Diagnosis of inflammatory bowel disease in Asia: the results of a multinational web-based survey in the 2nd Asian Organization for Crohn's and Colitis (AOCC) meeting in Seoul
- Affiliations
-
- 1Department of Internal Medicine, Kyungpook National University School of Medicine, Daegu, Korea.
- 2The First Affiliated Hospital of San Yat-Sen University, Guangzhou, China. chenminhu@vip.163.com
- 3Department of Internal Medicine, Chosun University College of Medicine, Gwangju, Korea.
- 4Department of Internal Medicine, Kyung Hee University College of Medicine, Seoul, Korea.
- 5Department of Internal Medicine, Seoul Paik Hospital, Inje University College of Medicine, Seoul, Korea.
- KMID: 2354964
- DOI: http://doi.org/10.5217/ir.2016.14.3.224
Abstract
- BACKGROUND/AIMS
As the number of Asian patients with inflammatory bowel disease (IBD) has increased recently, there is a growing need to improve IBD care in this region. This study is aimed at determining how Asian countries are currently dealing with their IBD patients in terms of diagnosis.
METHODS
A questionnaire was designed by the organizing committee of Asian Organization for Crohn's and Colitis, for a multinational web-based survey conducted between March 2014 and May 2014.
RESULTS
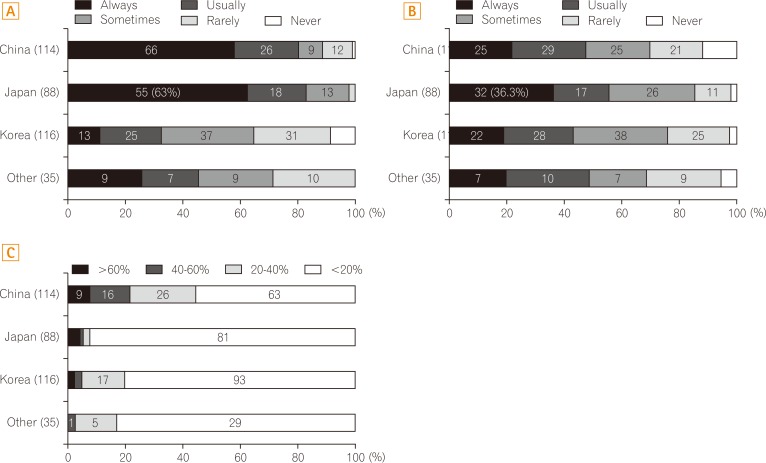
A total of 353 Asian medical doctors treating IBD patients responded to the survey (114 in China, 88 in Japan, 116 in Korea, and 35 in other Asian countries). Most of the respondents were gastroenterologists working in an academic teaching hospital. While most of the doctors from China, Japan, and Korea use their own national guidelines for IBD diagnosis, those from other Asian countries most commonly adopt the European Crohn's Colitis Organisation's guideline. Japanese doctors seldom adopt the Montreal classification for IBD. The most commonly used activity scoring system for ulcerative colitis is the Mayo score in all countries except China, whereas that for Crohn's disease (CD) is the Crohn's Disease Activity Index. The most available tool for small-bowel evaluation in CD patients differs across countries. Many physicians administer empirical anti-tuberculous medications before the diagnosis of CD.
CONCLUSIONS
The results of this survey demonstrate that Asian medical doctors have different diagnostic approaches for IBD. This knowledge would be important in establishing guidelines for improving the care of IBD patients in this region.
Keyword
MeSH Terms
Figure
Cited by 6 articles
-
Optimal diagnosis and disease activity monitoring of intestinal Behçet's disease
Hyun Jung Lee, Jae Hee Cheon
Intest Res. 2017;15(3):311-317. doi: 10.5217/ir.2017.15.3.311.Results of the first survey for the current status of inflammatory bowel disease management in Asian countries
Ji Won Kim
Intest Res. 2016;14(3):199-201. doi: 10.5217/ir.2016.14.3.199.Vaccination in patients with inflammatory bowel disease–Asian perspectives: the results of a multinational web-based survey in the 8th Asian Organization for Crohn’s and Colitis meeting
Su Bum Park, Kyeong Ok Kim, Hong Sub Lee, Chang Hwan Choi, Shu Chen Wei, Min Hu Chen, Katsuyoshi Matsuoka
Intest Res. 2023;21(3):363-374. doi: 10.5217/ir.2023.00015.Diagnosis of inflammatory bowel disease–Asian perspectives: the results of a multinational web-based survey in the 8th Asian Organization for Crohn’s and Colitis meeting
Han Hee Lee, Jae Jun Park, Bo-In Lee, Ida Hilmi, Jose Sollano, Zhi Hua Ran
Intest Res. 2023;21(3):328-338. doi: 10.5217/ir.2023.00012.Infectious complications in patients with inflammatory bowel disease in Asia: the results of a multinational web-based survey in the 8th Asian Organization for Crohn’s and Colitis meeting
Yu Kyung Jun, Seong-Joon Koh, Dae Seong Myung, Sang Hyoung Park, Choon Jin Ooi, Ajit Sood, Jong Pil Im
Intest Res. 2023;21(3):353-362. doi: 10.5217/ir.2023.00013.Treatment of inflammatory bowel disease–Asian perspectives: the results of a multinational web-based survey in the 8th Asian Organization for Crohn’s and Colitis meeting
Eun Mi Song, Soo-Young Na, Sung Noh Hong, Siew Chien Ng, Tadakazu Hisamatsu, Byong Duk Ye
Intest Res. 2023;21(3):339-352. doi: 10.5217/ir.2022.00135.
