J Korean Assoc Oral Maxillofac Surg.
2010 Oct;36(5):408-412.
The clinical study on the sedative effect and recovery in patients undergoing intravenous conscious sedation with midazolam for mandibular third molars extraction
- Affiliations
-
- 1Department of Oral and Maxillofacial Surgery, Mokdong Hospital, School of Medicine, Ewha Womans University, Seoul, Korea. sjsj7777@ewha.ac.kr
Abstract
- INTRODUCTION
This study examined the depth of sedation and the usefulness of the monitoring tool in determining the level of sedation in patients undergoing third molars extraction under conscious sedation with midazolam.
MATERIALS AND METHODS
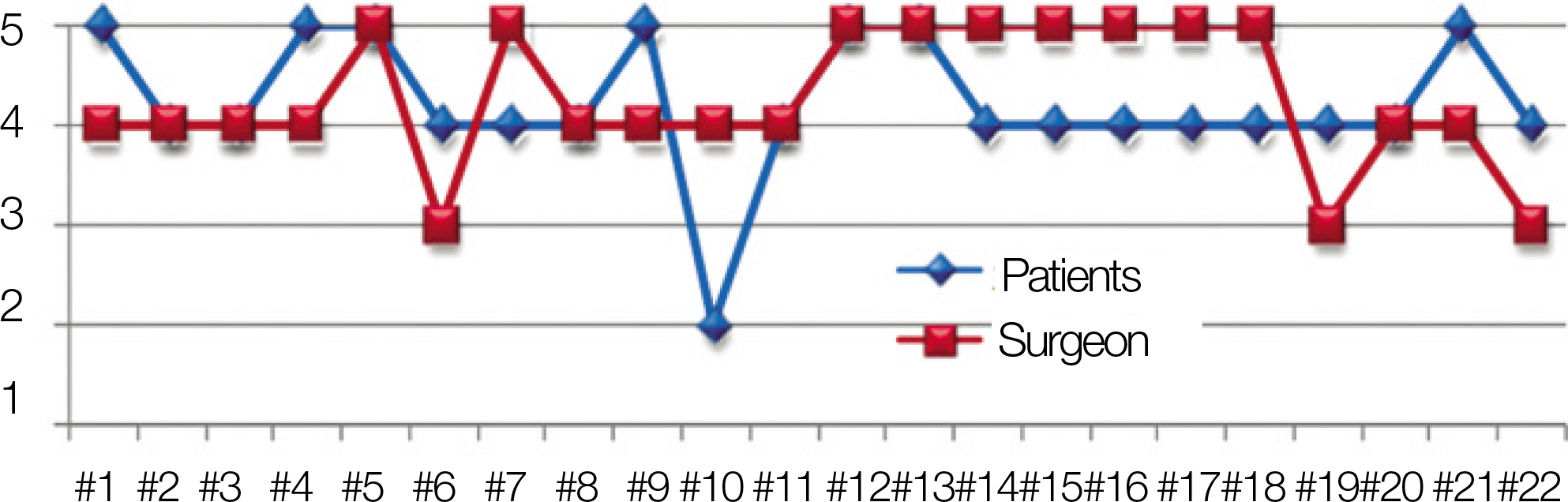
Twenty two patients undergoing third molars extraction at the department of Oral and Maxillofacial surgery, Ewha Womans Mokdong Hospital from February 2010 to April 2010 were analyzed. All patients were classified as American Society of Anesthesiologist (ASA) class I and had no contraindications tosedation. The bispectral index was recorded continually during surgery using a bispectral monitor. The initial sedation was accomplished using a 3 mg bolus of midazolam followed by a 2 mg bolus of midazolam until the level of sedation, at which the patient's eyes were closed or the subject was responsive only to loud or repeated calling of their name, was reached. All subjects were surveyed with a postoperative questionnaire to evaluate the level of sedation.
