Korean J Radiol.
2016 Apr;17(2):281-288. 10.3348/kjr.2016.17.2.281.
F-18 Sodium Fluoride Positron Emission Tomography/Computed Tomography for Detection of Thyroid Cancer Bone Metastasis Compared with Bone Scintigraphy
- Affiliations
-
- 1Department of Nuclear Medicine, Seoul National University Bundang Hospital, Seoul National University College of Medicine, Seoul 13620, Korea. wwlee@snu.ac.kr
- 2World Class University, Department of Molecular Medicine and Biopharmaceutical Science, Graduate School of Convergence Science and Technology, Seoul National University, Seoul 03080, Korea.
- 3Institute of Radiation Medicine, Medical Research Center, Seoul National University, Seoul 03087, Korea.
- 4Department of Pathology, Seoul National University Bundang Hospital, Seoul National University College of Medicine, Seoul 13620, Korea.
- KMID: 2360215
- DOI: http://doi.org/10.3348/kjr.2016.17.2.281
Abstract
OBJECTIVE
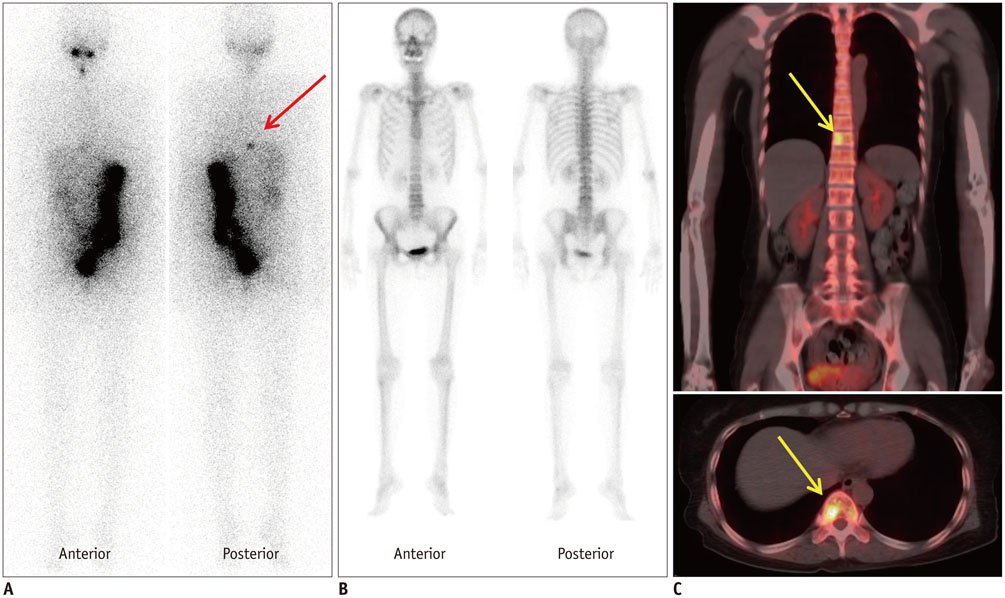
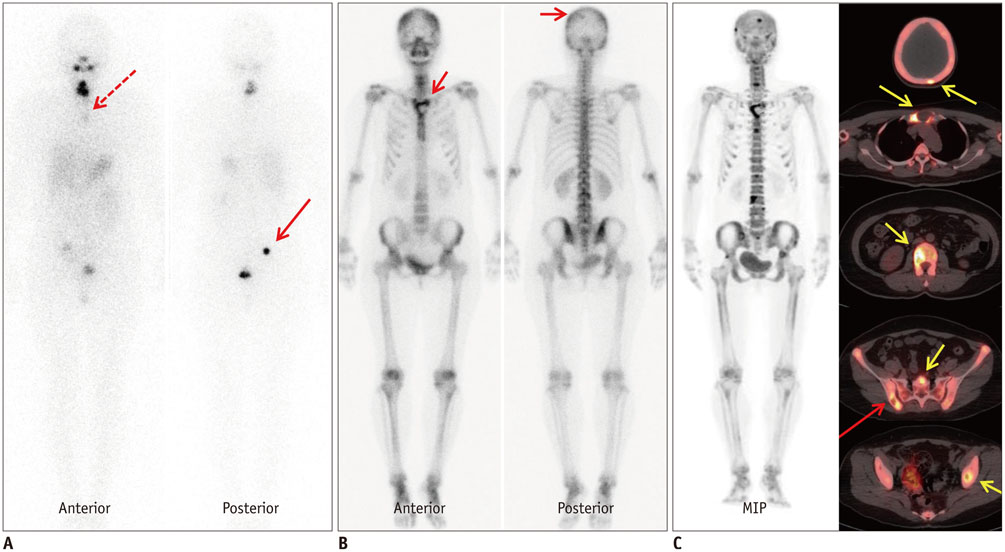
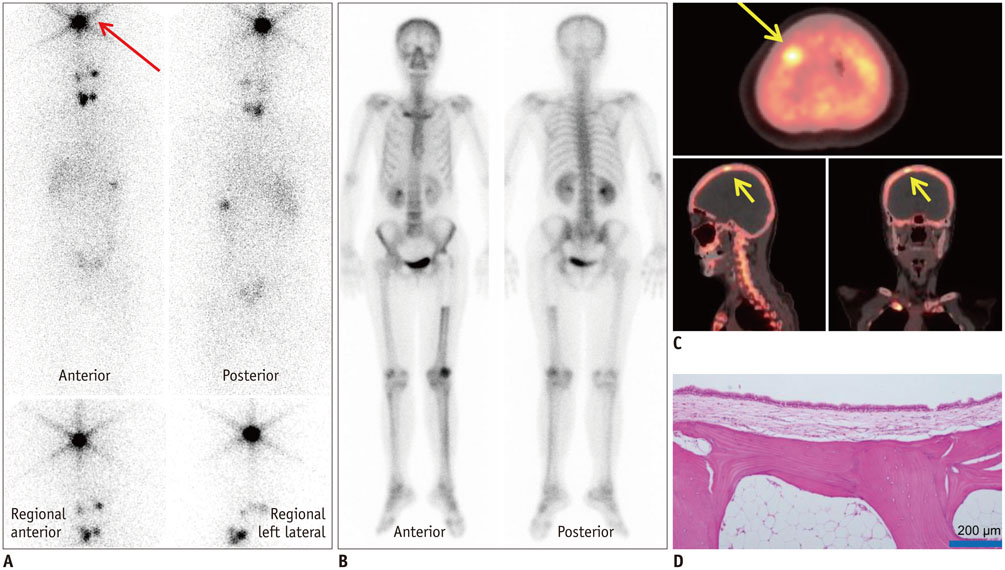
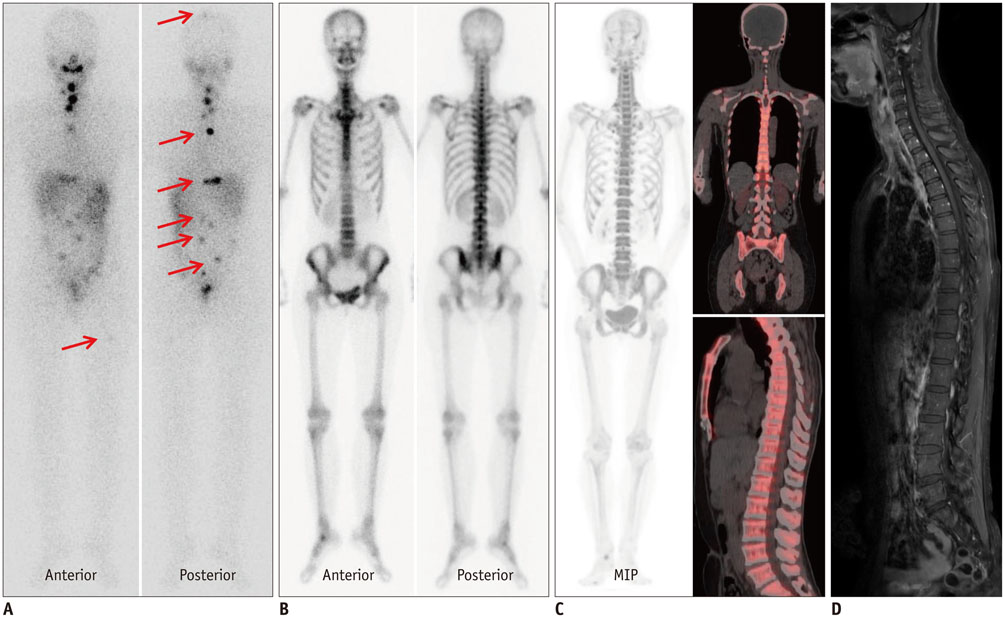
The aim of the study was to compare the diagnostic performances of F-18 sodium fluoride positron emission tomography/computed tomography (bone PET/CT) and bone scintigraphy (BS) for the detection of thyroid cancer bone metastasis.
