J Korean Endocr Soc.
2008 Aug;23(4):260-265.
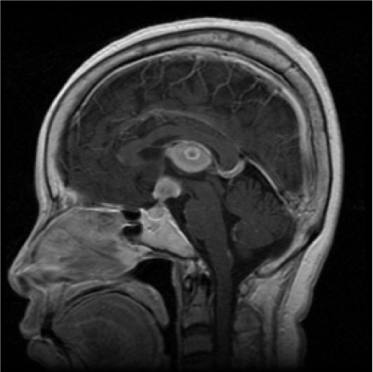
A Case of Panhypopituitarism and Central Diabetes Insipidus Caused by Primary Central Nervous System Lymphoma
- Affiliations
-
- 1Department of Endocrinology and Metabolism, Ajou University School of MedicineKorea.
- 2Department of Hematology-Oncology, Ajou University School of MedicineKorea.
- 3Department of Neurosurgery, Ajou University School of MedicineKorea.
- 4Department of Pathology, Ajou University School of MedicineKorea.
- 5Department of Radiology, Ajou University School of Medicine, Korea.
Abstract
- Primary central nervous system (CNS) lymphoma is an uncommon neoplasm. However, the incidence of primary CNS lymphoma has increased more than 10-fold over the past three decades, and continues to accelerate. Currently, primary CNS lymphoma represents 4 to 7 percent of all newly diagnosed primary CNS tumors. Primary CNS lymphoma may arise from different parts of the brain, with deep hemispheric periventricular white matter being the most common site of origin. The presenting symptoms in primary CNS lymphoma vary depending on the location of the mass. Involvement of the hypothalamic-pituitary axis may cause hypopituitarism, diabetes insipidus, headache, diplopia, and blurred vision.
MeSH Terms
Figure
Reference
-
1. Fine HA MR. Primary central nervous system lymphoma. Ann Intern Med. 1993. 119:1093–1104.2. Batchelor T, Loeffler JS. Primary CNS lymphoma. J Clin Oncol. 2006. 24:1281–1288.3. Erdag N, Bhorade RM, Alberico RA, Yousuf N, Patel MR. Primary lymphoma of the central nervous system: typical and atypical CT and MR imaging appearances. Am J Roentgenol. 2001. 176:1319–1326.4. Kaufmann TJ, Lopes MB, Laws ER Jr, Lipper MH. Primary sellar lymphoma: radiologic and pathologic findings in two patients. Am J Neuroradiol. 2002. 23:364–367.5. Liu JK, Sayama C, Chin SS, Couldwell WT. Extranodal NK/T-cell lymphoma presenting as a pituitary mass: case report and review of the literature. J Neurosurg. 2007. 107:660–665.6. Silfen ME, Garvin JH Jr, Hays AP, Starkman HS, Aranoff GS, Levine LS, Feldstein NA, Wong B, Oberfield SE. Primary central nervous system lymphoma in childhood presenting as progressive panhypopituitarism. J Pediatr Hematol Oncol. 2001. 23:130–133.7. Kim SH, Han DC, Park HM, Lee YB, Shin WC. A case of primary pituitary lymphoma. J Kor Neurol Assoc. 2006. 24:169–171.8. Miller DC, Hochberg FH, Harris NL, Gruber ML, Louis DN, Cohen H. Pathology with clinical correlations of primary central nervous system non-Hodgkin's lymphoma: The Massachusetts General Hospital experience 1958-1989. Cancer. 1994. 74:1383–1397.9. Hochberg FH, Miller DC. Primary central nervous system lymphoma. J Neurosurg. 1988. 68:835–853.10. Ahsan H, Neugut AI, Bruce JN. Trends in incidence of primary malignant brain tumors in USA, 1981-1990. Int J Epidemiol. 1995. 24:1078–1085.11. Nitta T, Kasuga C, Yasumoto Y, Okuda O, Kudo S, Sato K. A clinicopathological study of 21 cases of primary central nervous system lymphoma. No Shinkei Geka. 1994. 22:827–832.12. Kim IM, Son EI, Kim DW, Yim MB, Kim SP. Treatment strategies for primary central nervous system lymphoma. J Kor Neurosurg Soc. 2001. 30:334–341.13. Lee SH, Kim HS, Lee YM, Yoon YS, Lim SK, Lee HC, Huh KB. A case of central diabetes insipidus caused by metastatic malignant lymphoma. J Kor Endocrinol Soc. 1997. 12:596–601.14. Kwak JW, Hong SH, Kim JH, Lee SH, Jo JH, Kwon HS, Youn KH, Cha BY, Son HY. A case of pituitary metastasis of breast cancer presenting as diabetes insipidus and panhypopituitarism. J Kor Endocrinol Soc. 2007. 22:125–129.15. Rollins KE, Kleinschmidt-DeMasters BK, Corboy JR, Damek DM, Filley CM. Lymphomatosis cerebri as a cause of white matter dementia. Hum Pathol. 2005. 36:282–290.16. Capra M, Wherrett D, Weitzman S, Dirks P, Hawkins C, Bouffet E. Pituitary stalk thickening and primary central nervous system lymphoma. J Neuro-Oncology. 2004. 67:227–231.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Primary Central Nervous System Lymphoma with Panhypopituitarism
- Central Diabetes Insipidus Occurring during Therapy for Tsutsugamushi Disease
- A Case of Synchronized Pineal and Suprasellar Germinoma
- Primary Central Nervous System Lymphoma Mimicking Behcet's Disease
- A Case of Pituitary Metastasis of Breast Cancer Presenting as Diabetes Insipidus and Panhypopituitarism