RESULTS
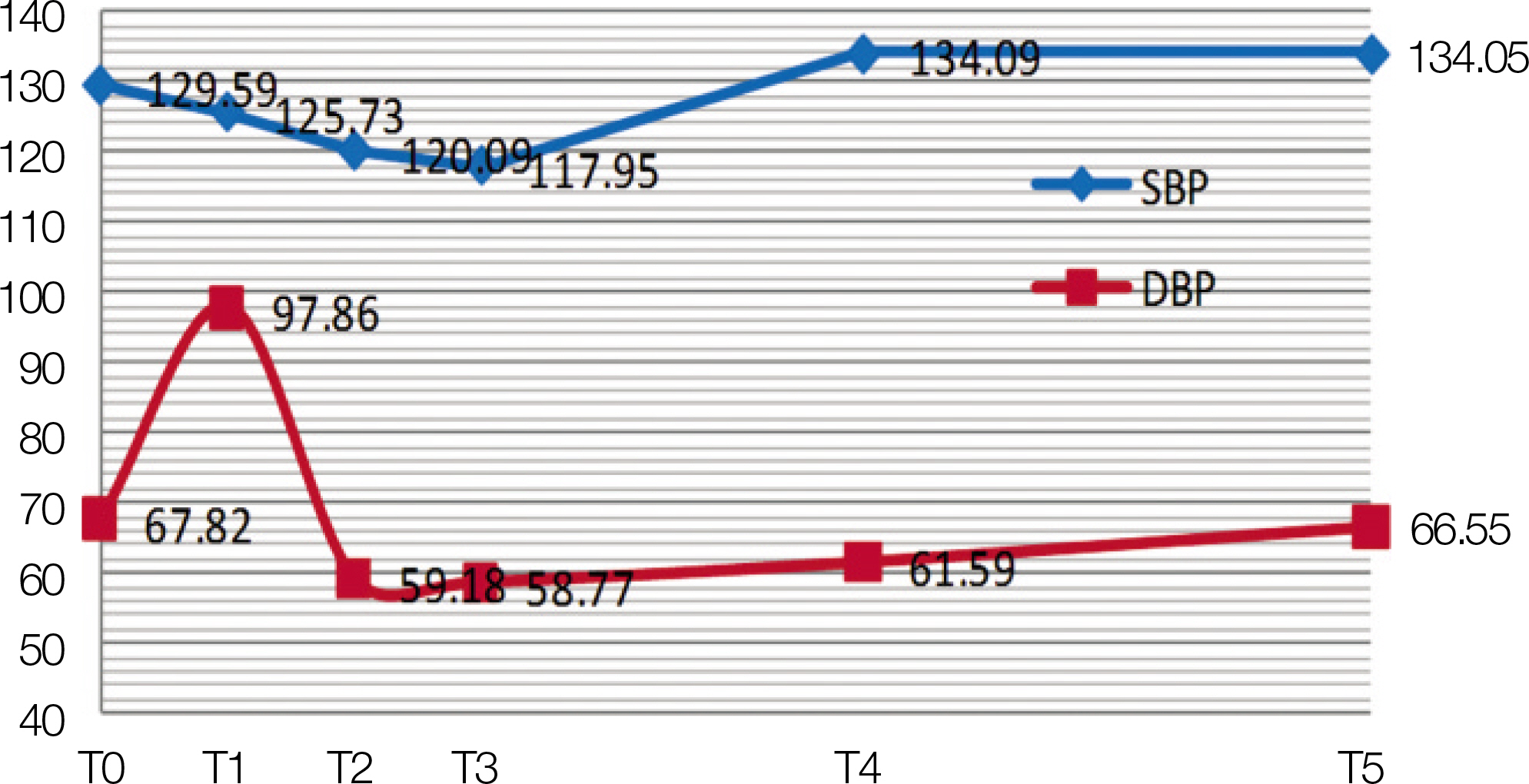
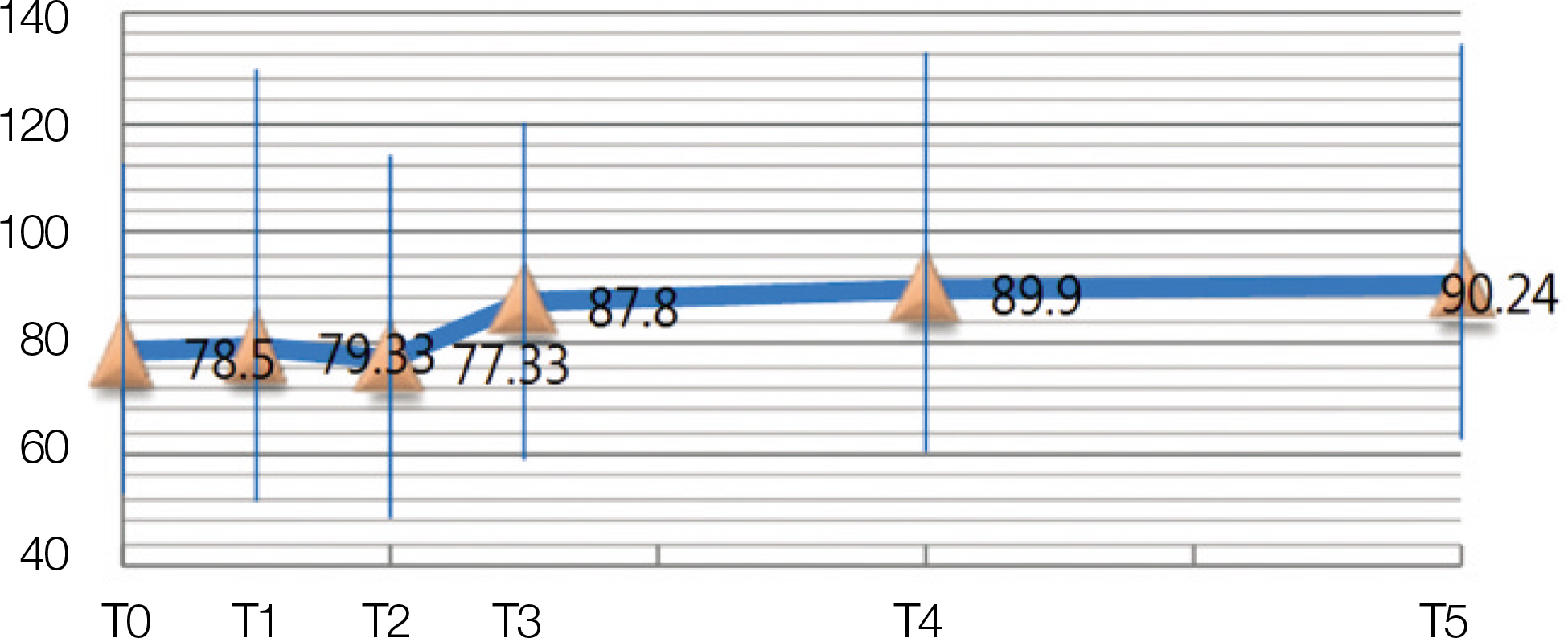
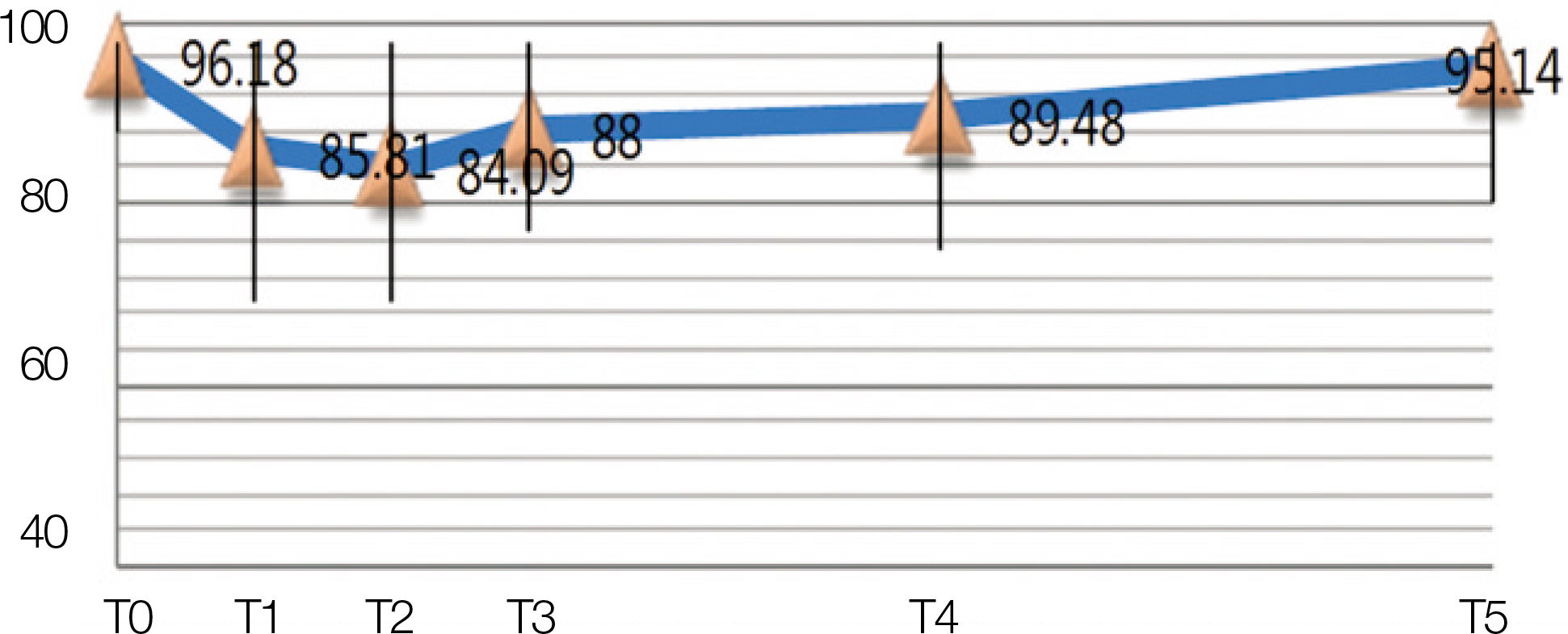
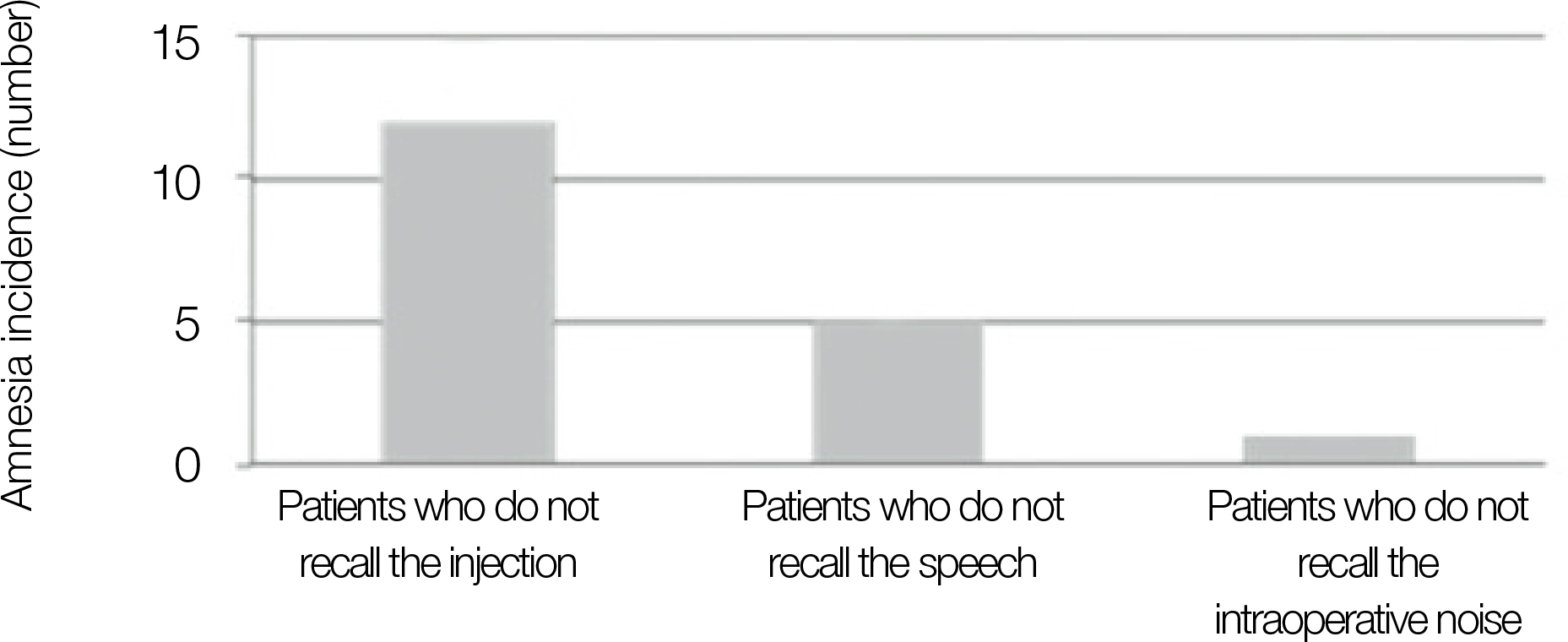
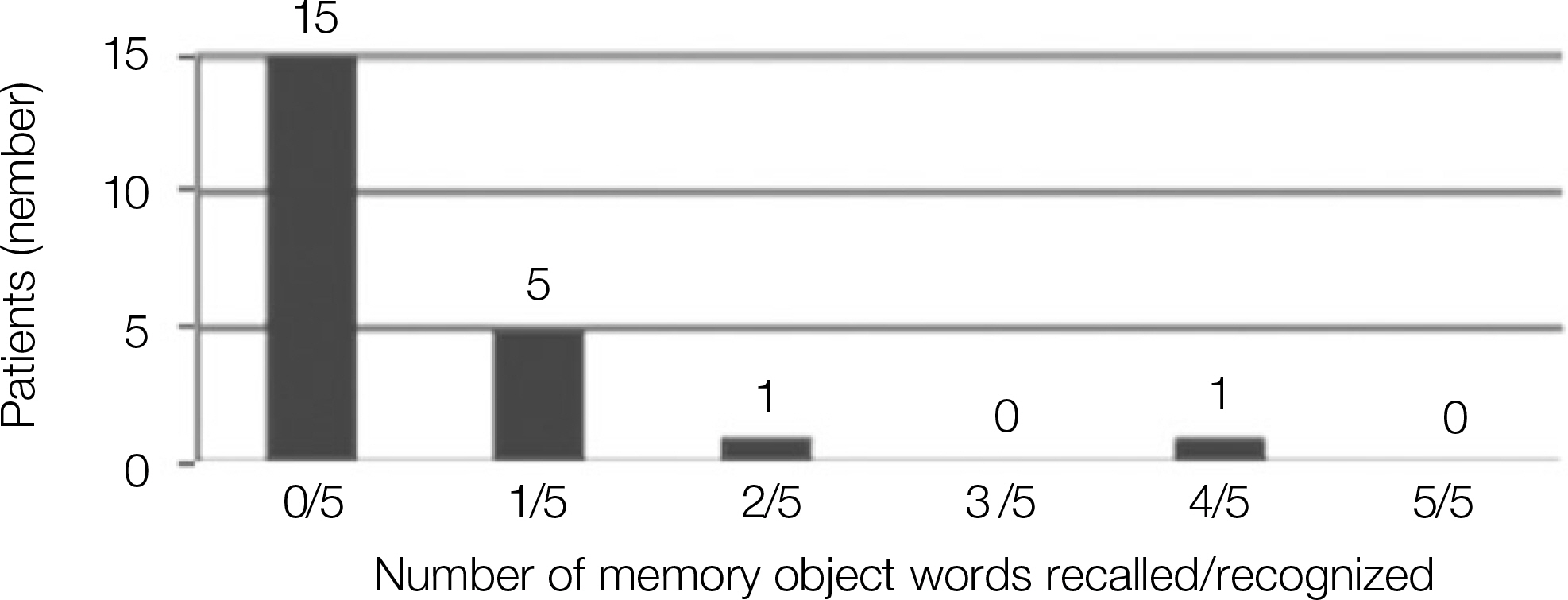
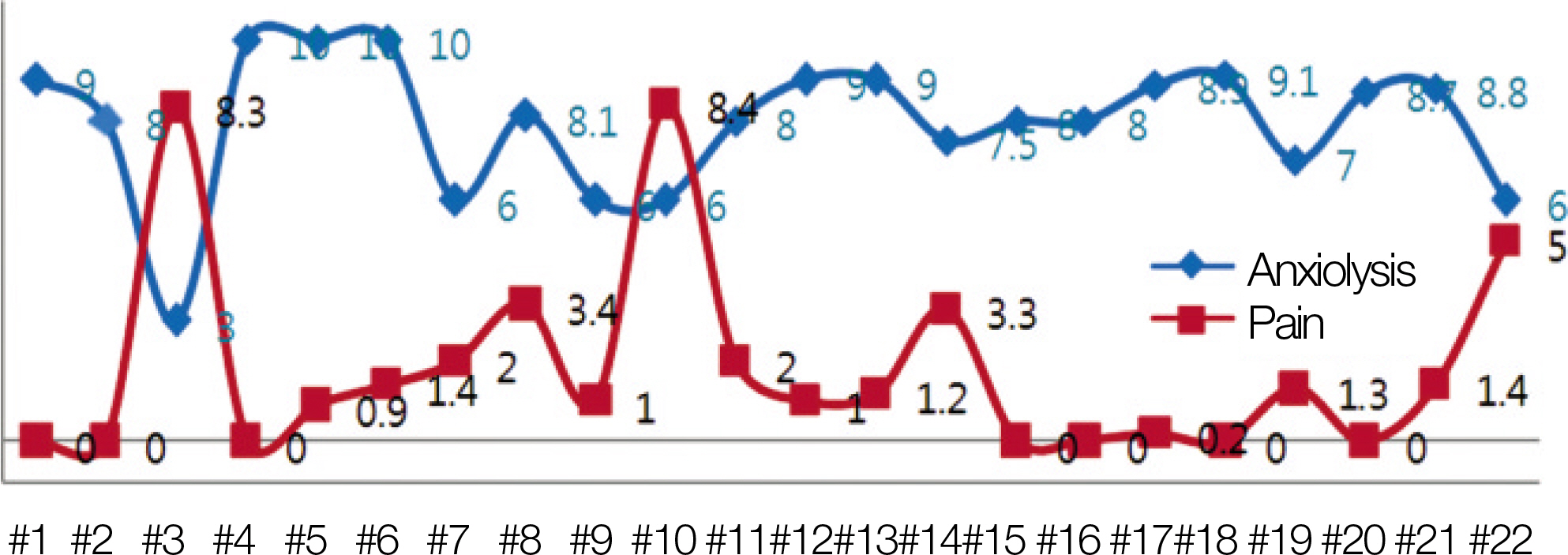
The bispectral index (BIS) decreased approximately 5 minutes after midazolam administration, but