Tuberc Respir Dis.
2011 Jun;70(6):474-481.
The Survival Rate of Korean Patients with COPD with or without Acute Exacerbations
- Affiliations
-
- 1Division of Allergy and Respiratory Medicine, Soonchunhyang University Seoul Hospital, Soonchunhyang University College of Medicine, Seoul, Korea.
- 2Division of Allergy and Respiratory Medicine, Soonchunhyang University Bucheon Hospital, Soonchunhyang University College of Medicine, Bucheon, Korea. mdcspark@unitel.co.kr
- 3Division of Allergy and Respiratory Medicine, Soonchunhyang University Cheonan Hospital, Soonchunhyang University College of Medicine, Cheonan, Korea.
- 4Genome Research Center for Allergy and Respiratory Diseases, Soonchunhyang University Bucheon Hospital, Soonchunhyang University College of Medicine, Bucheon, Korea.
Abstract
- BACKGROUND
Chronic obstructive pulmonary disease (COPD) is characterized by air flow limitation, which is one of the leading causes of mortality worldwide. There have been many studies on survival rates in the world literature, but there have been few reports regarding the survival rate in Korean patients with COPD. Acute exacerbation is regarded as a risk factor for mortality in patients with COPD. The purpose of this study was to investigate the survival rate and the effect of acute exacerbations on the survival rate of Korean patients with COPD.
METHODS
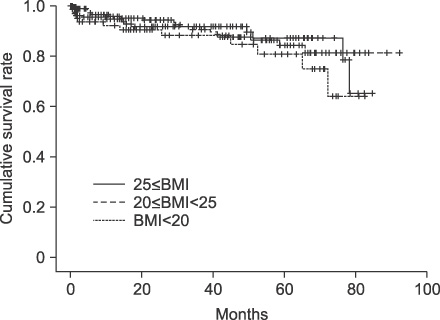
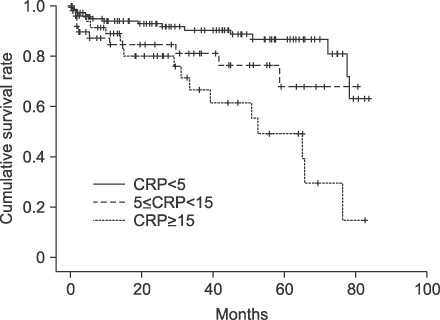
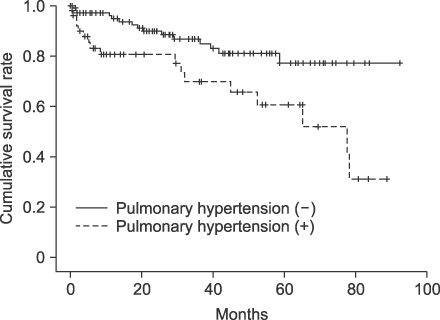
A total of 502 COPD patients who were diagnosed on the basis of history and lung function tests were enrolled in this study. The frequency of acute exacerbations, body mass index (BMI), C-reactive protein (CRP) and pulmonary hypertension were analyzed.
RESULTS
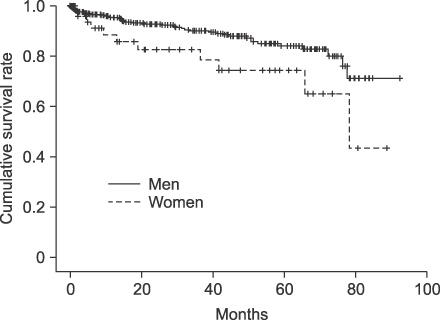
The 3- and 5-year survival rates were 98% and 83%, respectively. The median survival time was 78 months. The median survival time was 55 months in 322 patients with one or more acute exacerbations. The 3- and 5-year survival rates were significantly lower in the 322 patients with one or more acute exacerbations than in those without any. The mortality rate was significantly higher in patients with CRP >3 mg/L than in those with CRP < or =3 mg/L (p<0.005); it was significantly higher in patients with pulmonary hypertension than in those without it (p<0.01).
CONCLUSION
Because the 5-year survival rate is 83% in Korean patients with COPD, the management of stable patients with COPD should focus on the prevention of acute exacerbations.
