J Korean Neurosurg Soc.
2024 May;67(3):299-307. 10.3340/jkns.2024.0047.
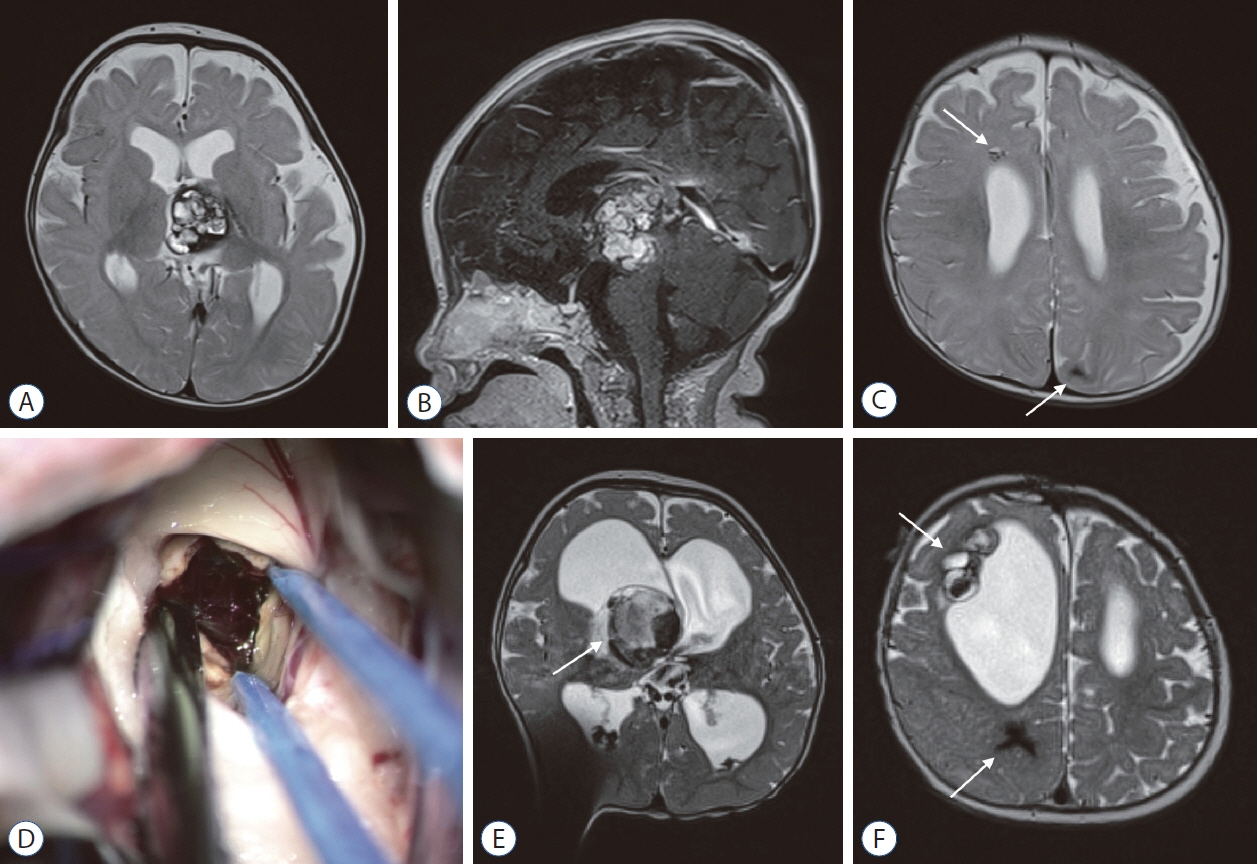
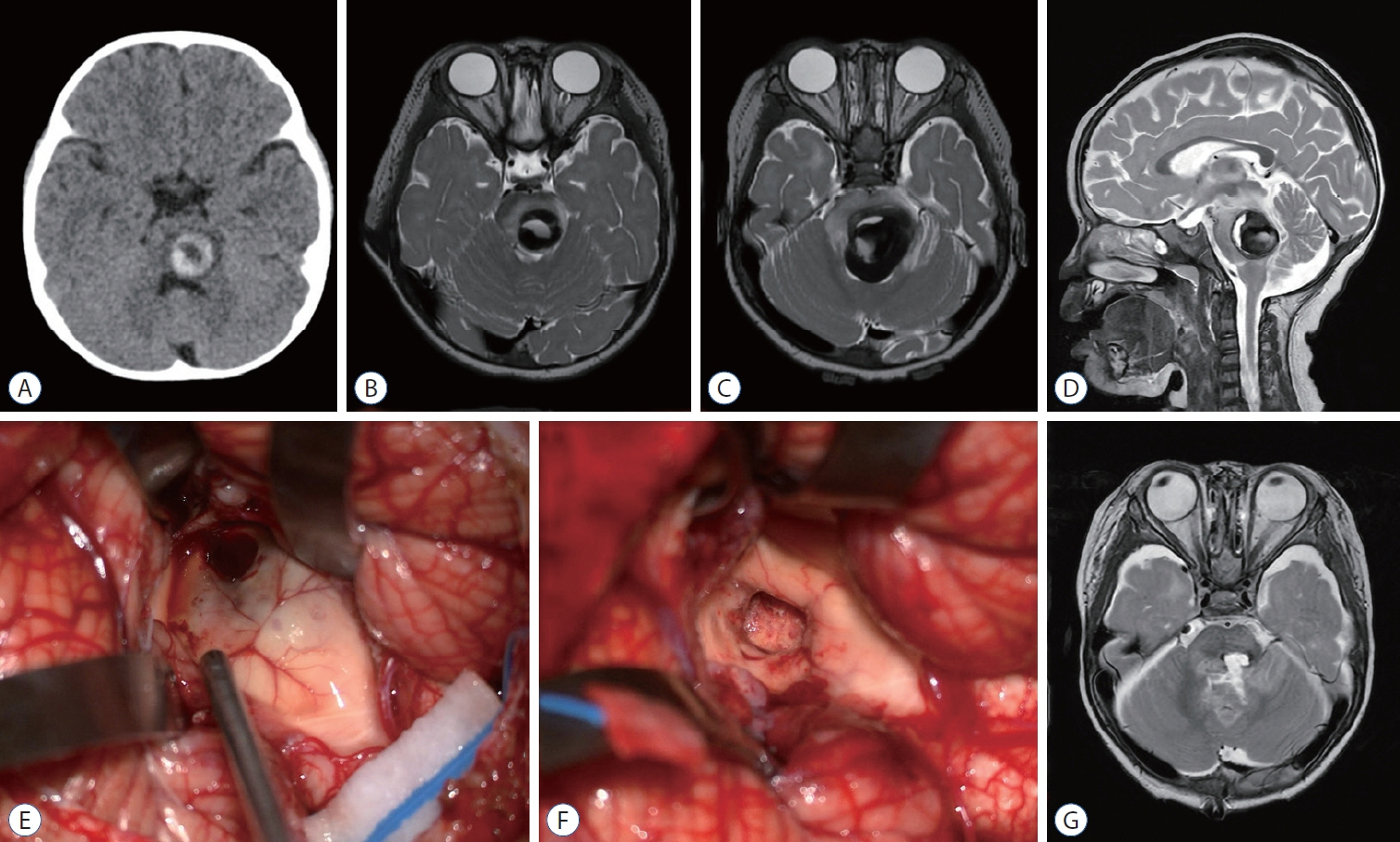
Clinical Features and Treatment of Pediatric Cerebral Cavernous Malformations
- Affiliations
-
- 1Division of Pediatric Neurosurgery, Seoul National University Children’s Hospital, Seoul National University College of Medicine, Seoul, Korea
- KMID: 2554867
- DOI: http://doi.org/10.3340/jkns.2024.0047
Abstract
- Cerebral cavernous malformation (CCM) is a vascular anomaly commonly found in children and young adults. Common clinical presentations of pediatric patients with CCMs include headache, focal neurological deficits, and seizures. Approximately 40% of pediatric patients are asymptomatic. Understanding the natural history of CCM is crucial and hemorrhagic rates are higher in patients with an initial hemorrhagic presentation, whereas it is low in asymptomatic patients. There is a phenomenon known as temporal clustering in which a higher frequency of symptomatic hemorrhages occurs within a few years following the initial hemorrhagic event. Surgical resection remains the mainstay of treatment for pediatric CCMs. Excision of a hemosiderin-laden rim is controversial regarding its impact on epilepsy outcomes. Stereotactic radiosurgery is an alternative treatment, especially for deepseated CCMs, but its true efficacy needs to be verified in a clinical trial.