Reference
-
1. Baumgart DC, Carding SR. Inflammatory bowel disease: cause and immunobiology. Lancet. 2007; 369:1627–1640. PMID: 17499605.
Article2. Yang SK, Yun S, Kim JH, et al. Epidemiology of inflammatory bowel disease in the Songpa-Kangdong district, Seoul, Korea, 1986-2005: a KASID study. Inflamm Bowel Dis. 2008; 14:542–549. PMID: 17941073.
Article3. Ng SC, Bernstein CN, Vatn MH, et al. Geographical variability and environmental risk factors in inflammatory bowel disease. Gut. 2013; 62:630–649. PMID: 23335431.
Article4. Kim ES, Kim WH. Inflammatory bowel disease in Korea: epidemiological, genomic, clinical, and therapeutic characteristics. Gut Liver. 2010; 4:1–14. PMID: 20479907.
Article5. Ye BD, Jang BI, Jeen YT, et al. Diagnostic guideline of Crohn's disease. Korean J Gastroenterol. 2009; 53:161–176. PMID: 19835218.6. Choi CH, Jung SA, Lee BI, et al. Diagnostic guideline of ulcerative colitis. Korean J Gastroenterol. 2009; 53:145–160. PMID: 19835217.7. Ueno F, Matsui T, Matsumoto T, et al. Evidence-based clinical practice guidelines for Crohn's disease, integrated with formal consensus of experts in Japan. J Gastroenterol. 2013; 48:31–72. PMID: 23090001.
Article8. Chinese Cooperative Group For The Study On IBD. Chinese Society Of Gastroenterology. Ouyang Q, et al. Consensus on the management of inflammatory bowel disease in China in 2007. J Dig Dis. 2008; 9:52–62. PMID: 18251795.
Article9. Truelove SC, Witts LJ. Cortisone in ulcerative colitis; final report on a therapeutic trial. Br Med J. 1955; 2:1041–1048. PMID: 13260656.10. Schroeder KW, Tremaine WJ, Ilstrup DM. Coated oral 5-aminosalicylic acid therapy for mildly to moderately active ulcerative colitis. A randomized study. N Engl J Med. 1987; 317:1625–1629. PMID: 3317057.
Article11. Sands BE, Ooi CJ. A survey of methodological variation in the Crohn's disease activity index. Inflamm Bowel Dis. 2005; 11:133–138. PMID: 15677906.
Article12. Annese V, Daperno M, Rutter MD, et al. European evidence based consensus for endoscopy in inflammatory bowel disease. J Crohns Colitis. 2013; 7:982–1018. PMID: 24184171.
Article13. Travis SP, Schnell D, Krzeski P, et al. Developing an instrument to assess the endoscopic severity of ulcerative colitis: the Ulcerative Colitis Endoscopic Index of Severity (UCEIS). Gut. 2012; 61:535–542. PMID: 21997563.
Article14. Samuel S, Bruining DH, Loftus EV Jr, et al. Validation of the ulcerative colitis colonoscopic index of severity and its correlation with disease activity measures. Clin Gastroenterol Hepatol. 2013; 11:49–54. PMID: 22902762.
Article15. Travis SP, Schnell D, Krzeski P, et al. Reliability and initial validation of the ulcerative colitis endoscopic index of severity. Gastroenterology. 2013; 145:987–995. PMID: 23891974.
Article16. Reddy SS, Brandt LJ. Clostridium difficile infection and inflammatory bowel disease. J Clin Gastroenterol. 2013; 47:666–671. PMID: 23507767.17. Singh S, Graff LA, Bernstein CN. Do NSAIDs, antibiotics, infections, or stress trigger flares in IBD? Am J Gastroenterol. 2009; 104:1298–1313. PMID: 19337242.
Article18. Larsson G, Shenoy T, Ramasubramanian R, et al. Routine diagnosis of intestinal tuberculosis and Crohn's disease in Southern India. World J Gastroenterol. 2014; 20:5017–5024. PMID: 24803814.
Article19. Li Y, Zhang LF, Liu XQ, et al. The role of in vitro interferongamma-release assay in differentiating intestinal tuberculosis from Crohn's disease in China. J Crohns Colitis. 2012; 6:317–323. PMID: 22405168.
Article20. Almadi MA, Ghosh S, Aljebreen AM. Differentiating intestinal tuberculosis from Crohn's disease: a diagnostic challenge. Am J Gastroenterol. 2009; 104:1003–1012. PMID: 19240705.
Article21. Zhao XS, Wang ZT, Wu ZY, et al. Differentiation of Crohn's disease from intestinal tuberculosis by clinical and CT enterographic models. Inflamm Bowel Dis. 2014; 20:916–925. PMID: 24694791.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Treatment of inflammatory bowel disease in Asia: the results of a multinational web-based survey in the 2nd Asian Organization of Crohn's and Colitis (AOCC) meeting in Seoul
- Diagnosis of inflammatory bowel disease–Asian perspectives: the results of a multinational web-based survey in the 8th Asian Organization for Crohn’s and Colitis meeting
- Erratum: Treatment of inflammatory bowel disease in Asia: the results of a multinational web-based survey in the 2(nd) Asian Organization for Crohn's and Colitis (AOCC) meeting in Seoul
- Quality of care in inflammatory bowel disease in Asia: the results of a multinational web-based survey in the 2nd Asian Organization of Crohn's and Colitis (AOCC) meeting in Seoul
- Treatment of inflammatory bowel disease–Asian perspectives: the results of a multinational web-based survey in the 8th Asian Organization for Crohn’s and Colitis meeting