Pediatr Infect Vaccine.
2016 Dec;23(3):229-235. 10.14776/piv.2016.23.3.229.
Infective Endocarditis Caused by Methicillin-Resistant Staphylococcus aureus Combined with Meningitis
- Affiliations
-
- 1Department of Pediatrics, Eulji University Hospital, Eulji University School of Medicine, Daejeon, Korea. sara67770@eulji.ac.kr
- KMID: 2362483
- DOI: http://doi.org/10.14776/piv.2016.23.3.229
Abstract
- Infective endocarditis (IE) caused by methicillin-resistant Staphylococcus aureus (MRSA) has become a worldwide concern. We present a case of a 12-year-old child with IE of the native mitral valve due to MRSA infection after an invasive dental procedure. Based on the clinical symptoms and the presence of cerebrospinal fluid pleocytosis, the patient was initially diagnosed with presumed bacterial meningitis and treated with empiric antibiotics. On the third day of hospitalization, MRSA was cultured from the initial blood samples and vegetation was observed on the mitral valve during an echocardiogram, findings which are compatible with a diagnosis of IE. The revised guidelines for antibiotic prophylaxis for the prevention of IE advise that IE prophylaxis for dental procedures is reasonable only for patients with underlying cardiac conditions, who are at the highest risk of adverse outcomes from IE. However, in this case, the patient had no high risk factors indicative of IE prophylaxis, except for mitral valve prolapse. She had no recurrence of IE over a follow-up period of 12 months.
Keyword
MeSH Terms
-
Anti-Bacterial Agents
Antibiotic Prophylaxis
Cerebrospinal Fluid
Child
Diagnosis
Endocarditis*
Follow-Up Studies
Hospitalization
Humans
Leukocytosis
Meningitis*
Meningitis, Bacterial
Methicillin Resistance*
Methicillin-Resistant Staphylococcus aureus*
Mitral Valve
Mitral Valve Prolapse
Recurrence
Risk Factors
Anti-Bacterial Agents
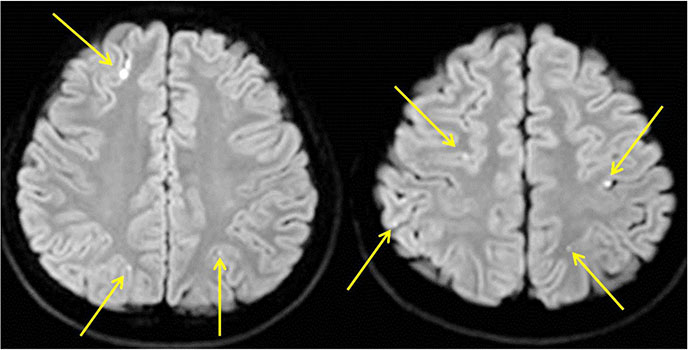
Figure
Reference
-
1. Moreillon P, Que YA. Infective endocarditis. Lancet. 2004; 363:139–149.
Article2. Gunebakmaz O, Kaya MG, Kaya EG, Ardic I, Yarlioglues M, Dogdu O, et al. Mean platelet volume predicts embolic complications and prognosis in infective endocarditis. Int J Infect Dis. 2010; 14:e982–e985.
Article3. San Roman JA, Vilacosta I, Lopez J, Sarria C. Critical questions about left-sided infective endocarditis. J Am Coll Cardiol. 2015; 66:1068–1076.
Article4. Dickerman SA, Abrutyn E, Barsic B, Bouza E, Cecchi E, Moreno A, et al. The relationship between the initiation of antimicrobial therapy and the incidence of stroke in infective endocarditis: an analysis from the ICE Prospective Cohort Study (ICE-PCS). Am Heart J. 2007; 154:1086–1094.
Article5. Coward K, Tucker N, Darville T. Infective endocarditis in Arkansan children from 1990 through 2002. Pediatr Infect Dis J. 2003; 22:1048–1052.
Article6. Kovarik A, Setina M, Sulda M, Pazderkova P, Mokracek A. Infective endocarditis of the tricuspid valve caused by Staphylococcus aureus after ear piercing. Scand J Infect Dis. 2007; 39:266–268.
Article7. Marom D, Ashkenazi S, Samra Z, Birk E. Infective endocarditis in previously healthy children with structurally normal hearts. Pediatr Cardiol. 2013; 34:1415–1421.
