disease small-cell lung cancer. Int J Radiat Oncol Biol Phys. 2011; 81:77–84.
Article19. Huang AJ, Huang KE, Page BR, Ayala-Peacock DN, Lucas JT Jr, Lesser GJ, et al. Risk factors for leptomeningeal carcinomatosis in patients with brain metastases who have previously undergone stereotactic radiosurgery. J Neurooncol. 2014; 120:163–9.
Article20. Ojerholm E, Lee JY, Thawani JP, Miller D, O'Rourke DM, Dorsey JF, et al. Stereotactic radiosurgery to the resection bed for intracranial metastases and risk of leptomeningeal carcinomatosis. J Neurosurg. 2014; 121 Suppl:75–83.
Article21. Atalar B, Modlin LA, Choi CY, Adler JR, Gibbs IC, Chang SD, et al. Risk of leptomeningeal disease in patients treated with stereotactic radiosurgery targeting the postoperative resection cavity for brain metastases. Int J Radiat Oncol Biol Phys. 2013; 87:713–8.
Article22. Jung JM, Kim S, Joo J, Shin KH, Gwak HS, Lee SH. Incidence and risk factors for leptomeningeal carcinomatosis in breast cancer patients with parenchymal brain metastases. J Korean Neurosurg Soc. 2012; 52:193–9.
Article23. Suki D, Abouassi H, Patel AJ, Sawaya R, Weinberg JS, Groves MD. Comparative risk of leptomeningeal disease after resection or stereotactic radiosurgery for solid tumor metastasis to the posterior fossa. J Neurosurg. 2008; 108:248–57.
Article24. Suki D, Hatiboglu MA, Patel AJ, Weinberg JS, Groves MD, Mahajan A, et al. Comparative risk of leptomeningeal dissemination of cancer after surgery or stereotactic radiosurgery for a single supratentorial solid tumor metastasis. Neurosurgery. 2009; 64:664–74.
Article25. Jo KI, Lim DH, Kim ST, Im YS, Kong DS, Seol HJ, et al. Leptomeningeal seeding in patients with brain metastases treated by gamma knife radiosurgery. J Neurooncol. 2012; 109:293–9.
Article26. Trifiletti DM, Romano KD, Xu Z, Reardon KA, Sheehan J. Leptomeningeal disease following stereotactic radiosurgery for brain metastases from breast cancer. J Neurooncol. 2015; 124:421–7.
Article27. Nelson MH, Dolder CR. Lapatinib: a novel dual tyrosine kinase inhibitor with activity in solid tumors. Ann Pharmacother. 2006; 40:261–9.
Article28. De Ieso PB, Schick U, Rosenfelder N, Mohammed K, Ross GM. Breast cancer brain metastases: a 12 year review of treatment outcomes. Breast. 2015; 24:426–33.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Breast Cancer with Leptomeningeal Metastasis
- Brain Metastasis and Leptomeningeal Carcinomatosis in Breast Cancer
- A Case of Cholangiocarcinoma with Brain and Leptomeningeal Carcinomatosis
- Incidence and Risk Factors for Leptomeningeal Carcinomatosis in Breast Cancer Patients with Parenchymal Brain Metastases
- A Case of Leptomeningeal Carcinomatosis Presenting as a Neurological Complication of Stomach Cancer