J Korean Neurosurg Soc.
2014 Sep;56(3):237-242. 10.3340/jkns.2014.56.3.237.
Microsurgical Treatment and Outcome of Pediatric Supratentorial Cerebral Cavernous Malformation
- Affiliations
-
- 1Department of Neurosurgery, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea. shinhj@skku.edu
- KMID: 2339963
- DOI: http://doi.org/10.3340/jkns.2014.56.3.237
Abstract
OBJECTIVE
The purpose of this study was to investigate the clinical features and outcomes of pediatric cavernous malformation (CM) in the central nervous system.
METHODS
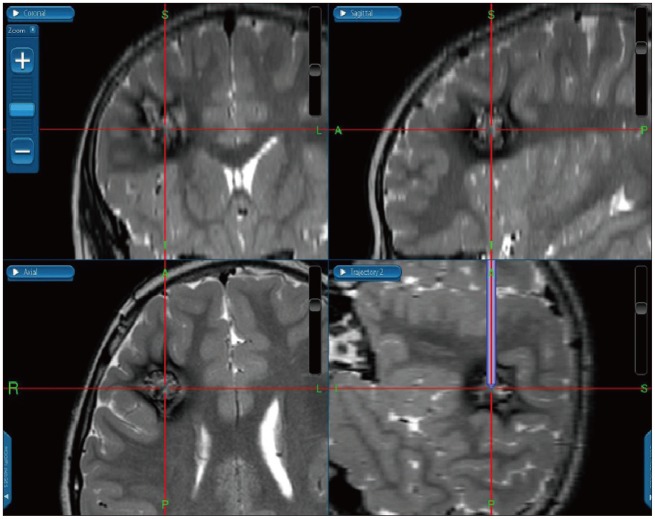
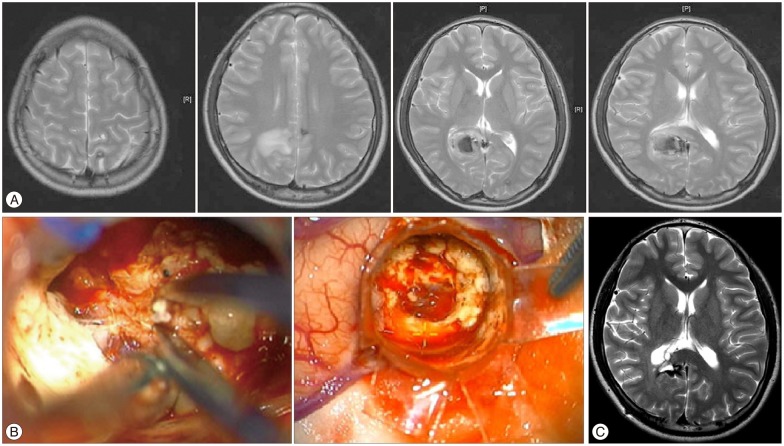
Twenty-nine pediatric patients with supratentorial CM underwent microsurgical excision. In selected cases, transparent tubular retractor system (TTRS) was used to reduce retraction injury and intraoperative neuromonitoring (IONM) was held to preserve functioning cortex. Patients' demographics and symptoms were reviewed and surgical outcomes were discussed.
RESULTS
The main initial clinical manifestations included the following : seizures (n=13, 45%), headache (n=7, 24%), focal neurological deficits (n=3, 10%), and an incidental finding (n=6, 21%). Overt hemorrhage was detected in 7 patients (24%). There were 19 children (66%) with a single CM and 10 (34%) children with multiple CMs. In 7 cases with deep-seated CM, we used a TTRS to minimize retraction. In 9 cases which location of CM was at eloquent area, IONM was taken during surgery. There was no major morbidity or mortality after surgery. In the 29 operated children, the overall long-term results were satisfactory : 25 (86%) patients had no signs or symptoms associated with CMs, 3 had controllable seizures, and 1 had mild weakness.
CONCLUSION
With the assistance of neuronavigation systems, intraoperative neuromonitoring, and TTRS, CMs could be targeted more accurately and excised more safely. Based on the satisfactory seizure outcome achieved, complete microsurgical excision in children is recommended for CMs presenting with seizures but removal of hemosiderin-stained areas seems to be unnecessary.
