Investig Clin Urol.
2017 Mar;58(2):109-116. 10.4111/icu.2017.58.2.109.
Long-term adherence to antimuscarinic drugs when treating overactive bladder in the older: Subjective reason and objective factors
- Affiliations
-
- 1Department of Social Sciences, School of Humanities, Far Eastern Federal University, Vladivostok, Russian Federation. oton2000@mail.ru
- 2Department of Theory and Methods of Adaptive Physical Education, Far Eastern Federal University, Vladivostok, Russian Federation.
- 3Department of Urology, City Polyclinic No. 3, Vladivostok, Russian Federation.
- 4Department of Theory and Methods of Adaptive Physical Education, Far Eastern Federal University, Vladivostok, Russian Federation.
- 5Undergrad of the Institute of Humanities, Far Eastern Federal University, Vladivostok, Russian Federation.
- KMID: 2368476
- DOI: http://doi.org/10.4111/icu.2017.58.2.109
Abstract
- PURPOSE
Comparison of subjective reasons for the refusal of antimuscarinic treatment and the state of objective economic, social, psychological and health status markers in the elderly with overactive bladder.
MATERIALS AND METHODS
One thousand seven hundred thirty-six (1,736) patients participated in the experiment: 1,036 or 59.7% of women, and 700 or 40.3% of men aged over 60 years (average age, 68.1 years) who took antimuscarinic (AM) drugs during the year. The control of objective parameters was carried out by studying patients' medical records, the use of overactive bladder questionnaire short form and Medical Outcomes Study 36-item Shor-Form Health Survey, voiding diaries, uroflowmetry, as well as income certificates from the Tax Inspectorate, support documentation for expenses on drugs.
RESULTS
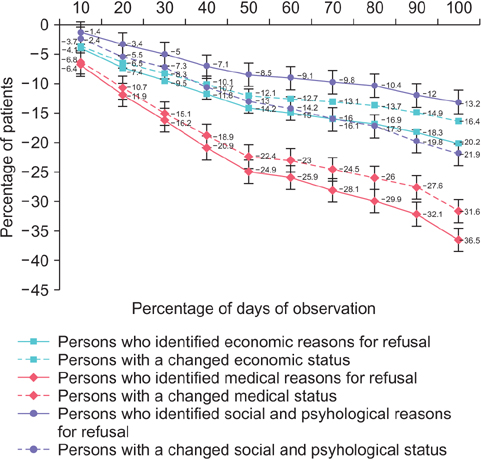
Fifty-two point six percent (52.6%) of patients preserved adherence to treatment during the first 6 months, 30.1% - during the follow-up period. The average time of reaching a 30-day break in the AM drugs administration was 174 days. In 36.5% of cases of the refusal of treatment, patients referred to medical reasons for the refusal, in 31.6% of cases disturbance was established in objective health status markers (differences were significant in 30% of the follow-up time). The percentage of refusals of treatment for social and psychological reasons (13.2%) was significantly lower (p≤0.05), than the percentage of individuals with statuses altered objectively (21.9%).
CONCLUSIONS
A significant share of elderly patients taking AM drugs when treating overactive bladder is inclined to overestimate the importance of health factors influencing their decisions and to underestimate the importance of social and psychological factors, and an urologist should take it into account for the efficacy evaluation.
MeSH Terms
Figure
Reference
-
1. Sexton CC, Coyne KS, Thompson C, Bavendam T, Chen CI, Markland A. Prevalence and effect on health-related quality of life of overactive bladder in older americans: results from the epidemiology of lower urinary tract symptoms study. J Am Geriatr Soc. 2011; 59:1465–1470.2. Milsom I, Kaplan SA, Coyne KS, Sexton CC, Kopp ZS. Effect of bothersome overactive bladder symptoms on health-related quality of life, anxiety, depression, and treatment seeking in the United States: results from EpiLUTS. Urology. 2012; 80:90–96.3. Coyne KS, Sexton CC, Clemens JQ, Thompson CL, Chen CI, Bavendam T, et al. The impact of OAB on physical activity in the United States: results from OAB-POLL. Urology. 2013; 82:799–806.4. Onukwugha E, Zuckerman IH, McNally D, Coyne KS, Vats V, Mullins CD. The total economic burden of overactive bladder in the United States: a disease-specific approach. Am J Manag Care. 2009; 15:4 Suppl. S90–S97.5. Felicilda-Reynaldo RF. A review of anticholinergic medications for overactive bladder symptoms. Medsurg Nurs. 2013; 22:119–123.6. Andersson KE. Antimuscarinics for treatment of overactive bladder. Lancet Neurol. 