Anesth Pain Med.
2017 Jul;12(3):220-223. 10.17085/apm.2017.12.3.220.
Anesthetic management during cesarean delivery in a pregnant woman with ruptured cerebral arteriovenous malformation: A case report
- Affiliations
-
- 1Department of Anesthesiology and Pain Medicine, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea.
- 2Department of Anesthesiology and Pain Medicine, Seoul Medical Center, Seoul, Korea. choiss@amc.seoul.kr
- KMID: 2388835
- DOI: http://doi.org/10.17085/apm.2017.12.3.220
Abstract
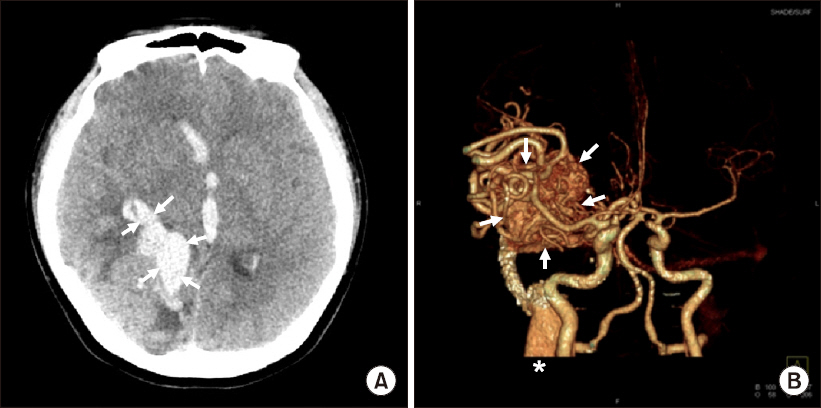
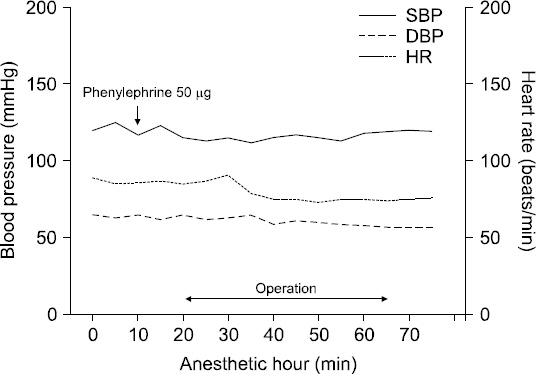
- Although intracranial hemorrhage from arteriovenous malformation (AVM) during pregnancy is rare, it can have fatal consequences. Anesthetic techniques for these patients should ensure precise hemodynamic control, and the goals of anesthesia should include both fetal and maternal well-being. We report a case of anesthetic management for cesarean section in a 31-year-old woman who presented at 32 weeks gestation with an acute intracranial hemorrhage secondary to rupture of a previously diagnosed AVM. Our medical team decided to perform emergent cesarean section under regional anesthesia before transferring the patient to the neurosurgical intensive care unit for further monitoring and appropriate postoperative pain control. The patient was alert and cooperative during neuraxial anesthesia. The operation was successful, and the patient showed gradual improvement in neurosurgical status after several days. We concluded that in case of emergency, regional anesthesia can be a safe strategy for cesarean section in a pregnant woman with symptomatic AVM.