MeSH Terms
Figure
Reference
-
1. Acciarri N, Galassi E, Giulioni M, Pozzati E, Grasso V, Palandri G, et al. Cavernous malformations of the central nervous system in the pediatric age group. Pediatr Neurosurg. 2009; 45:81–104. PMID: 19307743.
Article2. Aiba T, Tanaka R, Koike T, Kameyama S, Takeda N, Komata T. Natural history of intracranial cavernous malformations. J Neurosurg. 1995; 83:56–59. PMID: 7782850.
Article3. Baumann CR, Acciarri N, Bertalanffy H, Devinsky O, Elger CE, Lo Russo G, et al. Seizure outcome after resection of supratentorial cavernous malformations : a study of 168 patients. Epilepsia. 2007; 48:559–563. PMID: 17346251.
Article4. Baumann CR, Schuknecht B, Lo Russo G, Cossu M, Citterio A, Andermann F, et al. Seizure outcome after resection of cavernous malformations is better when surrounding hemosiderin-stained brain also is removed. Epilepsia. 2006; 47:563–566. PMID: 16529622.
Article5. Casazza M, Broggi G, Franzini A, Avanzini G, Spreafico R, Bracchi M, et al. Supratentorial cavernous angiomas and epileptic seizures : preoperative course and postoperative outcome. Neurosurgery. 1996; 39:26–32. discussion 32-34. PMID: 8805137.6. Cohen-Gadol AA, Jacob JT, Edwards DA, Krauss WE. Coexistence of intracranial and spinal cavernous malformations : a study of prevalence and natural history. J Neurosurg. 2006; 104:376–381. PMID: 16572649.
Article7. Del Curling O Jr, Kelly DL Jr, Elster AD, Craven TE. An analysis of the natural history of cavernous angiomas. J Neurosurg. 1991; 75:702–708. PMID: 1919691.
Article8. Di Rocco C, Iannelli A, Tamburrini G. Cavernomas of the central nervous system in children. A report of 22 cases. Acta Neurochir (Wien). 1996; 138:1267–1274. discussion 1273-1274. PMID: 8980728.9. Engel J Jr, Levesque MF, Shields WD. Surgical treatment of the epilepsies : presurgical evaluation. Clin Neurosurg. 1992; 38:514–534. PMID: 1537201.10. Ferroli P, Casazza M, Marras C, Mendola C, Franzini A, Broggi G. Cerebral cavernomas and seizures : a retrospective study on 163 patients who underwent pure lesionectomy. Neurol Sci. 2006; 26:390–394. PMID: 16601930.
Article11. Herter T, Brandt M, Szüwart U. Cavernous hemangiomas in children. Childs Nerv Syst. 1988; 4:123–127. PMID: 3396017.
Article12. Hsu F, Rigamonti D, Huhn SL. Epidemiology of cavernous malformations. In : Awad IA, Barrow DL, editors. Cavernous malformations. Park Ridge: American Association of Neurological Surgeons;1993. p. 13–23.13. Jo KI, Chung SB, Jo KW, Kong DS, Seol HJ, Shin HJ. Microsurgical resection of deep-seated lesions using transparent tubular retractor : pediatric case series. Childs Nerv Syst. 2011; 27:1989–1994. PMID: 21779977.
Article14. Johnston MV. Clinical disorders of brain plasticity. Brain Dev. 2004; 26:73–80. PMID: 15036425.
Article15. Kawagishi J, Suzuki M, Kayama T, Yoshimoto T. Huge multilobular cavernous angioma in an infant : case report. Neurosurgery. 1993; 32:1028–1030. discussion 1030-1031. PMID: 8327078.16. Lena G, Ternier J, Paz-Paredes A, Scavarda D. [Central nervous system cavernomas in children]. Neurochirurgie. 2007; 53(2-3 Pt 2):223–237. PMID: 17507057.17. Mazza C, Scienza R, Beltramello A, Da Pian R. Cerebral cavernous malformations (cavernomas) in the pediatric age-group. Childs Nerv Syst. 1991; 7:139–146. PMID: 1878867.
