J Korean Neurosurg Soc.
2024 Jul;67(4):458-466. 10.3340/jkns.2023.0203.
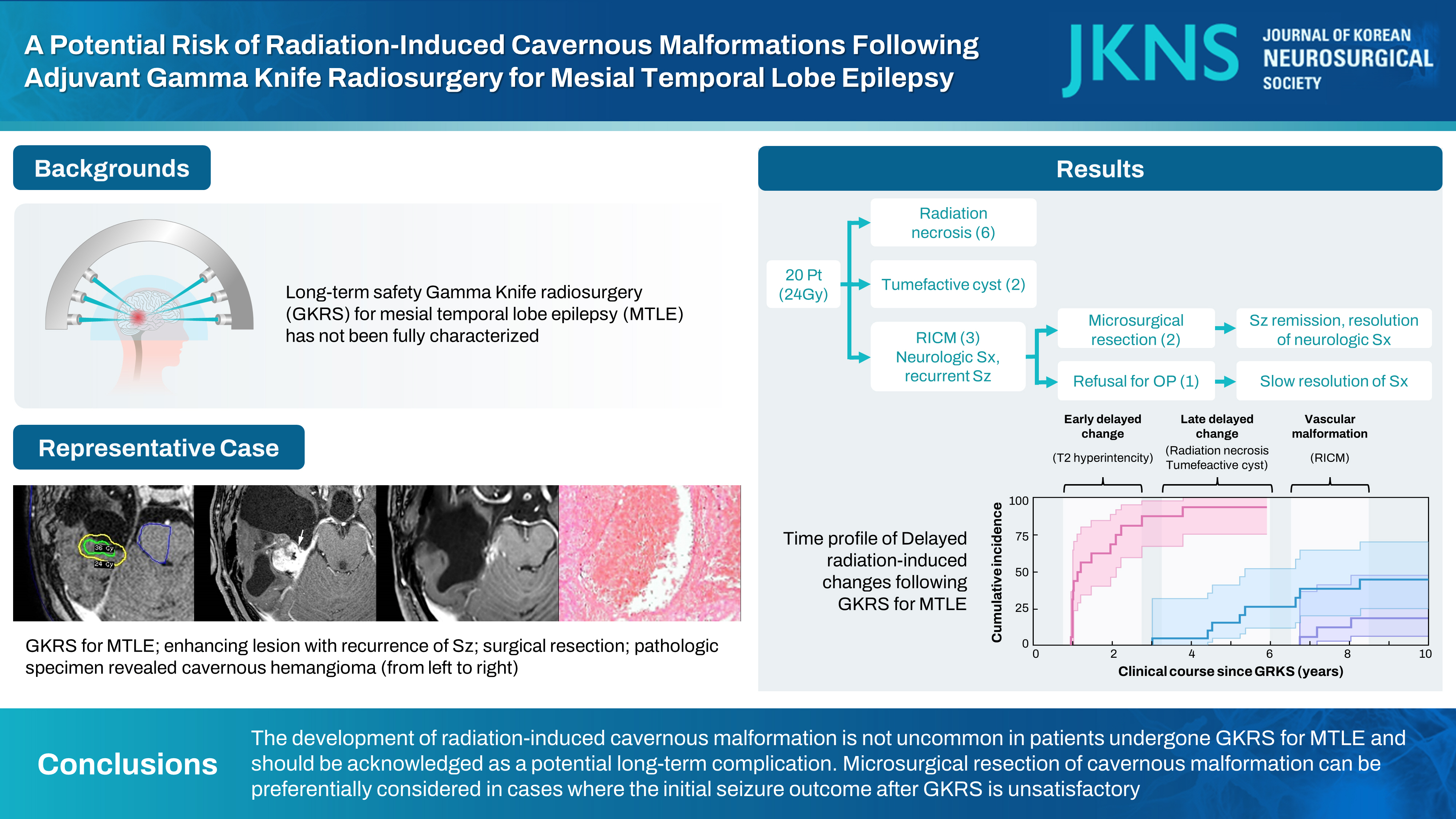
A Potential Risk of Radiation-Induced Cavernous Malformations Following Adjuvant Gamma Knife Radiosurgery for Mesial Temporal Lobe Epilepsy
- Affiliations
-
- 1Department of Neurological Surgery, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea
- KMID: 2556743
- DOI: http://doi.org/10.3340/jkns.2023.0203
Abstract
Objective
: Several clinical studies have explored the feasibility and efficacy of radiosurgical treatment for mesial temporal lobe epilepsy, but the long-term safety of this treatment has not been fully characterized. This study aims to report and describe radiation-induced cavernous malformation as a delayed complication of radiosurgery in epilepsy patients.