MeSH Terms
Figure
Reference
-
1. Rabe KF, Hurd S, Anzueto A, Barnes PJ, Buist SA, Calverley P, et al. Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease: GOLD executive summary. Am J Respir Crit Care Med. 2007. 176:532–555.2. Chapman KR, Mannino DM, Soriano JB, Vermeire PA, Buist AS, Thun MJ, et al. Epidemiology and costs of chronic obstructive pulmonary disease. Eur Respir J. 2006. 27:188–207.3. Kim DS, Kim YS, Jung KS, Chang JH, Lim CM, Lee JH, et al. Prevalence of chronic obstructive pulmonary disease in Korea: a population-based spirometry survey. Am J Respir Crit Care Med. 2005. 172:842–847.4. Nishimura K, Izumi T, Tsukino M, Oga T. Dyspnea is a better predictor of 5-year survival than airway obstruction in patients with COPD. Chest. 2002. 121:1434–1440.5. Calverley PM, Anderson JA, Celli B, Ferguson GT, Jenkins C, Jones PW, et al. Salmeterol and fluticasone propionate and survival in chronic obstructive pulmonary disease. N Engl J Med. 2007. 356:775–789.6. Patil SP, Krishnan JA, Lechtzin N, Diette GB. In-hospital mortality following acute exacerbations of chronic obstructive pulmonary disease. Arch Intern Med. 2003. 163:1180–1186.7. Ai-Ping C, Lee KH, Lim TK. In-hospital and 5-year mortality of patients treated in the ICU for acute exacerbation of COPD: a retrospective study. Chest. 2005. 128:518–524.8. Berkius J, Nolin T, Mårdh C, Karlström G, Walther SM. Swedish Intensive Care Registry. Characteristics and long-term outcome of acute exacerbations in chronic obstructive pulmonary disease: an analysis of cases in the Swedish Intensive Care Registry during 2002-2006. Acta Anaesthesiol Scand. 2008. 52:759–765.9. Gerardi D, ZuWallack R. Non-pulmonary factors affecting survival in patients completing pulmonary rehabilitation. Monaldi Arch Chest Dis. 2001. 56:331–335.10. Ringbaek T, Seersholm N, Viskum K. Standardised mortality rates in females and males with COPD and asthma. Eur Respir J. 2005. 25:891–895.11. Dahl M, Vestbo J, Lange P, Bojesen SE, Tybjaerg-Hansen A, Nordestgaard BG. C-reactive protein as a predictor of prognosis in chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 2007. 175:250–255.12. American Thoracic Society. Standardization of sirometry, 1994 update. Am J Respir Crit Care Med. 1995. 152:1107–1136.13. Postma DS, Gimeno F, van der Weele LT, Sluiter HJ. Assessment of ventilatory variables in survival prediction of patients with chronic airflow obstruction: the importance of reversibility. Eur J Respir Dis. 1985. 67:360–368.14. Vestbo J, Prescott E, Lange P, Schnohr P, Jensen G. Vital prognosis after hospitalization for COPD: a study of a random population sample. Respir Med. 1998. 92:772–776.15. Kanner RE, Renzetti AD Jr, Klauber MR, Smith CB, Golden CA. Variables associated with changes in spirometry in patients with obstructive lung diseases. Am J Med. 1979. 67:44–50.16. Monto AS, Higgins MW, Ross HW. The Tecumseh study of respiratory illness. VIII. Acute infection in chronic respiratory disease and comparison groups. Am Rev Respir Dis. 1975. 111:27–36.17. Burge PS, Calverley PM, Jones PW, Spencer S, Anderson JA, Maslen TK. Randomised, double blind, placebo controlled study of fluticasone propionate in patients with moderate to severe chronic obstructive pulmonary disease: the ISOLDE trial. BMJ. 2000. 320:1297–1303.18. Soler-Cataluña JJ, Martínez-García MA, Román Sánchez P, Salcedo E, Navarro M, Ochando R. Severe acute exacerbations and mortality in patients with chronic obstructive pulmonary disease. Thorax. 2005. 60:925–931.19. Boman C, Forsberg B, Sandström T. Shedding new light on wood smoke: a risk factor for respiratory health. Eur Respir J. 2006. 