Article18. Moriarity JL, Wetzel M, Clatterbuck RE, Javedan S, Sheppard JM, Hoenig-Rigamonti K, et al. The natural history of cavernous malformations : a prospective study of 68 patients. Neurosurgery. 1999; 44:1166–1171. discussion 1172-1173. PMID: 10371615.
Article19. Mottolese C, Hermier M, Stan H, Jouvet A, Saint-Pierre G, Froment JC, et al. Central nervous system cavernomas in the pediatric age group. Neurosurg Rev. 2001; 24:55–71. discussion 72-73. PMID: 11485241.
Article20. Papadias A, Taha A, Sgouros S, Walsh AR, Hockley AD. Incidence of vascular malformations in spontaneous intra-cerebral haemorrhage in children. Childs Nerv Syst. 2007; 23:881–886. PMID: 17450369.
Article21. Pozzati E, Giuliani G, Nuzzo G, Poppi M. The growth of cerebral cavernous angiomas. Neurosurgery. 1989; 25:92–97. PMID: 2755587.
Article22. Robinson JR, Awad IA. Clinical spectrum and natural course. In : Awad IA, Barrow DL, editors. Cavernous malformations. Park Ridge: American Association of Neurological Surgeons;1993. p. 25–36.23. Robinson JR, Awad IA, Little JR. Natural history of the cavernous angioma. J Neurosurg. 1991; 75:709–714. PMID: 1919692.
Article24. Robinson JR Jr, Awad IA, Magdinec M, Paranandi L. Factors predisposing to clinical disability in patients with cavernous malformations of the brain. Neurosurgery. 1993; 32:730–735. discussion 735-736. PMID: 8492847.
Article25. Sakai N, Yamada H, Nishimura Y, Shirakami S, Futamura A, Andoh T. Intracranial cavernous angioma in the 1st year of life and a review of the literature. Childs Nerv Syst. 1992; 8:49–52. PMID: 1576609.
Article26. Ueda Y, Willmore LJ, Triggs WJ. Amygdalar injection of FeCl3 causes spontaneous recurrent seizures. Exp Neurol. 1998; 153:123–127. PMID: 9743573.27. Wang CC, Liu A, Zhang JT, Sun B, Zhao YL. Surgical management of brain-stem cavernous malformations : report of 137 cases. Surg Neurol. 2003; 59:444–454. discussion 454. PMID: 12826334.
Article28. Wang X, Tao Z, You C, Li Q, Liu Y. Extended resection of hemosiderin fringe is better for seizure outcome : a study in patients with cavernous malformation associated with refractory epilepsy. Neurol India. 2013; 61:288–292. PMID: 23860150.
Article29. Washington CW, McCoy KE, Zipfel GJ. Update on the natural history of cavernous malformations and factors predicting aggressive clinical presentation. Neurosurg Focus. 2010; 29:E7. PMID: 20809765.
Article30. Willmore LJ, Triggs WJ. Iron-induced lipid peroxidation and brain injury responses. Int J Dev Neurosci. 1991; 9:175–180. PMID: 2058418.
Article31. Wilson JT, Pettigrew LE, Teasdale GM. Structured interviews for the Glasgow Outcome Scale and the extended Glasgow Outcome Scale : guidelines for their use. J Neurotrauma. 1998; 15:573–585. PMID: 9726257.
Article32. Wostrack M, Shiban E, Harmening K, Obermueller T, Ringel F, Ryang YM, et al. Surgical treatment of symptomatic cerebral cavernous malformations in eloquent brain regions. Acta Neurochir (Wien). 2012; 154:1419–1430. PMID: 22739772.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Potential Risk of Radiation-Induced Cavernous Malformations Following Adjuvant Gamma Knife Radiosurgery for Mesial Temporal Lobe Epilepsy
- Cavernous Hemangioma on the Frontal Lobe
- Management of Intracranial Cavernous Malformation: A Retrospective Analysis of 76 Consecutive Cases
- Clinical Features and Treatment of Pediatric Cerebral Cavernous Malformations
- A case involving anesthesia for cesarean section followed by resection of ruptured cavernous malformation of pons :A case report