Keyword
Figure
Reference
-
References
1. Abla AA, Lekovic GP, Garrett M, Wilson DA, Nakaji P, Bristol R, et al. Cavernous malformations of the brainstem presenting in childhood: surgical experience in 40 patients. Neurosurgery. 67:1589–1589. discussion 1598-1599. 2010.
Article2. Al-Holou WN, O’Lynnger TM, Pandey AS, Gemmete JJ, Thompson BG, Muraszko KM, et al. Natural history and imaging prevalence of cavernous malformations in children and young adults. J Neurosurg Pediatr. 9:198–205. 2012.
Article3. Al-Shahi Salman R, Berg MJ, Morrison L, Awad IA; Angioma Alliance Scientific Advisory Board. Hemorrhage from cavernous malformations of the brain: definition and reporting standards. Angioma Alliance Scientific Advisory Board. Stroke. 39:3222–3230. 2008.
Article4. Al-Shahi Salman R, Hall JM, Horne MA, Moultrie F, Josephson CB, Bhattacharya JJ, et al. Untreated clinical course of cerebral cavernous malformations: a prospective, population-based cohort study. Lancet Neurol. 11:217–224. 2012.
Article5. Al-Shahi Salman R, Kitchen N, Thomson J, Ganesan V, Mallucci C, Radatz M, et al. Top ten research priorities for brain and spine cavernous malformations. Lancet Neurol. 15:354–355. 2016.
Article6. Aoki R, Srivatanakul K. Developmental venous anomaly: benign or not benign. Neurol Med Chir (Tokyo). 56:534–543. 2016.
Article7. Awad I, Jabbour P. Cerebral cavernous malformations and epilepsy. Neurosurg Focus. 21:e7. 2006.
Article8. Barker FG 2nd, Amin-Hanjani S, Butler WE, Lyons S, Ojemann RG, Chapman PH, et al. Temporal clustering of hemorrhages from untreated cavernous malformations of the central nervous system. Neurosurgery. 49:15–24. discussion 24-25. 2001.
Article9. Baumann CR, Schuknecht B, Lo Russo G, Cossu M, Citterio A, Andermann F, et al. Seizure outcome after resection of cavernous malformations is better when surrounding hemosiderin-stained brain also is removed. Epilepsia. 47:563–566. 2006.
Article10. Blumcke I, Spreafico R, Haaker G, Coras R, Kobow K, Bien CG, et al. Histopathological findings in brain tissue obtained during epilepsy surgery. N Engl J Med. 377:1648–1656. 2017.
Article11. Campeau NG, Lane JI. De novo development of a lesion with the appearance of a cavernous malformation adjacent to an existing developmental venous anomaly. AJNR Am J Neuroradiol. 26:156–159. 2005.12. Casazza M, Broggi G, Franzini A, Avanzini G, Spreafico R, Bracchi M, et al. Supratentorial cavernous angiomas and epileptic seizures: preoperative course and postoperative outcome. Neurosurgery. 39:26–32. discussion 32-34. 1996.
