J Cerebrovasc Endovasc Neurosurg.
2016 Dec;18(4):396-401. 10.7461/jcen.2016.18.4.396.
Spontaneous Aggressive Conversion of Venous Drainage Pattern in Dural Arteriovenous Fistula Treated with Onyx Embolization
- Affiliations
-
- 1Department of Neurosurgery, Kyung Hee University Hospital, College of Medicine, Kyung Hee University, Seoul, Korea.
- 2Department of Radiology, Kyung Hee University Hospital, College of Medicine, Kyung Hee University, Seoul, Korea. euijkim@hanmail.net
- KMID: 2367333
- DOI: http://doi.org/10.7461/jcen.2016.18.4.396
Abstract
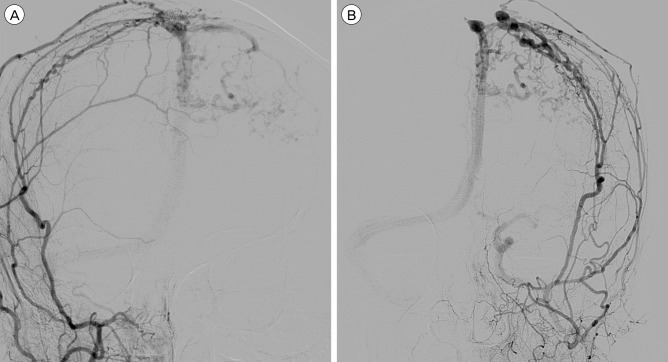
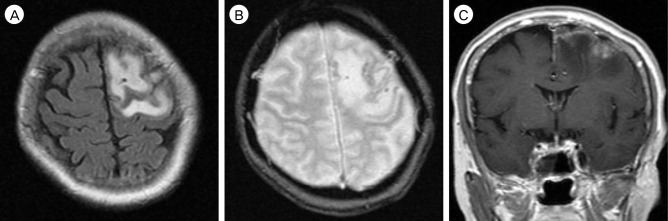
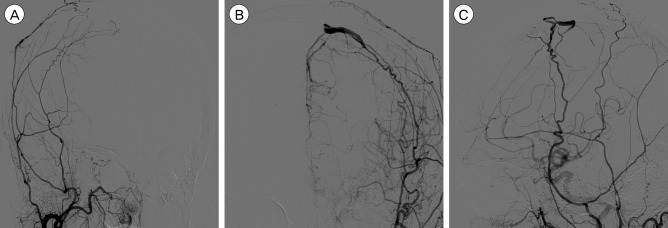
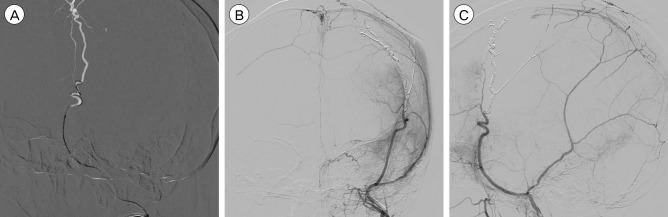
- We report a case of dural arteriovenous fistula (DAVF) that showed spontaneous conversion of venous drainage pattern from Borden type II to type III within a four month period of follow-up. Upon admission, the patient presented with aggravated neurologic status and newly developed seizure. After admission, endovascular embolization was performed through the middle meningeal artery with Onyx®. Complete obliteration of dural arteriovenous shunt was confirmed by angiography, and the patient's clinical symptoms improved. Although most cases of DAVF show benign clinical course and conversion pattern, close follow-up is required to detect potential aggravation.
Keyword
MeSH Terms
Figure
Reference
-
1. Al-Afif S, Nakamura M, Gotz F, Krauss JK. Spontaneous closure of a dural arteriovenous fistula. BMJ Case Rep. 2014; 7. 21:1–6.
Article2. Awad IA, Little JR, Akarawi WP, Ahl J. Intracranial dural arteriovenous malformations: factors predisposing to an aggressive neurological course. J Neurosurg. 1990; 6. 72(6):839–850. PMID: 2140125.
Article3. Bertalanffy A, Dietrich W, Kitz K, Bavinzski G. Treatment of dural arteriovenous fistulae (dAVF's) at the superior sagittal sinus (SSS) using embolisation combined with micro- or radiosurgery. Minim Invasive Neurosurg. 2001; 12. 44(4):205–210. PMID: 11830779.
Article4. Chaudhary MY, Sachdev VP, Cho SH, Weitzner I Jr, Puljic S, Huang YP. Dural arteriovenous malformation of the major venous sinuses: an acquired lesion. AJNR Am J Neuroradiol. 1982; Jan-Feb. 3(1):13–19. PMID: 6800236.5. Clarencon F, Biondi A, Sourour NA, Di Maria F, Iosif C, Nouet A, et al. Spontaneous closure of intracranial dural arteriovenous fistulas: a report of 3 cases. Clin Neurol Neurosurg. 2013; 7. 115(7):971–975. PMID: 23159510.6. Cognard C, Januel AC, Silva NA Jr, Tall P. Endovascular treatment of intracranial dural arteriovenous fistulas with cortical venous drainage: new management using Onyx. AJNR Am J Neuroradiol. 2008; 2. 29(2):235–241. PMID: 17989374.
