Clin Exp Vaccine Res.
2017 Jan;6(1):15-21. 10.7774/cevr.2017.6.1.15.
The development of mucosal vaccines for both mucosal and systemic immune induction and the roles played by adjuvants
- Affiliations
-
- 1Department of Molecular Biology and Institute for Molecular Biology and Genetics, Chonbuk National University, Jeonju, Korea. yongsuk@jbnu.ac.kr
- 2Department of Bioactive Material Sciences and Research Center of Bioactive Materials, Chonbuk National University, Jeonju, Korea.
- KMID: 2366887
- DOI: http://doi.org/10.7774/cevr.2017.6.1.15
Abstract
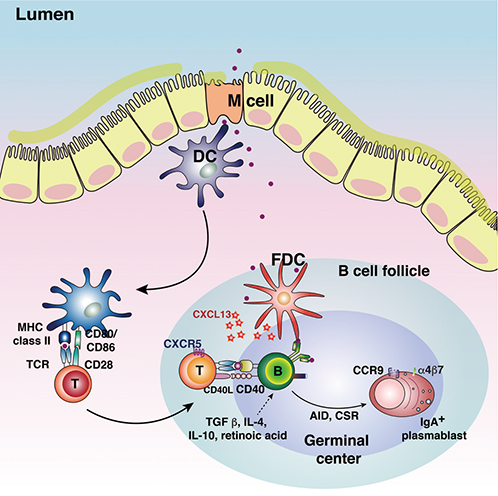
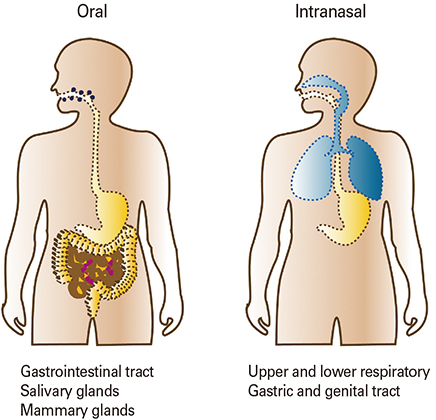
- Vaccination is the most successful immunological practice that improves the quality of human life and health. Vaccine materials include antigens of pathogens and adjuvants potentiating the effectiveness of vaccination. Vaccines are categorized using various criteria, including the vaccination material used and the method of administration. Traditionally, vaccines have been injected via needles. However, given that most pathogens first infect mucosal surfaces, there is increasing interest in the establishment of protective mucosal immunity, achieved by vaccination via mucosal routes. This review summarizes recent developments in mucosal vaccines and their associated adjuvants.
Keyword
Figure
Reference
-
1. Rappuoli R, Mandl CW, Black S, De Gregorio E. Vaccines for the twenty-first century society. Nat Rev Immunol. 2011; 11:865–872.
Article2. Kwok R. Vaccines: the real issues in vaccine safety. Nature. 2011; 473:436–438.
Article3. Gutjahr A, Tiraby G, Perouzel E, Verrier B, Paul S. Triggering intracellular receptors for vaccine adjuvantation. Trends Immunol. 2016; 37:573–587.
Article4. Bachmann MF, Jennings GT. Vaccine delivery: a matter of size, geometry, kinetics and molecular patterns. Nat Rev Immunol. 2010; 10:787–796.
Article5. McGhee JR, Fujihashi K. Inside the mucosal immune system. PLoS Biol. 2012; 10:e1001397.
Article6. Brandtzaeg P, Kiyono H, Pabst R, Russell MW. Terminology: nomenclature of mucosa-associated lymphoid tissue. Mucosal Immunol. 2008; 1:31–37.
Article7. Corr SC, Gahan CC, Hill C. M-cells: origin, morphology and role in mucosal immunity and microbial pathogenesis. FEMS Immunol Med Microbiol. 2008; 52:2–12.
Article8. Ohno H. Intestinal M cells. J Biochem. 2016; 159:151–160.
Article9. Schulz O, Pabst O. Antigen sampling in the small intestine. Trends Immunol. 2013; 34:155–161.
Article10. Cerutti A, Chen K, Chorny A. Immunoglobulin responses at the mucosal interface. Annu Rev Immunol. 2011; 29:273–293.
Article11. Bemark M, Boysen P, Lycke NY. Induction of gut IgA production through T cell-dependent and T cell-independent pathways. Ann N Y Acad Sci. 2012; 1247:97–116.
Article12. Pabst O. New concepts in the generation and functions of IgA. Nat Rev Immunol. 2012; 12:821–832.