Article13. Das A, Goyal A, Sangwan A, Bhalla AS, Kumar A, Kandasamy D, et al. Vascular anomalies: nomenclature, classification, and imaging algorithms. Acta Radiol. 64:837–849. 2023.
Article14. Detwiler PW, Porter RW, Zabramski JM, Spetzler RF. De novo formation of a central nervous system cavernous malformation: implications for predicting risk of hemorrhage. Case report and review of the literature. J Neurosurg. 87:629–632. 1997.
Article15. Flemming KD, Lanzino G. Cerebral cavernous malformation: what a practicing clinician should know. Mayo Clin Proc. 95:2005–2020. 2020.
Article16. Fontanella MM, Agosti E, Zanin L, di Bergamo LT, Doglietto F. Cerebral cavernous malformation remnants after surgery: a single-center series with long-term bleeding risk analysis. Neurosurg Rev. 44:2639–2645. 2021.
Article17. Giliberto G, Lanzino DJ, Diehn FE, Factor D, Flemming KD, Lanzino G. Brainstem cavernous malformations: anatomical, clinical, and surgical considerations. Neurosurg Focus. 29:E9. 2010.
Article18. Goyal A, Fernandes-Torres J, Flemming KD, Williams LN, Daniels DJ. Clinical presentation, natural history, and outcomes for infantile intracranial cavernous malformations: case series and systematic review of the literature. Childs Nerv Syst. 39:1545–1554. 2023.
Article19. Gross BA, Du R, Orbach DB, Scott RM, Smith ER. The natural history of cerebral cavernous malformations in children. J Neurosurg Pediatr. 17:123–128. 2016.
Article20. Hayashi S, Kondoh T, Morishita A, Sasayama T, Sanabria EA, Kohmura E. Congenital cavernous angioma exhibits a progressive decrease in size after birth. Childs Nerv Syst. 20:199–203. 2004.
Article21. Henrich W, Stupin JH, Bühling KJ, Bührer C, Bassir C, Dudenhausen JW. Prenatal sonographic findings of thalamic cavernous angioma. Ultrasound Obstet Gynecol. 19:518–522. 2002.
Article22. Horne MA, Flemming KD, Su IC, Stapf C, Jeon JP, Li D, et al. Clinical course of untreated cerebral cavernous malformations: a meta-analysis of individual patient data. Lancet Neurol. 15:166–173. 2016.
Article23. Jin Y, Zhao C, Zhang S, Zhang X, Qiu Y, Jiang J. Seizure outcome after surgical resection of supratentorial cavernous malformations plus hemosiderin rim in patients with short duration of epilepsy. Clin Neurol Neurosurg. 119:59–63. 2014.
Article24. Josephson CB, Rosenow F, Al-Shahi Salman R. Intracranial vascular malformations and epilepsy. Semin Neurol. 35:223–234. 2015.
Article25. Karaaslan B, Gülsuna B, Erol G, Dağli Ö, Emmez H, Kurt G, et al. Stereotactic radiosurgery for cerebral cavernous malformation: comparison of hemorrhage rates before and after stereotactic radiosurgery. J Neurosurg. 136:655–661. 2021.
Article26. Kondziolka D, Lunsford LD, Flickinger JC, Kestle JR. Reduction of hemorrhage risk after stereotactic radiosurgery for cavernous malformations. J Neurosurg. 83:825–831. 1995.
Article27. Lanfranconi S, Scola E, Meessen JMTA, Pallini R, Bertani GA, Al-Shahi Salman R, et al. Safety and efficacy of propranolol for treatment of familial cerebral cavernous malformations (Treat_CCM): a randomised, open-label, blinded-endpoint, phase 2 pilot trial. Lancet Neurol. 22:35–44. 2023.
Article28. Lerner A, Gilboa Y, Gerad L, Malinger G, Kidron D, Achiron R. Sonographic detection of fetal cerebellar cavernous hemangioma with inutero hemorrhage leading to cerebellar hemihypoplasia. Ultrasound Obstet Gynecol. 28:968–971. 2006.