increased at the local anesthesia injection and odontomy procedure. The amnestic effect was shown effectively in the early stages of surgery.
CONCLUSION
Conscious sedation with intravenous midazolam is effective in achieving the effect of anxiolysis, analgesia and amnesia. The BIS is an objective and useful means of assessing the depth of sedation.
MeSH Terms
Figure
Reference
-
References
1. Malamed SF, Nikchevich D Jr, Block J. Anterograde amnesia as a possible postoperative complication of Midazolam as an agent for intravenous conscious sedation. Anesth Prog. 1988; 35:160–2.2. Veselis RA, Reinsel RA, Feshchenko VA. Drug-induced amnesia is a separate phenomenon from sedation: electrophysiologic evidence. Anesthesiology. 2001; 95:896–907.3. Ishiguro T, Ishiguro C, Ishiguro G, Nagawa H. Midazolam sedation for upper gastrointestinal endoscopy: comparison between the states of patients in partial and complete amnesia. Hepatogastroenterology. 2002; 49:438–40.4. Chernik DA, Gillings D, Laine H, Hendler J, Silver JM, Davidson AB, et al. Validity and reliability of the Observer's Assessment of Alertness/Sedation Scale: study with intravenous midazolam. J Clin Psychopharmacol. 1990; 10:244–51.5. Bell JK, Laasch HU, Wilbraham L, England RE, Morris JA, Martin DF. Bispectral index monitoring for conscious sedation in intervention: better, safer, faster. Clin Radiol. 2004; 59:1106–13.
