Tuberc Respir Dis.
2012 Jan;72(1):55-58.
A Case of Mycobacterium szulgai Lung Disease in Patient with Healed Tuberculosis
- Affiliations
-
- 1Department of Pulmonary and Critical Care Medicine, Kyung Hee University Hospital at Gangdong, Kyung Hee University School of Medicine, Seoul, Korea. kumc92@naver.com
- 2Department of Pathology, Kyung Hee University Hospital at Gangdong, Kyung Hee University School of Medicine, Seoul, Korea.
- 3Department of Pulmonary and Critical Care Medicine, Jeju National University Hospital, Jeju National University School of Medicine, Jeju, Korea.
Abstract
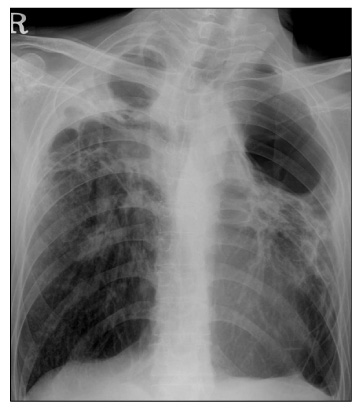
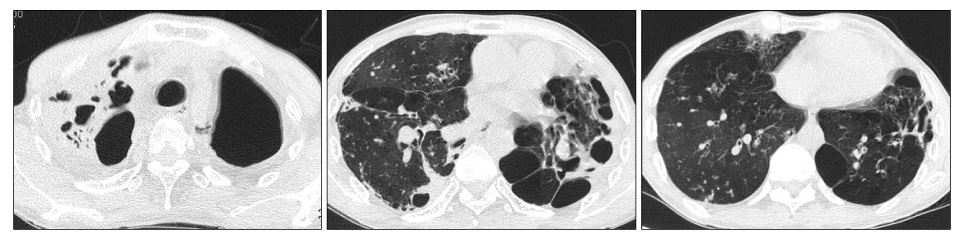
- Mycobacterium szulgai is a rare nontuberculous mycobacterium found in Korea. It is an opportunistic pathogen and is usually isolated from patients with a history of alcoholism, chronic pulmonary disease, or an immunocompromising condition. We present here a case of M. szulgai isolated from a patient with a history of pulmonary tuberculosis. A 54-year-old man was admitted with dyspnea and febrile sensation. He had a history of pulmonary tuberculosis which occurred 30 years earlier and treatment with anti-tuberculosis medication. His chest computed tomography scan showed cavitary consolidation in both upper lungs. A sputum acid-fast bacilli (AFB) smear was positive and anti-tuberculous medication was started. However, a polymerase chain reaction for mycobacterium tuberculosis was negative and anti-tuberculous medication was stopped. M. szulgai was isolated on 3 separate sputum and bronchial wash fluid AFB cultures. He was treated with clarithromycin, rifampicin, and ethambutol. After 1 month, a sputum AFB smear and culture became negative and no additional M. szulgai were isolated during a 16-month treatment.
MeSH Terms
Figure
Reference
-
1. Park YS, Lee CH, Lee SM, Yang SC, Yoo CG, Kim YW, et al. Rapid increase of non-tuberculous mycobacterial lung diseases at a tertiary referral hospital in South Korea. Int J Tuberc Lung Dis. 2010. 14:1069–1071.2. van Ingen J, Boeree MJ, de Lange WC, de Haas PE, Dekhuijzen PN, van Soolingen D. Clinical relevance of Mycobacterium szulgai in the Netherlands. Clin Infect Dis. 2008. 46:1200–1205.3. Koh WJ, Kwon OJ, Lee KS. Diagnosis and treatment of nontuberculous Mycobacterial pulmonary diseases: a Korean perspective. J Korean Med Sci. 2005. 20:913–925.4. Marks J, Jenkins PA, Tsukamura M. Mycobacterium szulgai--a new pathogen. Tubercle. 1972. 53:210–214.5. Benator DA, Kan V, Gordin FM. Mycobacterium szulgai infection of the lung: case report and review of an unusual pathogen. Am J Med Sci. 1997. 313:346–351.6. Maloney JM, Gregg CR, Stephens DS, Manian FA, Rimland D. Infections caused by Mycobacterium szulgai in humans. Rev Infect Dis. 1987. 9:1120–1126.7. Shenai S, Rodrigues C, Mehta A. Time to identify and define non-tuberculous mycobacteria in a tuberculosis-endemic region. Int J Tuberc Lung Dis. 2010. 14:1001–1008.8. Alvarez-Uria G. Lung disease caused by nontuberculous mycobacteria. Curr Opin Pulm Med. 2010. 16:251–256.9. Koh WJ, Kwon OJ, Yu CM, Jeon KM, Suh GY, Chung MP, et al. Recovery rate of nontuberculous Mycobacteria from acid-fast-bacilli smear-positive sputum specimens. Tuberc Respir Dis. 2003. 54:22–32.10. Griffith DE, Aksamit T, Brown-Elliott BA, Catanzaro A, Daley C, Gordin F, et al. An official ATS/IDSA statement: diagnosis, treatment, and prevention of nontuberculous mycobacterial diseases. Am J Respir Crit Care Med. 2007. 175:367–416.11. Kim JH, Suh JT, Park SY, Lee HJ, Lee WI. Clinical evaluation of 10 cases of nontuberculous Mycobacteria isolated from sputum. Korean J Lab Med. 2004. 24:49–52.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Mycobacterium Szulgai Pulmonary Infection: Case Report of an Uncommon Pathogen in Korea
- Recent Advances in Tuberculosis and Nontuberculous Mycobacteria Lung Disease
- Respiratory Review of 2009: Nontuberculous Mycobacterium
- A Case of Tuberculosis Verrucosa Cutis with Ulcer in a Patient with Pulmonary Tuberculosis
- A Case of Disseminated Bone Tuberculosis with Diagnosed by Bone Marrow Aspirated Filter Biopsy