Article29. Li W, Shenkar R, Detter MR, Moore T, Benavides C, Lightle R, et al. Propranolol inhibits cavernous vascular malformations by β1 adrenergic receptor antagonism in animal models. J Clin Invest. 131:e154909. 2021.
Article30. Lin F, Gao Z, Li C, Wang D, He Q, Kang D, et al. Intra-operative electrocorticography results and postoperative pathological findings are associated with epileptic outcomes in patients with cerebral cavernous malformations presenting with epilepsy. Epilepsy Res. 174:106672. 2021.
Article31. Lin Q, Yang PF, Jia YZ, Pei JS, Xiao H, Zhang TT, et al. Surgical treatment and long-term outcome of cerebral cavernous malformationsrelated epilepsy in pediatric patients. Neuropediatrics. 49:173–179. 2018.
Article32. Lunsford LD, Khan AA, Niranjan A, Kano H, Flickinger JC, Kondziolka D. Stereotactic radiosurgery for symptomatic solitary cerebral cavernous malformations considered high risk for resection. J Neurosurg. 113:23–29. 2010.
Article33. Mantziaris G, Dumot C, Pikis S, Peker S, Samanci Y, Ardor GD, et al. Pediatric cerebral cavernous malformations and stereotactic radiosurgery: an analysis of 50 cases from a multicentric study. J Neurosurg Pediatr. 4:315–322. 2024.
Article34. Morota N, Deletis V. Brainstem surgery: functional surgical anatomy with the use of an advanced modern intraoperative neurophysiological procedure. Adv Tech Stand Neurosurg. 48:21–55. 2023.
Article35. Oldenburg J, Malinverno M, Globisch MA, Maderna C, Corada M, Orsenigo F, et al. Propranolol reduces the development of lesions and rescues barrier function in cerebral cavernous malformations: a preclinical study. Stroke. 52:1418–1427. 2021.
Article36. Paddock M, Lanham S, Gill K, Sinha S, Connolly DJA. Pediatric cerebral cavernous malformations. Pediatr Neurol. 116:74–83. 2021.
Article37. Polster SP, Stadnik A, Akers AL, Cao Y, Christoforidis GA, Fam MD, et al. Atorvastatin treatment of cavernous angiomas with symptomatic hemorrhage exploratory proof of concept (AT CASH EPOC) trial. Neurosurgery. 85:843–853. 2019.
Article38. Porter RW, Detwiler PW, Spetzler RF. Surgical technique for resection of cavernous malformations of the brain stem. Oper Tech Neurosurg. 3:124–130. 2000.
Article39. Porter RW, Detwiler PW, Spetzler RF, Lawton MT, Baskin JJ, Derksen PT, et al. Cavernous malformations of the brainstem: experience with 100 patients. J Neurosurg. 90:50–58. 1999.
Article40. Rajeswarie RT, Aravinda HR, Arivazhagan A, Bevinahalli NN, Rao MB, Mahadevan A. Evaluating the role of perilesional tissue in pathobiology of epileptogenesis of vascular malformations of the central nervous system. J Epilepsy Res. 12:53–61. 2022.
Article41. Richardson BT, Dibble CF, Borikova AL, Johnson GL. Cerebral cavernous malformation is a vascular disease associated with activated RhoA signaling. Biol Chem. 394:35–42. 2013.
Article42. Rosenow F, Alonso-Vanegas MA, Baumgartner C, Blümcke I, Carreño M, Gizewski ER, et al. Cavernoma-related epilepsy: review and recommendations for management--report of the Surgical Task Force of the ILAE Commission on Therapeutic Strategies. Epilepsia. 54:2025–2035. 2013.
Article43. Santos AN, Rauschenbach L, Saban D, Chen B, Herten A, Dinger TF, et al. Natural course of cerebral cavernous malformations in children: a five-year follow-up study. Stroke. 53:817–824. 2022.