Article6. Mondello E, Panasiti R, Siliotti R, Floridia D, David A, Trimarchi G. BIS and Ramsay score in critically ill patient: what future? Minerva Anestesiol. 2002; 68:37–43.7. Sigl JC, Chamoun NG. An introduction to bispectral analysis for the electroencephalogram. J Clin Monit. 1994; 10:392–404.
Article8. Coolidge T, Heaton LJ, Milgrom P. The challenge of sedation with adolescents: case studies and clinical recommendations. SAAD Dig. 2009; 25:29–36.9. Bulach R, Myles PS, Russnak M. Double-blind randomized controlled trial to determine extent of amnesia with midazolam given immediately before general anaesthesia. Br J Anaesth. 2005; 94:300–5.
Article10. Barker I, Butchart DG, Gibson J, Lawson JI, Mackenzie N. I.v. sedation for conservative dentistry. A comparison of midazolam and diazepam. Br J Anaesth. 1986; 58:371–7.11. Milgrom P, Weinstein P, Fiset L, Beirne OR. The anxiolytic effects of intravenous sedation using midazolam alone or in multiple drug techniques. J Oral Maxillofac Surg. 1994; 52:219–24. discussion 225.
Article12. Ouellette SM, Simpson C. Monitoring for intraoperative awareness. AORN J. 1998; 68:950–6. 959–61.13. Sandler NA, Hodges J, Sabino M. Assessment of recovery in patients undergoing intravenous conscious sedation using bispectral analysis. J Oral Maxillofac Surg. 2001; 59:603–11. discussion 611–2.
Article14. Sandler NA. Bispectral analysis: an objective method of assessing anesthetic depth. J Oral Maxillofac Surg. 2004; 62:1002–4.
Article15. Osborn TM, Sandler NA. The effects of preoperative anxiety on intravenous sedation. Anesth Prog. 2004; 51:46–51.16. Park JH, Lee SH, Yoon HJ. The study of conscious sedation in both mandibular 3rd molars extraction in Koreans. J Korean Assoc Maxillofac Plast Reconstr Surg. 2004; 26:563–7.17. Pharmaceutical Association of Seoul National University Hospital. Medical pharmacologic index in Seoul National University. 14th ed.Seoul: Dae Jin;2001.18. Clark WG, Brater DC, Johnson AR, Goth A. Goth's medical pharmacology. 13rd ed.St. Louis, MO.: Mosby-Year Book;1992.19. Ochs MW, Tucker MR, White RP Jr. A comparison of amnesia in outpatients sedated with midazolam or diazepam alone or in combination with fentanyl during oral surgery. J Am Dent Assoc. 1986; 113:894–7.
Article20. Berggren L, Eriksson I, Mollenholt P, Wickbom G. Sedation for fibreoptic gastroscopy: a comparative study of midazolam and diazepam. Br J Anaesth. 1983; 55:289–96.
Article21. Jang JH, Kim SM, Kim SH, Park YW. A study of the midazolam dosage on conscious sedation at the department of the oral and maxillofacial surgery. J Korean Assoc Maxillofac Plast Reconstr Surg. 2002; 24:218–25.22. Bell GW, Kelly PJ. A study of anxiety, and midazolam-induced amnesia in patients having lower third molar teeth extracted. Br J Oral Maxillofac Surg. 2000; 38:596–602.
Article23. Malamed SF. Managing medical emergencies. J Am Dent Assoc. 1993; 124:40–53.
Article24. Ong CK, Seymour RA, Tan JM. Sedation with midazolam leads to reduced pain after dental surgery. Anesth Analg. 2004; 98:1289–93.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The Effect of Fixed Dose of Flumazenil on Recovery after Sedative Endoscopy by Midazolam
- The study of conscious sedation in both mandibular 3rd molars extraction in Koreans
- Sedation at Sedation Clinic of Department of Dentistry in Hanyang University Medical Center (II)
- Considerations for submucosal midazolam administration in combination with oral and inhaled medications for sedation of pediatric dental patients
- Sedative Effect of Sublingual Midazolam after Oral Chloral Hydrate or Hydroxyzine in Children