Anesth Pain Med.
2017 Jan;12(1):42-46. 10.17085/apm.2017.12.1.42.
A case involving anesthesia for cesarean section followed by resection of ruptured cavernous malformation of pons :A case report
- Affiliations
-
- 1Department of Anesthesiology and Pain Medicine, Dongtan Sacred Heart Hospital, Hallym University College of Medicine, Hwaseong, Korea. hardmong@naver.com
- KMID: 2369665
- DOI: http://doi.org/10.17085/apm.2017.12.1.42
Abstract
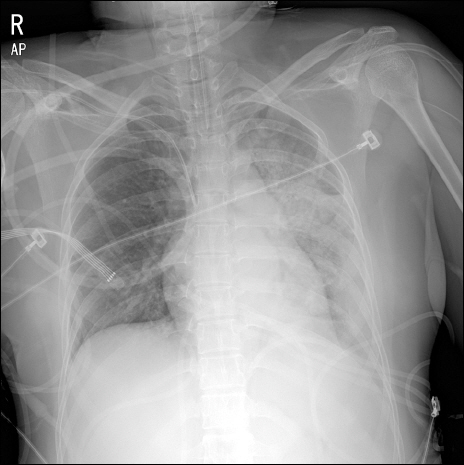
- Cavernous malformation is an important cause of cerebral hemorrhage in pregnant women. We experienced a case of cesarean section followed by neurosurgery for resection of ruptured cavernous malformation of pons in a 24-year-old pregnant woman. Establishing integrated treatment strategy for pregnant women with cavernous malformation is difficult because of the small number of cases. Therefore, the cooperation between the brain surgeon, anesthesiologist and obstetrician is essential when surgical intervention is needed. Despite aspiration pneumonia, the patient successfully underwent surgery. We reported this case along with a brief literature review.
MeSH Terms
Figure
Reference
-
1. Robinson JR, Awad IA, Little JR. Natural history of the cavernous angioma. J Neurosurg. 1991; 75:709–14. DOI: 10.3171/jns.1991.75.5.0709. PMID: 1919692.2. Kivelev J, Niemelä M, Hernesniemi J. Characteristics of cavernomas of the brain and spine. J Clin Neurosci. 2012; 19:643–8. DOI: 10.1016/j.jocn.2011.08.015. PMID: 22502911.3. Abla AA, Lekovic GP, Turner JD, de Oliveira JG, Porter R, Spetzler RF. Advances in the treatment and outcome of brainstem cavernous malformation surgery: a single-center case series of 300 surgically treated patients. Neurosurgery. 2011; 68:403–14. DOI: 10.1227/NEU.0b013e3181ff9cde. PMID: 21654575.4. Safavi-Abbasi S, Feiz-Erfan I, Spetzler RF, Kim L, Dogan S, Porter RW, et al. Hemorrhage of cavernous malformations during pregnancy and in the peripartum period: causal or coincidence? Case report and review of the literature. Neurosurg Focus. 2006; 21:e12. DOI: 10.3171/foc.2006.21.1.13. PMID: 16859250.5. Dias MS, Sekhar LN. Intracranial hemorrhage from aneurysms and arteriovenous malformations during pregnancy and the puerperium. Neurosurgery. 1990; 27:855–65. DOI: 10.1227/00006123-199012000-00001.6. Kiliç T, Pamir MN, Küllü S, Eren F, Ozek MM, Black PM. Expression of structural proteins and angiogenic factors in cerebrovascular anomalies. Neurosurgery. 2000; 46:1179–91. DOI: 10.1097/00006123-200005000-00032. PMID: 10807251.7. Nagamine N, Shintani N, Furuya A, Suzuki S, Nonaka A, Abe F, et al. Anesthetic managements for emergency cesarean section and craniotomy in patients with intracranial hemorrhage due to ruptured cerebral aneurysm and arteriovenous malformation. Masui. 2007; 56:1081–4. PMID: 17877052.8. Chotai S, Qi S, Xu S. Prediction of outcomes for brainstem cavernous malformation. Clin Neurol Neurosurg. 2013; 115:2117–23. DOI: 10.1016/j.clineuro.2013.07.033. PMID: 23962756.9. Hawkins JL. Anesthesia-related maternal mortality. Clin Obstet Gynecol. 2003; 46:679–87. DOI: 10.1097/00003081-200309000-00020. PMID: 12972749.10. Gin T, O’Meara ME, Kan AF, Leung RK, Tan P, Yau G. Plasma catecholamines and neonatal condition after induction of anaesthesia with propofol or thiopentone at caesarean section. Br J Anaesth. 1993; 70:311–6. DOI: 10.1093/bja/70.3.311. PMID: 8471376.11. Tran DT, Newton EK, Mount VA, Lee JS, Wells GA, Perry JJ. Rocuronium versus succinylcholine for rapid sequence induction intubation. Cochrane Database Syst Rev. 2015; 10:CD002788. DOI: 10.1002/14651858.cd002788.pub3.12. Wang LP, Paech MJ. Neuroanesthesia for the pregnant woman. Anesth Analg. 2008; 107:193–200. DOI: 10.1213/ane.0b013e31816c8888. PMID: 18635488.13. Korula G, Farling P. Anesthetic management for a combined Cesarean section and posterior fossa craniectomy. J Neurosurg Anesthesiol. 1998; 10:30–3. DOI: 10.1097/00008506-199801000-00007. PMID: 9438616.14. Martinez-Tica J, Vadhera RB. Disorders of the central nervous systemin pregnancy. Obstetics Anesthesia and Uncommon Disorders. 2nd ed. Gambling DR, editor. New York: Cambridge University Press;2008. p. 167–90. DOI: 10.1017/CBO9780511544552.010.15. Wlody DJ, Weems L. anesthesia for neurosurgery in the pregnant patient. Cottrell and Young’s Neuroanesthesia. 5th ed. Cottrell JE, editor. Philadelphia: Mosby, Inc;2010. p. 416–24.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Anesthetic management during cesarean delivery in a pregnant woman with ruptured cerebral arteriovenous malformation: A case report
- An anesthetic experience with cesarean section in a patient with vasovagal syncope: A case report
- Cavernous Malformation after Radiation Therapy for Pilocytic Astrocytoma: Case Report
- Complete resolution of myoclonus-like involuntary movements under subarachnoid block after midazolam administration in a patient undergoing cesarean section: a case report
- General anesthesia for cesarean section: are we doing it well?