Article13. Strugnell RA, Wijburg OL. The role of secretory antibodies in infection immunity. Nat Rev Microbiol. 2010; 8:656–667.
Article14. Lycke N. Recent progress in mucosal vaccine development: potential and limitations. Nat Rev Immunol. 2012; 12:592–605.
Article15. Sallusto F, Lanzavecchia A, Araki K, Ahmed R. From vaccines to memory and back. Immunity. 2010; 33:451–463.
Article16. Kim SH, Jang YS. Antigen targeting to M cells for enhancing the efficacy of mucosal vaccines. Exp Mol Med. 2014; 46:e85.
Article17. Pedersen G, Cox R. The mucosal vaccine quandary: intranasal vs. sublingual immunization against influenza. Hum Vaccin Immunother. 2012; 8:689–693.
Article18. Lamichhane A, Azegamia T, Kiyonoa H. The mucosal immune system for vaccine development. Vaccine. 2014; 32:6711–6723.
Article19. Mabbott NA, Donaldson DS, Ohno H, Williams IR, Mahajan A. Microfold (M) cells: important immunosurveillance posts in the intestinal epithelium. Mucosal Immunol. 2013; 6:666–677.
Article20. Clark MA, Jepson MA, Simmons NL, Hirst BH. Differential surface characteristics of M cells from mouse intestinal Peyer’s and caecal patches. Histochem J. 1994; 26:271–280.
Article21. Foster N, Clark MA, Jepson MA, Hirst BH. Ulex europaeus 1 lectin targets microspheres to mouse Peyer's patch M-cells in vivo. Vaccine. 1998; 16:536–541.
Article22. Hirabayashi J, Hashidate T, Arata Y, et al. Oligosaccharide specificity of galectins: a search by frontal affinity chromatography. Biochim Biophys Acta. 2002; 1572:232–254.
Article23. Kim SH, Jung DI, Yang IY, et al. M cells expressing the complement C5a receptor are efficient targets for mucosal vaccine delivery. Eur J Immunol. 2011; 41:3219–3229.
Article24. Kim SH, Lee HY, Jang YS. Expression of the ATP-gated P2X7 receptor on M cells and its modulating role in the mucosal immune environment. Immune Netw. 2015; 15:44–49.
Article25. Kim SH, Yang IY, Kim J, Lee KY, Jang YS. Antimicrobial peptide LL-37 promotes antigen-specific immune responses in mice by enhancing Th17-skewed mucosal and systemic immunities. Eur J Immunol. 2015; 45:1402–1413.
Article26. Clark MA, Hirst BH, Jepson MA. M-cell surface beta1 integrin expression and invasin-mediated targeting of Yersinia pseudotuberculosis to mouse Peyer's patch M cells. Infect Immun. 1998; 66:1237–1243.
Article27. Hase K, Kawano K, Nochi T, et al. Uptake through glycoprotein 2 of FimH(+) bacteria by M cells initiates mucosal immune response. Nature. 2009; 462:226–230.
Article28. Keely S, Glover LE, Weissmueller T, et al. Hypoxia-inducible factor-dependent regulation of platelet-activating factor receptor as a route for gram-positive bacterial translocation across epithelia. Mol Biol Cell. 2010; 21:538–546.
Article29. Kunisawa J, Kurashima Y, Kiyono H. Gut-associated lymphoid tissues for the development of oral vaccines. Adv Drug Deliv Rev. 2012; 64:523–530.
Article30. Kyd JM, Cripps AW. Functional differences between M cells and enterocytes in sampling luminal antigens. Vaccine. 2008; 26:6221–6224.31. Lo DD, Ling J, Eckelhoefer AH. M cell targeting by a Claudin 4 targeting peptide can enhance mucosal IgA responses. BMC Biotechnol. 2012; 12:7.32. Nakato G, Hase K, Suzuki M, et al. Cutting Edge: Brucella abortus exploits a cellular prion protein on intestinal M cells as an invasive receptor. J Immunol. 2012; 189:1540–1544.
Article33. Nochi T, Yuki Y, Matsumura A, et al. A novel M cell-specific carbohydrate-targeted mucosal vaccine effectively induces antigen-specific immune responses. J Exp Med. 2007; 204:2789–2796.
Article34. Osanai A, Sashinami H, Asano K, Li SJ, Hu DL, Nakane A. Mouse peptidoglycan recognition protein PGLYRP-1 plays a role in the host innate immune response against Listeria monocytogenes infection. Infect Immun. 2011; 79:858–866.
