J Korean Soc Transplant.
2016 Jun;30(2):94-97. 10.4285/jkstn.2016.30.2.94.
Tacrolimus-induced, Transplant-associated Thrombotic Microangiopathies after Lung Transplantation
- Affiliations
-
- 1Division of Pulmonology, Department of Internal Medicine, Institute of Chest Diseases, Severance Hospital, Yonsei University College of Medicine, Seoul, Korea. dobie@yuhs.ac
- 2Department of Thoracic and Cardiovascular Surgery, Yonsei University College of Medicine, Seoul, Korea.
- 3Division of Hematology, Department of Internal Medicine, Severance Hospital, Yonsei University College of Medicine, Seoul, Korea.
- KMID: 2327970
- DOI: http://doi.org/10.4285/jkstn.2016.30.2.94
Abstract
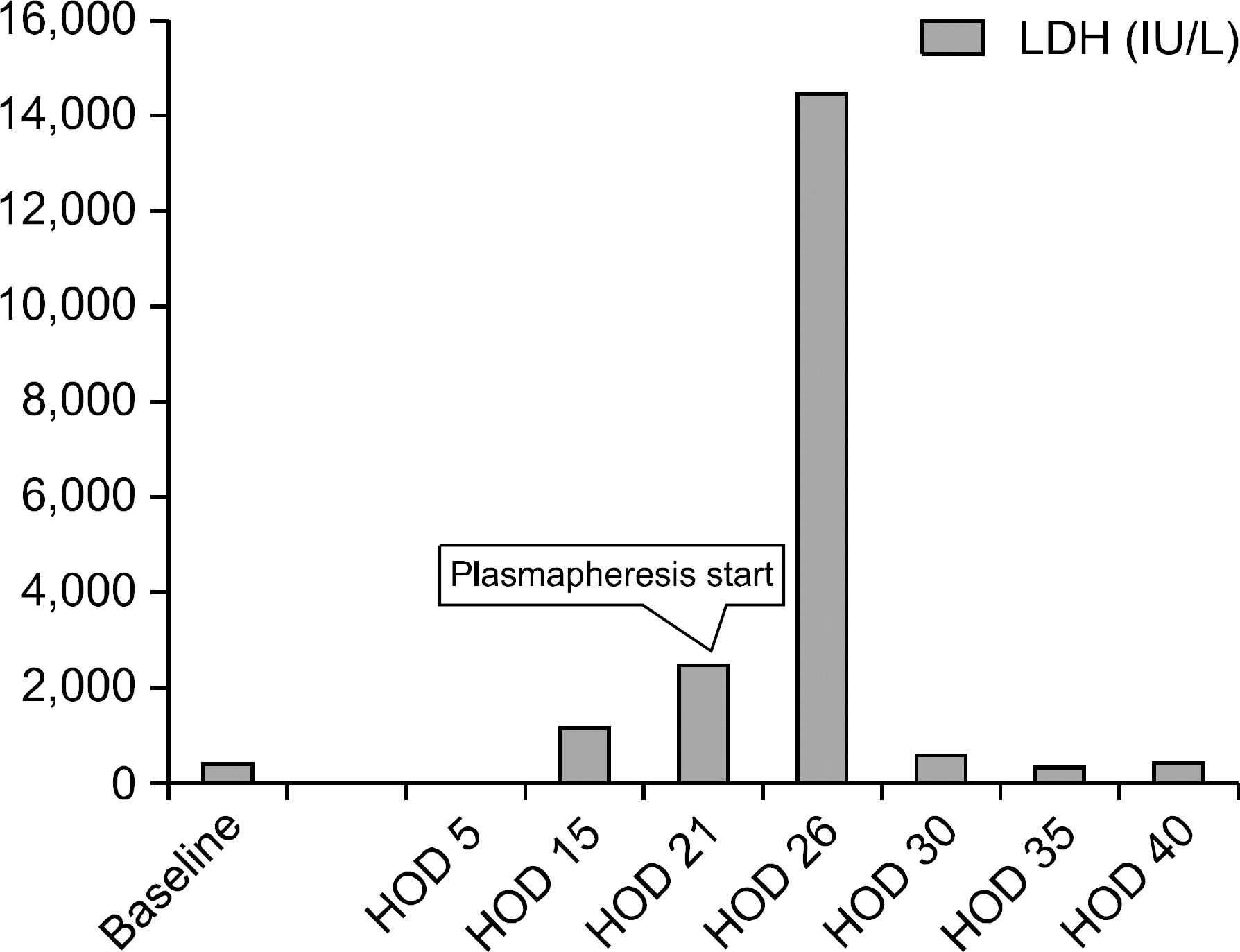
- We report a case of tacrolimus-induced transplant-associated thrombotic microangiopathies (TA-TMA) after lung transplantation. A 71-year-old man underwent lung transplantation secondary to idiopathic pulmonary fibrosis. After 4 months, he presented with abdominal discomfort and dyspnea, and was diagnosed with hemolytic anemia and thrombocytopenia. Tacrolimus was considered the cause of the TMA. Tacrolimus was stopped and several sessions of plasma exchange were performed immediately after diagnosis of TA-TMA. However, his platelet count did not normalize, gastrointestinal bleeding was recurrent, and severe pneumonia developed, following which he died. TA-TMA are rare but severe, life-threatening complications in lung transplant recipients. Therefore, the possibility of TA-TMA should be considered in posttransplant recipients.