Article44. Shang-Guan HC, Wu ZY, Yao PS, Chen GR, Zheng SF, Kang DZ. Is extended lesionectomy needed for patients with cerebral cavernous malformations presenting with epilepsy? A meta-analysis. World Neurosurg. 120:e984–e990. 2018.45. Shenkar R, Peiper A, Pardo H, Moore T, Lightle R, Girard R, et al. Rho kinase inhibition blunts lesion development and hemorrhage in murine models of aggressive Pdcd10/Ccm3 disease. Stroke. 50:738–744. 2019.46. Shenkar R, Shi C, Austin C, Moore T, Lightle R, Cao Y, et al. RhoA kinase inhibition with fasudil versus simvastatin in murine models of cerebral cavernous malformations. Stroke. 48:187–194. 2017.47. Shih YC, Chou CC, Peng SJ, Yu HY, Hsu SPC, Lin CF, et al. Clinical characteristics and long-term outcome of cerebral cavernous malformationsrelated epilepsy. Epilepsia. 63:2056–2067. 2022.48. Shim Y, Phi JH, Wang KC, Cho BK, Lee JY, Koh EJ, et al. Clinical outcomes of pediatric cerebral cavernous malformation: an analysis of 124 consecutive cases. J Neurosurg Pediatr. 30:474–483. 2022.49. Smith ER, Scott RM. Cavernous malformations. Neurosurg Clin N Am. 21:483–490. 2010.
Article50. Stavrou I, Baumgartner C, Frischer JM, Trattnig S, Knosp E. Long-term seizure control after resection of supratentorial cavernomas: a retrospective single-center study in 53 patients. Neurosurgery. 63:888–896. discussion 897. 2008.51. Steiner L, Karlsson B, Yen CP, Torner JC, Lindquist C, Schlesinger D. Radiosurgery in cavernous malformations: anatomy of a controversy. J Neurosurg. 113:16–21. discussion 21-22. 2010.52. Velz J, Özkaratufan S, Krayenbühl N, Beccaria K, Akeret K, Attieh C, et al. Pediatric brainstem cavernous malformations: 2-center experience in 40 children. J Neurosurg Pediatr. 29:612–623. 2022.
Article53. Willmore LJ, Sypert GW, Munson JB. Recurrent seizures induced by cortical iron injection: a model of posttraumatic epilepsy. Ann Neurol. 4:329–336. 1978.
Article54. Zevgaridis D, van Velthoven V, Ebeling U, Reulen HJ. Seizure control following surgery in supratentorial cavernous malformations: a retrospective study in 77 patients. Acta Neurochir (Wien). 138:672–677. 1996.
Article55. Zhang P, Zhang H, Shi C, Zhou J, Dong J, Liang M, et al. Clinical characteristics and risk factors of cerebral cavernous malformation-related epilepsy. Epilepsy Behav. 139:109064. 2023.
Article56. Zuurbier SM, Hickman CR, Rinkel LA, Berg R, Sure U, Al-Shahi Salman R, et al. Association between beta-blocker or statin drug use and the risk of hemorrhage from cerebral cavernous malformations. Stroke. 53:2521–2527. 2022.
Article57. Zuurbier SM, Santos AN, Flemming KD, Schmidt B, Jabbarli R, Lanzino G, et al. Female hormone therapy and risk of intracranial hemorrhage from cerebral cavernous malformations: a multicenter observational cohort study. Neurology. 100:e1673–e1679. 2023.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Cavernous Hemangioma on the Frontal Lobe
- Corrigendum to “Clinical Features and Treatment of Pediatric Cerebral Cavernous Malformations” by Phi et al. (J Korean Neurosurg Soc 67 : 299-307, 2024)
- Pediatric Cerebral Vascular Malformations : Current and Future Perspectives
- Giant Cystic Cerebral Cavernous Malformation with Multiple Calcification: Case Report
- Pediatric Central Nervous System Vascular Malformation : Pathological Review with Diagram