Article35. Rand JH, Wu XX, Lin EY, Griffel A, Gialanella P, McKitrick JC. Annexin A5 binds to lipopolysaccharide and reduces its endotoxin activity. MBio. 2012; 3:pii: e00292-11.
Article36. Sato S, Kaneto S, Shibata N, et al. Transcription factor Spi-B-dependent and -independent pathways for the development of Peyer's patch M cells. Mucosal Immunol. 2013; 6:838–846.
Article37. Shafique M, Wilschut J, de Haan A. Induction of mucosal and systemic immunity against respiratory syncytial virus by inactivated virus supplemented with TLR9 and NOD2 ligands. Vaccine. 2012; 30:597–606.
Article38. Tyrer P, Foxwell AR, Cripps AW, Apicella MA, Kyd JM. Microbial pattern recognition receptors mediate M-cell uptake of a gram-negative bacterium. Infect Immun. 2006; 74:625–631.
Article39. Wolf JL, Kauffman RS, Finberg R, Dambrauskas R, Fields BN, Trier JS. Determinants of reovirus interaction with the intestinal M cells and absorptive cells of murine intestine. Gastroenterology. 1983; 85:291–300.
Article40. Kim SH, Seo KW, Kim J, Lee KY, Jang YS. The M cell-targeting ligand promotes antigen delivery and induces antigen-specific immune responses in mucosal vaccination. J Immunol. 2010; 185:5787–5795.
Article41. Agren LC, Ekman L, Lowenadler B, Lycke NY. Genetically engineered nontoxic vaccine adjuvant that combines B cell targeting with immunomodulation by cholera toxin A1 subunit. J Immunol. 1997; 158:3936–3946.
Article42. Chen K, Cerutti A. Vaccination strategies to promote mucosal antibody responses. Immunity. 2010; 33:479–491.
Article43. Christensen D, Agger EM, Andreasen LV, Kirby D, Andersen P, Perrie Y. Liposome-based cationic adjuvant formulations (CAF): past, present, and future. J Liposome Res. 2009; 19:2–11.
Article44. Eliasson DG, Helgeby A, Schon K, et al. A novel non-toxic combined CTA1-DD and ISCOMS adjuvant vector for effective mucosal immunization against influenza virus. Vaccine. 2011; 29:3951–3961.
Article45. Manicassamy S, Pulendran B. Modulation of adaptive immunity with Toll-like receptors. Semin Immunol. 2009; 21:185–193.
Article46. Thompson AL, Johnson BT, Sempowski GD, et al. Maximal adjuvant activity of nasally delivered IL-1alpha requires adjuvant-responsive CD11c(+) cells and does not correlate with adjuvant-induced in vivo cytokine production. J Immunol. 2012; 188:2834–2846.
Article47. Uematsu S, Fujimoto K, Jang MH, et al. Regulation of humoral and cellular gut immunity by lamina propria dendritic cells expressing Toll-like receptor 5. Nat Immunol. 2008; 9:769–776.
Article48. van der Lubben IM, Verhoef JC, Borchard G, Junginger HE. Chitosan for mucosal vaccination. Adv Drug Deliv Rev. 2001; 52:139–144.
Article49. Winstone N, Wilson AJ, Morrow G, et al. Enhanced control of pathogenic Simian immunodeficiency virus SIVmac239 replication in macaques immunized with an interleukin-12 plasmid and a DNA prime-viral vector boost vaccine regimen. J Virol. 2011; 85:9578–9587.
Article50. Agren L, Sverremark E, Ekman L, et al. The ADP-ribosylating CTA1-DD adjuvant enhances T cell-dependent and independent responses by direct action on B cells involving anti-apoptotic Bcl-2- and germinal center-promoting effects. J Immunol. 2000; 164:6276–6286.
Article51. Mastelic Gavillet B, Eberhardt CS, Auderset F, et al. MF59 Mediates Its B Cell Adjuvanticity by Promoting T Follicular Helper Cells and Thus Germinal Center Responses in Adult and Early Life. J Immunol. 2015; 194:4836–4845.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Mucosal vaccine adjuvants update
- Development of mucosal vaccine delivery: an overview on the mucosal vaccines and their adjuvants
- Mucosal Immune System and M Cell-targeting Strategies for Oral Mucosal Vaccination
- New era for mucosal mast cells: their roles in inflammation, allergic immune responses and adjuvant development
- Microbiota Influences Vaccine and Mucosal Adjuvant Efficacy