Methods
: The series includes 20 patients with mesial temporal lobe epilepsy who underwent Gamma Knife radiosurgery (GKRS). The majority received a prescribed isodose of 24 Gy as an adjuvant treatment after anterior temporal lobectomy.
Results
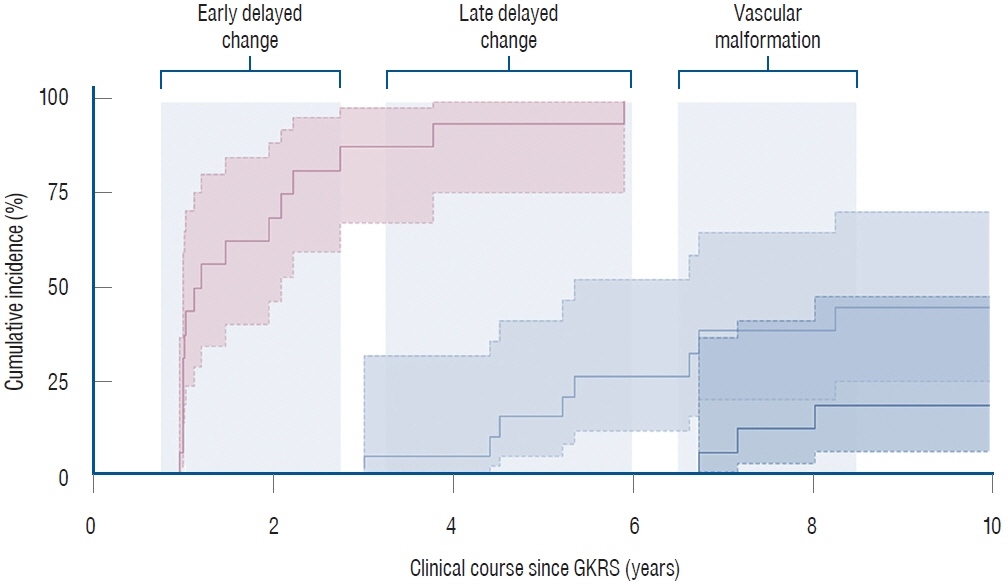
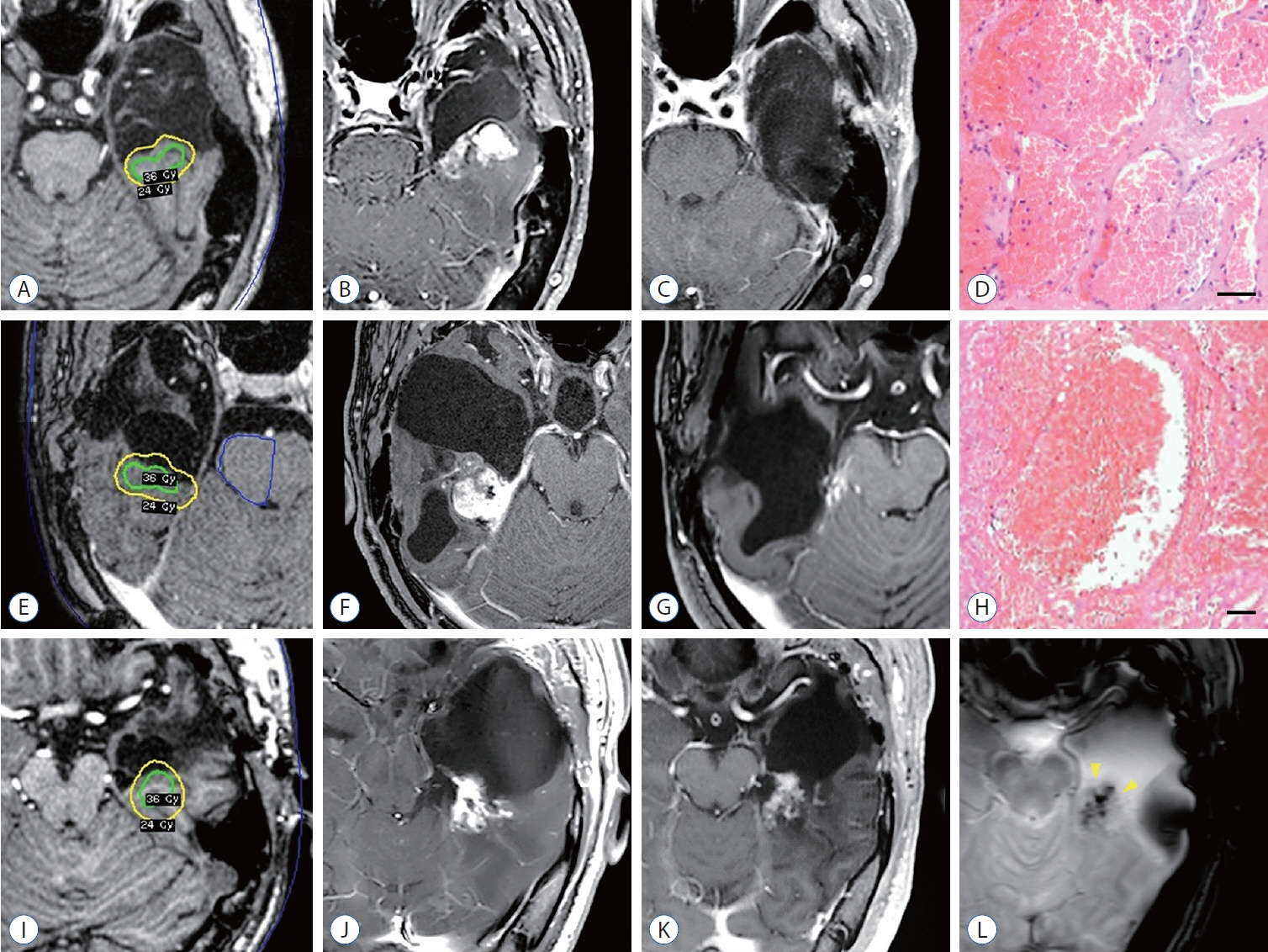
: In this series, we identified radiation-induced cavernous malformation in three patients, resulting in a cumulative incidence of 18.4% (95% confidence interval, 6.3% to 47.0%) at an 8-year follow-up. These late sequelae of vascular malformation occurred between 6.9 and 7.6 years after GKRS, manifesting later than other delayed radiation-induced changes, such as radiation necrosis. Neurological symptoms attributed to intracranial hypertension were present in those three cases involving cavernous malformation. Of these, two cases, which initially exhibited an insufficient response to radiosurgery, ultimately demonstrated seizure remission following the successful microsurgical resection of the cavernous malformation.
Conclusion
: All things considered, the development of radiation-induced cavernous malformation is not uncommon in this population and should be acknowledged as a potential long-term complication. Microsurgical resection of cavernous malformation can be preferentially considered in cases where the initial seizure outcome after GKRS is unsatisfactory.
Keyword
Figure
Cited by 1 articles
-
Editors’ Pick in July 2024
Hee-Jin Yang
J Korean Neurosurg Soc. 2024;67(4):383-384. doi: 10.3340/jkns.2024.0119.
Reference
-
References