MATERIALS AND METHODS
We retrospectively enrolled 6 thyroid cancer patients (age = 44.7 ± 9.8 years, M:F = 1:5, papillary:follicular = 2:4) with suspected bone metastatic lesions in the whole body iodine scintigraphy or BS, who subsequently underwent bone PET/CT. Pathologic diagnosis was conducted for 4 lesions of 4 patients.
RESULTS
Of the 17 suspected bone lesions, 10 were metastatic and 7 benign. Compared to BS, bone PET/CT exhibited superior sensitivity (10/10 = 100% vs. 2/10 = 20%, p = 0.008), and accuracy (14/17 = 82.4% vs. 7/17 = 41.2%, p < 0.025). The specificity (4/7 = 57.1%) of bone PET/CT was not significantly different from that of BS (5/7 = 71.4%, p > 0.05).
CONCLUSION
Bone PET/CT may be more sensitive and accurate than BS for the detection of thyroid cancer bone metastasis.
Keyword
MeSH Terms
-
Adult
Bone Neoplasms/*radiography/secondary
Bone and Bones/*radiography
Contrast Media/*chemistry
Female
Fluorine Radioisotopes/chemistry
Humans
Male
Middle Aged
Positron-Emission Tomography
Retrospective Studies
Sodium Fluoride/*chemistry
Thyroid Neoplasms/*pathology
Tomography, X-Ray Computed
Whole Body Imaging
Contrast Media
Fluorine Radioisotopes
Sodium Fluoride
Figure
Reference
-
1. American Thyroid Association (ATA) Guidelines Taskforce on Thyroid Nodules and Differentiated Thyroid Cancer. Cooper DS, Doherty GM, Haugen BR, Kloos RT, Lee SL, et al. Revised American Thyroid Association management guidelines for patients with thyroid nodules and differentiated thyroid cancer. Thyroid. 2009; 19:1167–1214.2. Sampson E, Brierley JD, Le LW, Rotstein L, Tsang RW. Clinical management and outcome of papillary and follicular (differentiated) thyroid cancer presenting with distant metastasis at diagnosis. Cancer. 2007; 110:1451–1456.3. Schlumberger M, Tubiana M, De Vathaire F, Hill C, Gardet P, Travagli JP, et al. Long-term results of treatment of 283 patients with lung and bone metastases from differentiated thyroid carcinoma. J Clin Endocrinol Metab. 1986; 63:960–967.4. Brown AP, Greening WP, McCready VR, Shaw HJ, Harmer CL. Radioiodine treatment of metastatic thyroid carcinoma: the Royal Marsden Hospital experience. Br J Radiol. 1984; 57:323–327.5. Durante C, Haddy N, Baudin E, Leboulleux S, Hartl D, Travagli JP, et al. Long-term outcome of 444 patients with distant metastases from papillary and follicular thyroid carcinoma: benefits and limits of radioiodine therapy. J Clin Endocrinol Metab. 2006; 91:2892–2899.6. Davila D, Antoniou A, Chaudhry MA. Evaluation of osseous metastasis in bone scintigraphy. Semin Nucl Med. 2015; 45:3–15.7. Ito S, Kato K, Ikeda M, Iwano S, Makino N, Tadokoro M, et al. Comparison of 18F-FDG PET and bone scintigraphy in detection of bone metastases of thyroid cancer. J Nucl Med. 2007; 48:889–895.8. Qiu ZL, Xue YL, Song HJ, Luo QY. Comparison of the diagnostic and prognostic values of 99mTc-MDP-planar bone scintigraphy, 131I-SPECT/CT and 18F-FDG-PET/CT for the detection of bone metastases from differentiated thyroid cancer. Nucl Med Commun. 