Article8. Fowler VG Jr, Miro JM, Hoen B, Cabell CH, Abrutyn E, Rubinstein E, et al. Staphylococcus aureus endocarditis: a consequence of medical progress. JAMA. 2005; 293:3012–3021.9. Hoen B, Duval X. Clinical practice. Infective endocarditis. N Engl J Med. 2013; 368:1425–1433.10. Selton-Suty C, Celard M, Le Moing V, Doco-Lecompte T, Chirouze C, Iung B, et al. Preeminence of Staphylococcus aureus in infective endocarditis: a 1-year population-based survey. Clin Infect Dis. 2012; 54:1230–1239.
Article11. Choi EN, Kwon JH, Choi KM, Hwang HD, Sin KM, Choi JY, et al. A clinical study of infective endocarditis in childhood. Korean J Pediatr. 2004; 47:844–850.12. Knudsen JB, Fuursted K, Petersen E, Wierup P, Molgaard H, Poulsen SH, et al. Infective endocarditis: a continuous challenge. The recent experience of a European tertiary center. J Heart Valve Dis. 2009; 18:386–394.13. Saiman L, Prince A, Gersony WM. Pediatric infective endocarditis in the modern era. J Pediatr. 1993; 122:847–853.
Article14. Baltimore RS, Gewitz M, Baddour LM, Beerman LB, Jackson MA, Lockhart PB, et al. Infective endocarditis in childhood: 2015 update: a scientific statement from the American Heart Association. Circulation. 2015; 132:1487–1515.15. Awadallah SM, Kavey RE, Byrum CJ, Smith FC, Kveselis DA, Blackman MS. The changing pattern of infective endocarditis in childhood. Am J Cardiol. 1991; 68:90–94.
Article16. Wilson W, Taubert KA, Gewitz M, Lockhart PB, Baddour LM, Levison M, et al. Prevention of infective endocarditis: guidelines from the American Heart Association: a guideline from the American Heart Association Rheumatic Fever, Endocarditis, and Kawasaki Disease Committee, Council on Cardiovascular Disease in the Young, and the Council on Clinical Cardiology, Council on Cardiovascular Surgery and Anesthesia, and the Quality of Care and Outcomes Research Interdisciplinary Working Group. Circulation. 2007; 116:1736–1754.17. Lucas VS, Omar J, Vieira A, Roberts GJ. The relationship between odontogenic bacteraemia and orthodontic treatment procedures. Eur J Orthod. 2002; 24:293–301.
Article18. American Academy of Pediatrics Committee on Infectious Diseases. Staphylococcal infections. In : Pickering LK, Baker CJ, Kimberlin DW, Long SS, editors. Red book: 2012 report of the committee on infectious diseases. 29th ed. EIK Groove Village: American Academy of Pediatrics;2012. p. 653–667.19. Pant S, Patel NJ, Deshmukh A, Golwala H, Patel N, Badheka A, et al. Trends in infective endocarditis incidence, microbiology, and valve replacement in the United States from 2000 to 2011. J Am Coll Cardiol. 2015; 65:2070–2076.
Article20. Baddour LM, Wilson WR, Bayer AS, Fowler VG Jr, Tleyjeh IM, Rybak MJ, et al. Infective endocarditis in adults: diagnosis, antimicrobial therapy, and management of complications: a scientific statement for healthcare professionals from the American Heart Association. Circulation. 2015; 132:1435–1486.
Article21. Duval X, Iung B, Klein I, Brochet E, Thabut G, Arnoult F, et al. Effect of early cerebral magnetic resonance imaging on clinical decisions in infective endocarditis: a prospective study. Ann Intern Med. 2010; 152:497–504.
Article22. Aguilar J, Urday-Cornejo V, Donabedian S, Perri M, Tibbetts R, Zervos M. Staphylococcus aureus meningitis: case series and literature review. Medicine (Baltimore). 2010; 89:117–125.23. Sonneville R, Mourvillier B, Bouadma L, Wolff M. Management of neurological complications of infective endocarditis in ICU patients. Ann Intensive Care. 2011; 1:10.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Fatal Case of Infective Endocarditis Caused by Community-Associated Methicillin-Resistant Staphylococcus aureus ST72 in Korea
- A case of multiple furunculosis caused by methicillin-resistant staphylococcs aureus
- Detection of Multidrug Resistant Patterns and Associated - genes of Methicillin Resistant Staphylococcus aureus ( MRSA ) Isolated from Clinical Specimens
- Methicillin-resistant Staphylococcus aureus Endocarditis after Sigmoidoscopy
- A statistical analysis of methicillin-resistant staphylococcus aureus