1. Abe K, Yamaguchi T, Hori H, Sumi M, Horisawa S, Taira T, et al. Magnetic resonance-guided focused ultrasound for mesial temporal lobe epilepsy: a case report. BMC Neurol. 20:160. 2020.
Article2. Barbaro NM, Quigg M, Broshek DK, Ward MM, Lamborn KR, Laxer KD, et al. A multicenter, prospective pilot study of gamma knife radiosurgery for mesial temporal lobe epilepsy: seizure response, adverse events, and verbal memory. Ann Neurol. 65:167–175. 2009.
Article3. Barbaro NM, Quigg M, Ward MM, Chang EF, Broshek DK, Langfitt JT, et al. Radiosurgery versus open surgery for mesial temporal lobe epilepsy: the randomized, controlled ROSE trial. Epilepsia. 59:1198–1207. 2018.
Article4. Bartolomei F, Hayashi M, Tamura M, Rey M, Fischer C, Chauvel P, et al. Long-term efficacy of gamma knife radiosurgery in mesial temporal lobe epilepsy. Neurology. 70:1658–1663. 2008.
Article5. Chen N, Du SQ, Yan N, Liu C, Zhang JG, Ge Y, et al. Delayed complications after gamma knife surgery for intractable epilepsy. J Clin Neurosci. 21:1525–1528. 2014.
Article6. Cmelak AJ, Abou-Khalil B, Konrad PE, Duggan D, Maciunas RJ. Low-dose stereotactic radiosurgery is inadequate for medically intractable mesial temporal lobe epilepsy: a case report. Seizure. 10:442–446. 2001.
Article7. Cutsforth-Gregory JK, Lanzino G, Link MJ, Brown RD Jr, Flemming KD. Characterization of radiation-induced cavernous malformations and comparison with a nonradiation cavernous malformation cohort. J Neurosurg. 122:1214–1222. 2015.
Article8. Gross BA, Lin N, Du R, Day AL. The natural history of intracranial cavernous malformations. Neurosurg Focus. 30:E24. 2011.