2004; 3:46–53.7. Kosilov KV, Loparev SA, Ivanovskaya MA, Kosilova LV. Randomized controlled trial of cyclic and continuous therapy with trospium and solifenacin combination for severe overactive bladder in elderly patients with regard to patient compliance. Ther Adv Urol. 2014; 6:215–223.8. Kosilov K, Loparev S, Iwanowskaya M, Kosilova L. Effectiveness of combined high-dosed trospium and solifenacin depending on severity of OAB symptoms in elderly men and women under cyclic therapy. Cent European J Urol. 2014; 67:43–48.9. Veenboer PW, Bosch JL. Long-term adherence to antimuscarinic therapy in everyday practice: a systematic review. J Urol. 2014; 191:1003–1008.10. Chancellor MB, Migliaccio-Walle K, Bramley TJ, Chaudhari SL, Corbell C, Globe D. Long-term patterns of use and treatment failure with anticholinergic agents for overactive bladder. Clin Ther. 2013; 35:1744–1751.11. Basra RK, Wagg A, Chapple C, Cardozo L, Castro-Diaz D, Pons ME, et al. A review of adherence to drug therapy in patients with overactive bladder. BJU Int. 2008; 102:774–779.12. Oefelein MG. Safety and tolerability profiles of anticholinergic agents used for the treatment of overactive bladder. Drug Saf. 2011; 34:733–754.13. Gopal M, Haynes K, Bellamy SL, Arya LA. Discontinuation rates of anticholinergic medications used for the treatment of lower urinary tract symptoms. Obstet Gynecol. 2008; 112:1311–1318.14. Brubaker L, Fanning K, Goldberg EL, Benner JS, Trocio JN, Bavendam T, et al. Predictors of discontinuing overactive bladder medications. BJU Int. 2010; 105:1283–1290.15. Wagg A, Compion G, Fahey A, Siddiqui E. Persistence with prescribed antimuscarinic therapy for overactive bladder: a UK experience. BJU Int. 2012; 110:1767–1774.16. Sears CL, Lewis C, Noel K, Albright TS, Fischer JR. Overactive bladder medication adherence when medication is free to patients. J Urol. 2010; 183:1077–1081.17. Brostrøm S, Hallas J. Persistence of antimuscarinic drug use. Eur J Clin Pharmacol. 2009; 65:309–314.18. Campbell UB, Stang P, Barron R. Survey assessment of continuation of and satisfaction with pharmacological treatment for urinary incontinence. Value Health. 2008; 11:726–732.19. Kleinman NL, Odell K, Chen CI, Atkinson A, Zou KH. Persistence and adherence with urinary antispasmodic medications among employees and the impact of adherence on costs and absenteeism. J Manag Care Spec Pharm. 2014; 20:1047–1056.20. Harpe SE, Szeinbach SL, Caswell RJ, Corey R, McAuley JW. The relative importance of health related quality of life and prescription insurance coverage in the decision to pharmacologically manage symptoms of overactive bladder. J Urol. 2007; 178:2532–2536.21. Jin J, Sklar GE, Min Sen, Chuen Li S. Factors affecting therapeutic compliance: A review from the patient's perspective. Ther Clin Risk Manag. 2008; 4:269–286.22. Clifford S, Coyne KS. What is the value of medication adherence? J Manag Care Spec Pharm. 2014; 20:650–651.23. Schröder A, Abrams P, Andersson KE, Artibani W, Chapple CR, Drake MJ, et al. Guidelines on urinary incontinence. Anheim (NL): European Association of Urology;2010.24. Kosilov KV, Loparev SA, Ivanovskaya MA, Kosilova LV. Randomized controlled trial of cyclic and continuous therapy with trospium and solifenacin combination for severe overactive bladder in elderly patients with regard to patient compliance. Ther Adv Urol. 2014; 6:215–223.25. Yu YF, Nichol MB, Yu AP, Ahn J. Persistence and adherence of medications for chronic overactive bladder/urinary incontinence in the california medicaid program. Value Health. 2005; 8:495–505.26. Coyne KS, Thompson CL, Lai JS, Sexton CC. An overactive bladder symptom and health-related quality of life short-form: validation of the OAB-q SF. Neurourol Urodyn. 2015; 34:255–263.27. Amundsen CL, Parsons M, Cardozo L, Vella M, Webster GD, Coats AC. Bladder diary volume per void measurements in detrusor overactivity. J Urol. 2006; 176(6 Pt 1):2530–2534.28. Dmochowski R, Larson-Peters A, Aronstein W, Seifu Y. Efficacy of darifenacin in patients with varying baseline symptom. UroToday Int J. 2009; 2(3):29. Yang M, Wang H, Wang J, Ruan M. Impact of invasive bladder cancer and orthotopic urinary diversion on general health-related quality of life: An SF-36 survey. Mol Clin Oncol. 2013; 1:758–762.30. Vecchioli Scaldazza C, Morosetti C, Pace G, Azizi B, Giannubilo W, Ferrara V. Has the cost of anti-muscarinic a key role in the success rate of patients diagnosed with overactive bladder syndrome? Arch Ital Urol Androl. 2012; 84:68–73.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Review of the Anticholinergics for the Treatment of Overactive Bladder: 2009 Update
- Medical Treatment of Overactive Bladder
- Predictors of Antimuscarinic Treatment Response for Female Patients with Overactive Bladder
- The Analysis of Persistent Overactive Bladder Syndrome after Sling Surgery in Female Stress Urinary Incontinence
- Persistence and compliance with medication management in the treatment of overactive bladder