MeSH Terms
Figure
Reference
-
1). Klintmalm G. A review of FK506: a new immunosuppressant agent for the prevention and rescue of graft rejection. Transplant Rev. 1994. 8:53–63.
Article2). Mach-Pascual S., Samii K., Beris P. Microangiopathic hemolytic anemia complicating FK506 (tacrolimus) therapy. Am J Hematol. 1996. 52:310–2.
Article3). Matsusaki T., Morimatsu H., Sato T., Sato K., Mizobuchi S., Morita K. Thrombotic microangiopathy after living-donor liver re-transplantation. J Anesth. 2010. 24:614–7.
Article4). Nakazawa Y., Hashikura Y., Urata K., Ikegami T., Terada M., Yagi H, et al. Von Willebrand factor: cleaving protease activity in thrombotic microangiopathy after living donor liver transplantation: a case report. Liver Transpl. 2003. 9:1328–33.5). Ho VT., Cutler C., Carter S., Martin P., Adams R., Horowitz M, et al. Blood and marrow transplant clinical trials network toxicity committee consensus summary: thrombotic microangiopathy after hematopoietic stem cell transplantation. Biol Blood Marrow Transplant. 2005. 11:571–5.
Article6). Trimarchi HM., Truong LD., Brennan S., Gonzalez JM., Suki WN. FK506-associated thrombotic microangiopathy: report of two cases and review of the literature. Transplantation. 1999. 67:539–44.7). Humar A., Jessurun J., Sharp HL., Gruessner RW. Hemolytic uremic syndrome in small-bowel transplant recipients: the first two case reports. Transpl Int. 1999. 12:387–90.
Article8). Nwaba A., MacQuillan G., Adams LA., Garas G., Delriviere L., Augustson B, et al. Tacrolimus-induced thrombotic microangiopathy in orthotopic liver transplant patients: case series of four patients. Intern Med J. 2013. 43:328–33.
Article9). Kojouri K., George JN. Thrombotic microangiopathy following allogeneic hematopoietic stem cell transplantation. Curr Opin Oncol. 2007. 19:148–54.
Article10). Myers JN., Shabshab SF., Burton NA., Nathan SD. Successful use of cyclosporine in a lung transplant recipient with tacrolimus-associated hemolytic uremic syndrome. J Heart Lung Transplant. 1999. 18:1024–6.11). Boyer NL., Niven A., Edelman J. Tacrolimus-associated thrombotic microangiopathy in a lung transplant recipient. BMJ Case Rep. Epub 2013 Feb 8.DOI: doi: http://dx.doi.org/10.1136/bcr-2012-007351.12). Chinen Y., Kuroda J., Ohshiro M., Shimura Y., Mizutani S., Nagoshi H, et al. Low ADAMTS-13 activity during hemorrhagic events with disseminated intravascular coagulation. Int J Hematol. 2013. 97:511–9.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Overcome of Drug Induced Thrombotic Microangiopathy after Kidney Transplantation by Using Belatacept for Maintenance Immunosuppression
- Risk of graft loss on once-daily versus twice-daily tacrolimus in kidney transplant patients: a meta-analysis
- Intestinal Thrombotic Microangiopathy after Liver Transplantation
- Two Cases of Tacrolimus-related Transplant-associated Thrombotic Microangiopathy Retinopathy after Allogenic Peripheral Blood Stem Cell Transplantation
- The comparison of coefficient of variation among once-daily and twice-daily tacrolimus in kidney transplant patients: a meta-analysis