Article9. Kang JY, Wu C, Tracy J, Lorenzo M, Evans J, Nei M, et al. Laser interstitial thermal therapy for medically intractable mesial temporal lobe epilepsy. Epilepsia. 57:325–334. 2016.
Article10. Kawai K, Suzuki I, Kurita H, Shin M, Arai N, Kirino T. Failure of low-dose radiosurgery to control temporal lobe epilepsy. J Neurosurg. 95:883–887. 2001.
Article11. Kawamura T, Onishi H, Kohda Y, Hirose G. Serious adverse effects of gamma knife radiosurgery for mesial temporal lobe epilepsy. Neurol Med Chir (Tokyo). 52:892–898. 2012.
Article12. Kim MJ, Chang KW, Park SH, Chang WS, Chang JH, Chang JW, et al. Predictive factors of radiation-induced changes following single-session gamma knife radiosurgery for arteriovenous malformations. J Clin Med. 10:2186. 2021.
Article13. Koike T, Yanagimachi N, Ishiguro H, Yabe H, Yabe M, Morimoto T, et al. High incidence of radiation-induced cavernous hemangioma in longterm survivors who underwent hematopoietic stem cell transplantation with radiation therapy during childhood or adolescence. Biol Blood Marrow Transplant. 18:1090–1098. 2012.
Article14. Lee EM, Kang JK, Kim SJ, Hong SH, Ko TS, Lee SA, et al. Gamma knife radiosurgery for recurrent or residual seizures after anterior temporal lobectomy in mesial temporal lobe epilepsy patients with hippocampal sclerosis: long-term follow-up results of more than 4 years. J Neurosurg. 123:1375–1382. 2015.
Article15. Lew SM, Morgan JN, Psaty E, Lefton DR, Allen JC, Abbott R. Cumulative incidence of radiation-induced cavernomas in long-term survivors of medulloblastoma. J Neurosurg. 104(2 Suppl):103–107. 2006.
Article16. McGonigal A, Sahgal A, De Salles A, Hayashi M, Levivier M, Ma L, et al. Radiosurgery for epilepsy: systematic review and International Stereotactic Radiosurgery Society (ISRS) practice guideline. Epilepsy Res. 137:123–131. 2017.
Article17. Nimjee SM, Powers CJ, Bulsara KR. Review of the literature on de novo formation of cavernous malformations of the central nervous system after radiation therapy. Neurosurg Focus. 21:e4. 2006.
Article18. Patet G, Bartoli A, Meling TR. Natural history and treatment options of radiation-induced brain cavernomas: a systematic review. Neurosurg Rev. 45:243–251. 2022.
Article19. Régis J, Rey M, Bartolomei F, Vladyka V, Liscak R, Schröttner O, et al. Gamma knife surgery in mesial temporal lobe epilepsy: a prospective multicenter study. Epilepsia. 45:504–515. 2004.
Article20. Srikijvilaikul T, Najm I, Foldvary-Schaefer N, Lineweaver T, Suh JH, Bingaman WE. Failure of gamma knife radiosurgery for mesial temporal lobe epilepsy: report of five cases. Neurosurgery. 54:1395–1402. discussion 1402-1404. 2004.
Article21. Trifiletti DM, Redmond KJ, Kim MM, Soltys SG, Milano MT, HattangadiGluth JA. Novel applications of stereotactic radiosurgery beyond oncology: prospective trials in functional radiosurgery. Int J Radiat Oncol Biol Phys. 115:4–6. 2023.
Article22. Vojtěch Z, Malíková H, Syrůček M, Krámská L, Šroubek J, Vladyka V, et al. Morphological changes after radiosurgery for mesial temporal lobe epilepsy. Acta Neurochir (Wien). 157:1783–1791. discussion 1791-1792. 2015.
Article23. Vojtech Z, Vladyka V, Kalina M, Nespor E, Seltenreichová K, Semnická J, et al. The use of radiosurgery for the treatment of mesial temporal lobe epilepsy and long-term results. Epilepsia. 50:2061–2071. 2009.
Article24. Winkler EA, Rutledge C, Ward M, Tihan T, Sneed PK, Barbaro N, et al. Radiation-induced cavernous malformation as a late sequelae of stereotactic radiosurgery for epilepsy. Cureus. 10:e2308. 2018.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Radiosurgery for Cavernous Malformations
- Radiosurgery for Cerebrovascular Disease
- Fractionated Stereotactic Gamma Knife Radiosurgery for Medial Temporal Lobe Epilepsy: A Case Report
- Semiology and its Lateralizing Signs in Mesial Temporal Lobe Epilepsy
- Development of De Novo Cavernous Hemangioma after Radiosurgery for Cavernous Hemangioma