Korean J Radiol.
2014 Oct;15(5):651-654. 10.3348/kjr.2014.15.5.651.
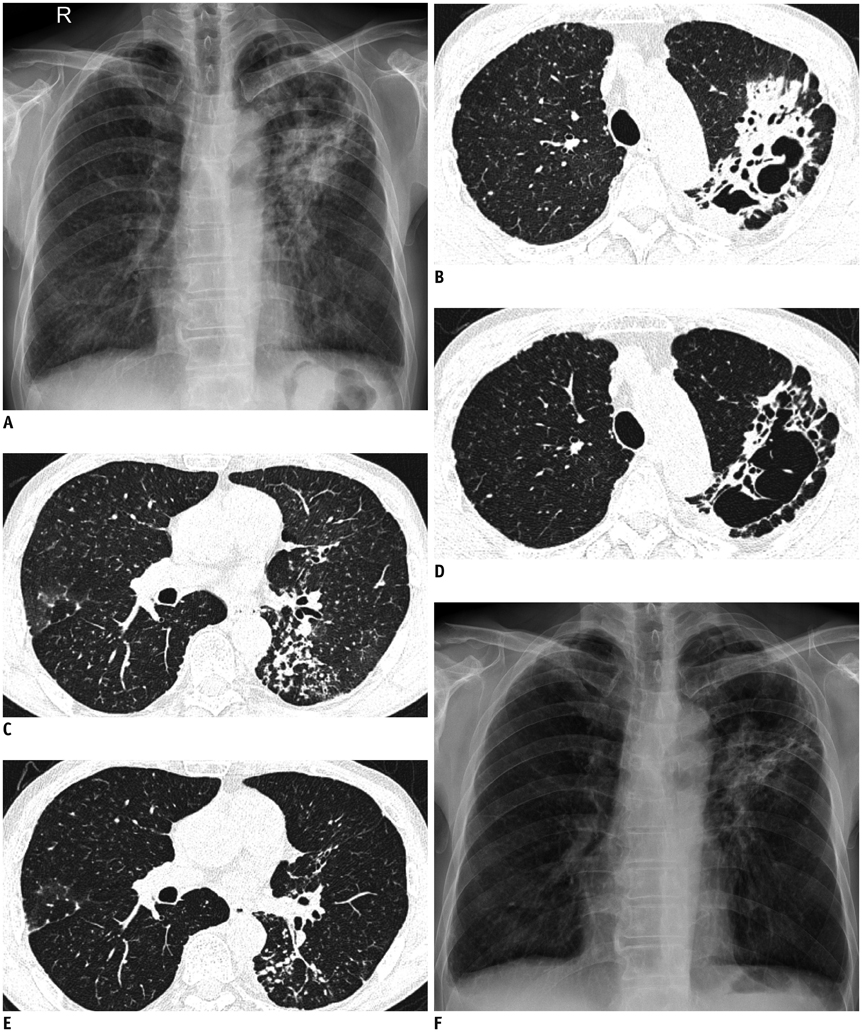
Mycobacterium Szulgai Pulmonary Infection: Case Report of an Uncommon Pathogen in Korea
- Affiliations
-
- 1Department of Radiology, Jeju National University School of Medicine, Jeju 690-767, Korea. sy7728.jeong@gmail.com
- 2Department of Internal Medicine, Jeju National University School of Medicine, Jeju 690-767, Korea.
- KMID: 1734952
- DOI: http://doi.org/10.3348/kjr.2014.15.5.651
Abstract
- Mycobacterium szulgai (M. szulgai) is an unusual pathogen in a human non-tuberculous mycobacterial infection. Pulmonary infection due to M. szulgai may be clinically and radiologically confused with active pulmonary tuberculosis. In contrast to other non-tuberculous mycobacteria, M. szulgai infection is well controlled by combination antimycobacterial therapy. Most of the previously reported cases of M. szulgai pulmonary infection showed cavitary upper lobe infiltrates. We herein describe a case of pulmonary M. szulgai infection that shows clinical and radiological presentations similar to active pulmonary tuberculosis.
MeSH Terms
Figure
Reference
-
1. Marks J, Jenkins PA, Tsukamura M. Mycobacterium szulgai--a new pathogen. Tubercle. 1972; 53:210–214.2. van Ingen J, Boeree MJ, de Lange WC, de Haas PE, Dekhuijzen PN, van Soolingen D. Clinical relevance of Mycobacterium szulgai in The Netherlands. Clin Infect Dis. 2008; 46:1200–1205.3. Griffith DE, Aksamit T, Brown-Elliott BA, Catanzaro A, Daley C, Gordin F, et al. An official ATS/IDSA statement: diagnosis, treatment, and prevention of nontuberculous mycobacterial diseases. Am J Respir Crit Care Med. 2007; 175:367–416.4. Sánchez-Alarcos JM, De Miguel-Díez J, Bonilla I, Sicilia JJ, Alvarez-Sala JL. Pulmonary infection due to Mycobacterium szulgai. Respiration. 2003; 70:533–536.5. Ohta H, Miyauchi E, Ebina M, Nukiwa T. A case of cutaneous infection caused by mycobacterium szulgai with progression to acute respiratory distress syndrome. Clin Med Insights Case Rep. 2011; 4:29–33.6. Randhawa K, Smethurst P, Soo Hoo GW. Nine-year progression of untreated pulmonary Mycobacterium szulgai infection. South Med J. 2010; 103:828–830.7. Koh WJ, Kwon OJ, Lee KS. Nontuberculous mycobacterial pulmonary diseases in immunocompetent patients. Korean J Radiol. 2002; 3:145–157.8. Yoo H, Jeon K, Kim SY, Jeong BH, Park HY, Ki CS, et al. Clinical significance of Mycobacterium szulgai isolates from respiratory specimens. Scand J Infect Dis. 2014; 46:169–174.9. van Ingen J. Diagnosis of nontuberculous mycobacterial infections. Semin Respir Crit Care Med. 2013; 34:103–109.10. Piersimoni C, Scarparo C. Pulmonary infections associated with non-tuberculous mycobacteria in immunocompetent patients. Lancet Infect Dis. 2008; 8:323–334.11. Polverosi R, Guarise A, Balestro E, Carloni A, Dalpiaz G, Feragalli B. High-resolution CT of nontuberculous mycobacteria pulmonary infection in immunocompetent, non-HIV-positive patients. Radiol Med. 2010; 115:191–204.12. Erasmus JJ, McAdams HP, Farrell MA, Patz EF Jr. Pulmonary nontuberculous mycobacterial infection: radiologic manifestations. Radiographics. 1999; 19:1487–1505.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Mycobacterium szulgai Lung Disease in Patient with Healed Tuberculosis
- Acute pneumonia caused by mycobacterium intracellulare
- Pulmonary infection with Mycobacterium celatum in immunocompetent host: The first case report in Korea
- A Case of Pulmonary and Endobronchial Mycobacterium avium Infection Presenting as an Acute Pneumonia in an Immunocompetent Patient
- A case of Idiopathic CD4+ T-Lymphocytopenia with disseminated Mycobacterium kansasii infection and Pulmonary alveolar proteinosis