Blood Res.
2016 Sep;51(3):200-203. 10.5045/br.2016.51.3.200.
Changes in serum uric acid levels after allogeneic hematologic stem cell transplantation: A retrospective cohort study
- Affiliations
-
- 1Division of Rheumatology, Department of Internal Medicine, Seoul National University Hospital, Seoul, Korea.
- 2Department of Molecular Medicine and Biopharmaceutical Sciences, Graduate School of Convergence Science and Technology, and College of Medicine, Medical Research Institute, Seoul National University, Seoul, Korea.
- 3Division of Hematology and Oncology, Department of Internal Medicine, Seoul National University Hospital, Seoul, Korea. ssysmc@snu.ac.kr
- 4Cancer Research Institute, Seoul National University College of Medicine, Seoul, Korea.
- 5Biomedical Research Institute, Seoul National University Hospital, Seoul, Korea.
- KMID: 2353502
- DOI: http://doi.org/10.5045/br.2016.51.3.200
Abstract
- BACKGROUND
Since cell turnover in the hematopoietic system constitutes a major source of uric acid (UA) production, we investigated whether hematopoietic stem cell transplantation (HSCT) is associated with significant changes in serum UA levels in patients with hematological disorders.
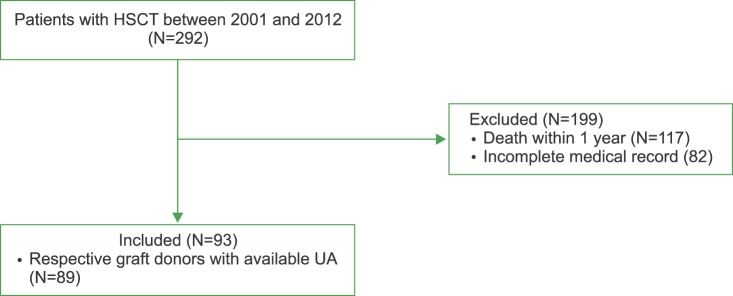
METHODS
Patients who underwent HSCT at our institution between 2001 and 2012 were retrospectively enrolled. Serum UA levels at 3 months before, 1 week before, and 3 months and 1 year after HSCT were examined.
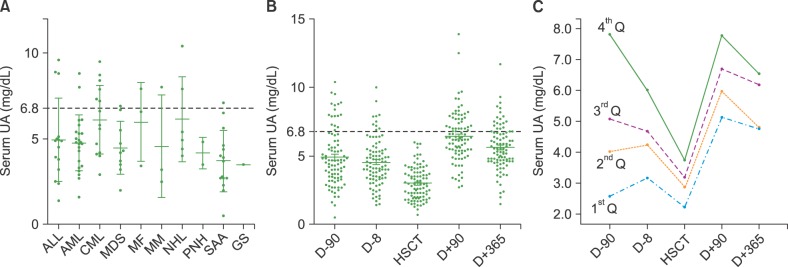
RESULTS
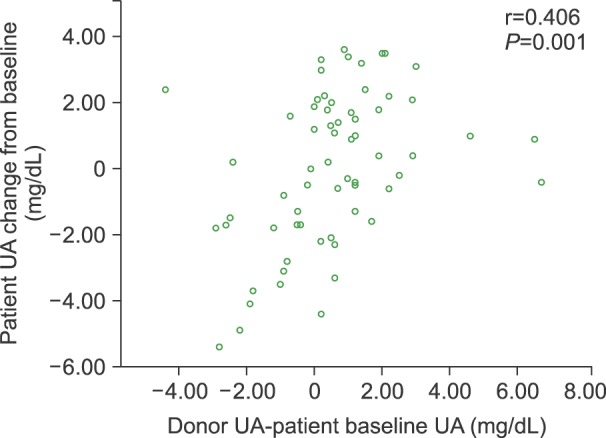
Complete clinical and laboratory information including data regarding UA levels was available for 93 patients. At baseline, the mean UA level was 4.9±2.1 mg/dL, with an overall prevalence of hyperuricemia of 15% (defined as serum UA>6.8 mg/dL). Mean UA levels tended to be higher in patients with acute myeloid leukemia (4.8±2.0 mg/dL) and non-Hodgkin lymphoma (5.1±2.3 mg/dL) and lower in patients with aplastic anemia (mean, 4.2±1.8 mg/dL). UA levels dropped during myeloablative conditioning, reaching a nadir on the day of HSCT (3.27±1.4 mg/dL). Over the 3 months following HSCT, UA levels rose sharply (5.0±2.1 mg/dL) and remained stable up to 1 year after HSCT (5.5±1.6 mg/dL). UA levels in HSCT recipients at 12 months correlated with those of their respective graft donors (Pearson r=0.406, P=0.001).
CONCLUSION
HSCT is associated with significant changes in uric acid levels in patients with hematologic disorders.
MeSH Terms
Figure
Reference
-
1. Hediger MA, Johnson RJ, Miyazaki H, Endou H. Molecular physiology of urate transport. Physiology (Bethesda). 2005; 20:125–133. PMID: 15772301.
Article2. Kamble RT, Guo S, Ramos CA, Carrum G. Acute gout at engraftment following hematopoietic transplantation. Am J Hematol. 2011; 86:961–962. PMID: 21948346.
Article3. Yamauchi T, Negoro E, Lee S, et al. A high serum uric acid level is associated with poor prognosis in patients with acute myeloid leukemia. Anticancer Res. 2013; 33:3947–3951. PMID: 24023333.4. Carpenter PA, Ziegler JB, Vowels MR. Late diagnosis and correction of purine nucleoside phosphorylase deficiency with allogeneic bone marrow transplantation. Bone Marrow Transplant. 1996; 17:121–124. PMID: 8673045.5. Zegers BJ, Stoop JW, Staal GE, Wadman SK. An approach to the restoration of T cell function in a purine nucleoside phosphorylase deficient patient. Ciba Found Symp. 1978; 68:231–253. PMID: 115663.
Article6. Cannell PK, Herrmann RP. Urate metabolism during bone marrow transplantation. Bone Marrow Transplant. 1992; 10:337–339. PMID: 1422489.7. Rieselbach RE, Bentzel CJ, Cotlove E, Frei E 3rd, Freireich EJ. Uric acid excretion and renal function in the acute hyperuricemia of leukemia. Pathogenesis and therapy of uric acid nephropathy. Am J Med. 1964; 37:872–883. PMID: 14246089.8. Shulman H, Striker G, Deeg HJ, Kennedy M, Storb R, Thomas ED. Nephrotoxicity of cyclosporin A after allogeneic marrow transplantation: glomerular thromboses and tubular injury. N Engl J Med. 1981; 305:1392–1395. PMID: 7029278.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Serum Uric Acid and Metabolic Syndrome: a Retrospective Cohort Study
- Four-Year Change of Metabolic Syndrome Incidence According to Serum Uric Acid
- Two Cases of Generalized Vitiligo after Allogeneic Stem Cell Transplantation
- Serum Hepcidin Level as an Early Marker of Hematopoietic Activity after Allogeneic Peripheral Blood Stem Cell Transplantation
- A case of pneumomediastinum combined with chronic graft-versus-host disease following allogeneic hematopoietic stem cell transplantation