27:446–447.20. Ezzati M. Indoor air pollution and health in developing countries. Lancet. 2005. 366:104–106.21. Bateman ED, Hurd SS, Barnes PJ, Bousquet J, Drazen JM, FitzGerald M, et al. Global strategy for asthma management and prevention: GINA executive summary. Eur Respir J. 2008. 31:143–178.22. Traver GA, Cline MG, Burrows B. Predictors of mortality in chronic obstructive pulmonary disease. A 15-year follow-up study. Am Rev Respir Dis. 1979. 119:895–902.23. Wouters EF. Local and systemic inflammation in chronic obstructive pulmonary disease. Proc Am Thorac Soc. 2005. 2:26–33.24. Pinto-Plata VM, Müllerova H, Toso JF, Feudjo-Tepie M, Soriano JB, Vessey RS, et al. C-reactive protein in patients with COPD, control smokers and non-smokers. Thorax. 2006. 61:23–28.25. de Torres JP, Cordoba-Lanus E, López-Aguilar C, Muros de Fuentes M, Montejo de Garcini A, Aguirre-Jaime A, et al. C-reactive protein levels and clinically important predictive outcomes in stable COPD patients. Eur Respir J. 2006. 27:902–907.26. de Torres JP, Pinto-Plata V, Casanova C, Mullerova H, Córdoba-Lanús E, Muros de Fuentes M, et al. C-reactive protein levels and survival in patients with moderate to very severe COPD. Chest. 2008. 133:1336–1343.27. Gosker HR, Wouters EF, van der Vusse GJ, Schols AM. Skeletal muscle dysfunction in chronic obstructive pulmonary disease and chronic heart failure: underlying mechanisms and therapy perspectives. Am J Clin Nutr. 2000. 71:1033–1047.28. Schols AM, Slangen J, Volovics L, Wouters EF. Weight loss is a reversible factor in the prognosis of chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 1998. 157:1791–1797.29. Landbo C, Prescott E, Lange P, Vestbo J, Almdal TP. Prognostic value of nutritional status in chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 1999. 160:1856–1861.30. Vestbo J, Prescott E, Almdal T, Dahl M, Nordestgaard BG, Andersen T, et al. Body mass, fat-free body mass, and prognosis in patients with chronic obstructive pulmonary disease from a random population sample: findings from the Copenhagen City Heart Study. Am J Respir Crit Care Med. 2006. 173:79–83.31. Nakano Y, Muro S, Sakai H, Hirai T, Chin K, Tsukino M, et al. Computed tomographic measurements of airway dimensions and emphysema in smokers. Correlation with lung function. Am J Respir Crit Care Med. 2000. 162:1102–1108.32. Rothpearl A, Varma AO, Goodman K. Radiographic measures of hyperinflation in clinical emphysema. Discrimination of patients from controls and relationship to physiologic and mechanical lung function. Chest. 1988. 94:907–913.33. Jung EJ, Kim YK, Lee YM, Kim KU, Uh S, Kim YH, et al. The Correlation of dyspnea and radiologic quantity in patients with COPD. Tuberc Respir Dis. 2009. 66:288–294.34. Machado MC, Krishnan JA, Buist SA, Bilderback AL, Fazolo GP, Santarosa MG, et al. Sex differences in survival of oxygen-dependent patients with chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 2006. 174:524–529.35. Gonzalez AV, Suissa S, Ernst P. Gender differences in survival following hospitalisation for COPD. Thorax. 2011. 66:38–42.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- When is LABA/LAMA Better than LAMA in GOLD Group B or D Patients for Reducing Acute Exacerbations of COPD?
- Pharmacologic Therapies for Preventing Chronic Obstructive Pulmonary Disease Exacerbations: A Comprehensive Review
- Predictors of Long-term Mortality after Hospitalization for Acute Exacerbation of COPD
- Sputum Inflammometry to Manage Chronic Obstructive Pulmonary Disease Exacerbations: Beyond Guidelines
- Bacterial etiology of acute exacerbations of chronic obstructive pulmonary disease in hospitalized patients