MeSH Terms
Figure
Reference
-
1. Viscomi CM, Wilson J, Bernstein I. Anesthetic management of a parturient with an incompletely resected cerebral arteriovenous malformation. Reg Anesth. 1997; 22:192–7. DOI: 10.1016/S1098-7339(06)80041-6.2. Perquin DA, Kloet A, Tans JT, Witte GN, Dörr PJ. Intracranial arteriovenous malformations in pregnant women. Ned Tijdschr Geneeskd. 1999; 143:497–500. PMID: 10321255.3. Trivedi RA, Kirkpatrick PJ. Arteriovenous malformations of the cerebral circulation that rupture in pregnancy. J Obstet Gynaecol. 2003; 23:484–9. DOI: 10.1080/0144361031000153684. PMID: 12963503.4. Horton JC, Chambers WA, Lyons SL, Adams RD, Kjellberg RN. Pregnancy and the risk of hemorrhage from cerebral arteriovenous malformations. Neurosurgery. 1990; 27:867–71. DOI: 10.1227/00006123-199012000-00002. PMID: 2274126.5. Uchide K, Terada S, Akasofu K, Higashi S. Cerebral arteriovenous malformations in a pregnancy with twins: case report. Neurosurgery. 1992; 31:780–2. DOI: 10.1227/00006123-199210000-00026. PMID: 1407468.6. Gross BA, Du R. Hemorrhage from arteriovenous malformations during pregnancy. Neurosurgery. 2012; 71:349–55. DOI: 10.1227/NEU.0b013e318256c34b. PMID: 22472554.7. Robinson JL, Hall CS, Sedzimir CB. Arteriovenous malformations, aneurysms, and pregnancy. J Neurosurg. 1974; 41:63–70. DOI: 10.3171/jns.1974.41.1.0063. PMID: 4858207.8. Laidler JA, Jackson IJ, Redfern N. The management of caesarean section in a patient with an intracranial arteriovenous malformation. Anaesthesia. 1989; 44:490–1. DOI: 10.1111/j.1365-2044.1989.tb11377.x. PMID: 2667389.9. da Costa L, Wallace MC, Ter Brugge KG, O’Kelly C, Willinsky RA, Tymianski M. The natural history and predictive features of hemorrhage from brain arteriovenous malformations. Stroke. 2009; 40:100–5. DOI: 10.1161/STROKEAHA.108.524678. PMID: 19008469.10. Liu XJ, Wang S, Zhao YL, Zhang D, Zhao JZ. A single-center study of hemorrhagic stroke caused by cerebrovascular disease during pregnancy and puerperium in China. Int J Gynaecol Obstet. 2011; 113:82–3. DOI: 10.1016/j.ijgo.2010.11.010. PMID: 21334622.11. Maclure M. The case-crossover design: a method for studying transient effects on the risk of acute events. Am J Epidemiol. 1991; 133:144–53. DOI: 10.1093/oxfordjournals.aje.a115853. PMID: 1985444.12. Rispoli R, Donati L, Bartolini N, Bolli L, Sulis A, Zofrea G, et al. Rupture of an intracranial arteriovenous malformation (AVM) in pregnancy: Case report. J Stem Cell Res Ther. 2015; 5:2.13. Coskun D, Mahli A, Yilmaz Z, Cizmeci P. Anesthetic management of caesarean section of a pregnant woman with cerebral arteriovenous malformation: a case report. Cases J. 2008; 1:327. DOI: 10.1186/1757-1626-1-327. PMID: 19017413. PMCID: PMC2611980.14. Jeon JY, Do SH, Lee IH, Jee YS, Park SI, Yoon HJ. Effectiveness of spinal anesthesia after epidural labor analgesia versus spinal anesthesia only for intrapartum cesarean section. Anesth Pain Med. 2015; 10:203–7. DOI: 10.17085/apm.2015.10.3.203.15. Block BM, Liu SS, Rowlingson AJ, Cowan AR, Cowan JA Jr, Wu CL. Efficacy of postoperative epidural analgesia: a meta-analysis. JAMA. 2003; 290:2455–63. DOI: 10.1001/jama.290.18.2455. PMID: 14612482.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A case involving anesthesia for cesarean section followed by resection of ruptured cavernous malformation of pons :A case report
- Anesthetic Management for Simultaneous Cesarean Section and Aneurysmal Clipping of the Pregnant with Ruptured Cerebral Aneurysm
- A Case of Anesthetic Management for a Pregnant Woman with Unruptured Cerebral Aneurysm Undergoing Simultaneous Cesarean Section and Aneurysm Clipping: A case report
- Arteriovenous malformation in uterine cervix during pregnancy
- Changes in the Cesarean Section Rate Following the Implementation of Guidelines Concerning Cesarean Section on Maternal Request