2012; 33:1232–1242.9. Kang JY, Lee WW, So Y, Lee BC, Kim SE. Clinical Usefulness of (18)F-fluoride Bone PET. Nucl Med Mol Imaging. 2010; 44:55–61.10. Yoon SH, Kim KS, Kang SY, Song HS, Jo KS, Choi BH, et al. Usefulness of (18)F-fluoride PET/CT in Breast Cancer Patients with Osteosclerotic Bone Metastases. Nucl Med Mol Imaging. 2013; 47:27–35.11. Grant FD, Fahey FH, Packard AB, Davis RT, Alavi A, Treves ST. Skeletal PET with 18F-fluoride: applying new technology to an old tracer. J Nucl Med. 2008; 49:68–78.12. Schirrmeister H, Buck A, Guhlmann A, Reske SN. Anatomical distribution and sclerotic activity of bone metastases from thyroid cancer assessed with F-18 sodium fluoride positron emission tomography. Thyroid. 2001; 11:677–683.13. Ota N, Kato K, Iwano S, Ito S, Abe S, Fujita N, et al. Comparison of 18F-fluoride PET/CT, 18F-FDG PET/CT and bone scintigraphy (planar and SPECT) in detection of bone metastases of differentiated thyroid cancer: a pilot study. Br J Radiol. 2014; 87:20130444.14. Lee SJ, Lee WW, Kim SE. Bone positron emission tomography with or without CT is more accurate than bone scan for detection of bone metastasis. Korean J Radiol. 2013; 14:510–519.15. Wolff H, Breda DJ, Da Silva N, Hartmann AA. False-positive I-131 deposition in a parotid gland duct ectasia. Clin Nucl Med. 1998; 23:257–259.16. Agriantonis DJ, Hall L, Wilson MA. Pitfalls of I-131 whole body scan interpretation: bronchogenic cyst and mucinous cystadenoma. Clin Nucl Med. 2008; 33:325–327.17. Buton L, Morel O, Gault P, Illouz F, Rodien P, Rohmer V. False-positive iodine-131 whole-body scan findings in patients with differentiated thyroid carcinoma: report of 11 cases and review of the literature. Ann Endocrinol (Paris). 2013; 74:221–230.18. Oh JR, Byun BH, Hong SP, Chong A, Kim J, Yoo SW, et al. Comparison of 131I whole-body imaging, 131I SPECT/CT, and 18F-FDG PET/CT in the detection of metastatic thyroid cancer. Eur J Nucl Med Mol Imaging. 2011; 38:1459–1468.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Early Evaluation of Inflammatory Focus and Treatment Response Using ¹â¸F-Sodium Fluoride Bone Positron Emission Tomography/Computed Tomography in Patients with Metallic Implants: A Case Report
- Unusual Soft Tissue Uptake of F-18 Sodium Fluoride in Three Patients Undergoing F-18 NaF PET/CT Bone Scans for Prostate Cancer
- Transient ¹â¸F-Fluorodeoxyglucose Activity on PET/CT of Herniation Pit in Thyroid Cancer Patient: A Case Report
- Bone Positron Emission Tomography with or without CT Is More Accurate than Bone Scan for Detection of Bone Metastasis
- Bone and Calcified Soft Tissue Metastases of Medullary Thyroid Carcinoma Better Characterized on ¹â¸F-Fluoride PET/CT than on â¶â¸Ga-Dotatate PET/CT