Article7. Davies MA, TerBrugge K, Willinsky R, Coyne T, Saleh J, Wallace MC. The validity of classification for the clinical presentation of intracranial dural arteriovenous fistulas. J Neurosurg. 1996; 11. 85(5):830–837. PMID: 8893721.
Article8. Fermand M, Reizine D, Melki JP, Riche MC, Merland JJ. Long term follow-up of 43 pure dural arteriovenous fistulae (AVF) of the lateral sinus. Neuroradiology. 1987; 29(4):348–353. PMID: 3627416.
Article9. Ghobrial GM, Marchan E, Nair AK, Dumont AS, Tjoumakaris SI, Gonzalez LF, et al. Dural arteriovenous fistulas: a review of the literature and a presentation of a single institution's experience. World Neurosurg. 2013; Jul-Aug. 80(1-2):94–102. PMID: 22381858.
Article10. Halbach VV, Higashida RT, Hieshima GB, Rosenblum M, Cahan L. Treatment of dural arteriovenous malformations involving the superior sagittal sinus. AJNR Am J Neuroradiol. 1988; Mar-Apr. 9(2):337–343. PMID: 3128082.11. Kim DJ, terBrugge K, Krings T, Willinsky R, Wallace C. Spontaneous angiographic conversion of intracranial dural arteriovenous shunt: long-term follow-up in nontreated patients. Stroke. 2010; 7. 41(7):1489–1494. PMID: 20522815.12. Luciani A, Houdart E, Mounayer C, Saint Maurice JP, Merland JJ. Spontaneous closure of dural arteriovenous fistulas: report of three cases and review of the literature. AJNR Am J Neuroradiol. 2001; 5. 22(5):992–996. PMID: 11337347.13. Lv X, Jiang C, Zhang J, Li Y, Wu Z. Complications related to percutaneous transarterial embolization of intracranial dural arteriovenous fistulas in 40 patients. AJNR Am J Neuroradiol. 2009; 3. 30(3):462–468. PMID: 19131416.
Article14. Natarajan SK, Ghodke B, Kim LJ, Hallam DK, Britz GW, Sekhar LN. Multimodality treatment of intracranial dural arteriovenous fistulas in the Onyx era: a single center experience. World Neurosurg. 2010; 4. 73(4):365–379. PMID: 20849795.
Article15. Piske RL, Campos CM, Chaves JB, Abicalaf R, Dabus G, Batista LL, et al. Dural sinus compartment in dural arteriovenous shunts: a new angioarchitectural feature allowing superselective transvenous dural sinus occlusion treatment. AJNR Am J Neuroradiol. 2005; 8. 26(7):1715–1722. PMID: 16091520.16. Saito A, Furuno Y, Nishimura S, Kamiyama H, Nishijima M. Spontaneous closure of transverse sinus dural arteriovenous fistula: case report. Neurol Med Chir (Tokyo). 008; 12. 48(12):564–568. PMID: 19106495.17. Santillan A, Nanaszko M, Burkhardt JK, Patsalides A, Gobin YP, Riina HA. Endovascular management of intracranial dural arteriovenous fistulas: a review. Clin Neurol Neurosurg. 2013; 3. 115(3):241–251. PMID: 23287743.
Article18. Satomi J, van Dijk JM, Terbrugge KG, Willinsky RA, Wallace MC. Benign cranial dural arteriovenous fistulas: outcome of conservative management based on the natural history of the lesion. J Neurosurg. 2002; 10. 97(4):767–770. PMID: 12405361.
Article19. Soderman M, Pavic L, Edner G, Holmin S, Andersson T. Natural history of dural arteriovenous shunts. Stroke. 2008; 6. 39(6):1735–1739. PMID: 18388337.
Article20. Stiefel MF, Albuquerque FC, Park MS, Dashti SR, McDougall CG. Endovascular treatment of intracranial dural arteriovenous fistulae using Onyx: a case series. Neurosurgery. 2009; 12. 65(6 Suppl):132–139. discussion 139-40. PMID: 19934987.
Article21. Tsai LK, Jeng JS, Liu HM, Wang HJ, Yip PK. Intracranial dural arteriovenous fistulas with or without cerebral sinus thrombosis: analysis of 69 patients. J Neurol Neurosurg Psychiatry. 2004; 11. 75(11):1639–1641. PMID: 15489406.
Article22. van Dijk JM, terBrugge KG, Willinsky RA, Wallace MC. Clinical course of cranial dural arteriovenous fistulas with long-term persistent cortical venous reflux. Stroke. 2002; 5. 33(5):1233–1236. PMID: 11988596.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Dural Arteriovenous Fistula Involving Transverse Sinus: Successful Embolization Using Onyx(R)
- Onyx Embolization of Dural Arteriovenous Fistula, using Scepter C Balloon Catheter: a Case Report
- Hairball-Like Migration of “Onyx Threads” into the Draining Vein during Transarterial Embolization of a Dural Arteriovenous Fistula: A Case Report and Experimental Validation
- Cortical versus Pial Venous Drainage in Dural Arteriovenous Fistula
- Dural Arteriovenous Fistula Involving an Isolated Sinus Treated Using Transarterial Onyx Embolization