Tuberc Respir Dis.
2011 May;70(5):416-422.
Recent 10 Years' Trend Analysis of Inhaled Corticosteroids Prescription Rate and Severe Exacerbation Rate in Asthma Patients
- Affiliations
-
- 1Department of Pulmonary and Critical Care Medicine, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea. ymoh55@amc.seoul.kr
- 2Department of Allergy and Clinical Immunology, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea.
- 3Department of Radiology, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea.
- 4Asthma Center, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea.
Abstract
- BACKGROUND
Inhaled corticosteroids (ICSs) are the most essential medication for asthma control. Many reports suggest that the usage of ICSs improves not only the control of asthma symptoms but also prevents exacerbation. We investigated whether increases in ICS prescriptions are associated with decreases in asthma exacerbation in the clinical practice setting.
METHODS
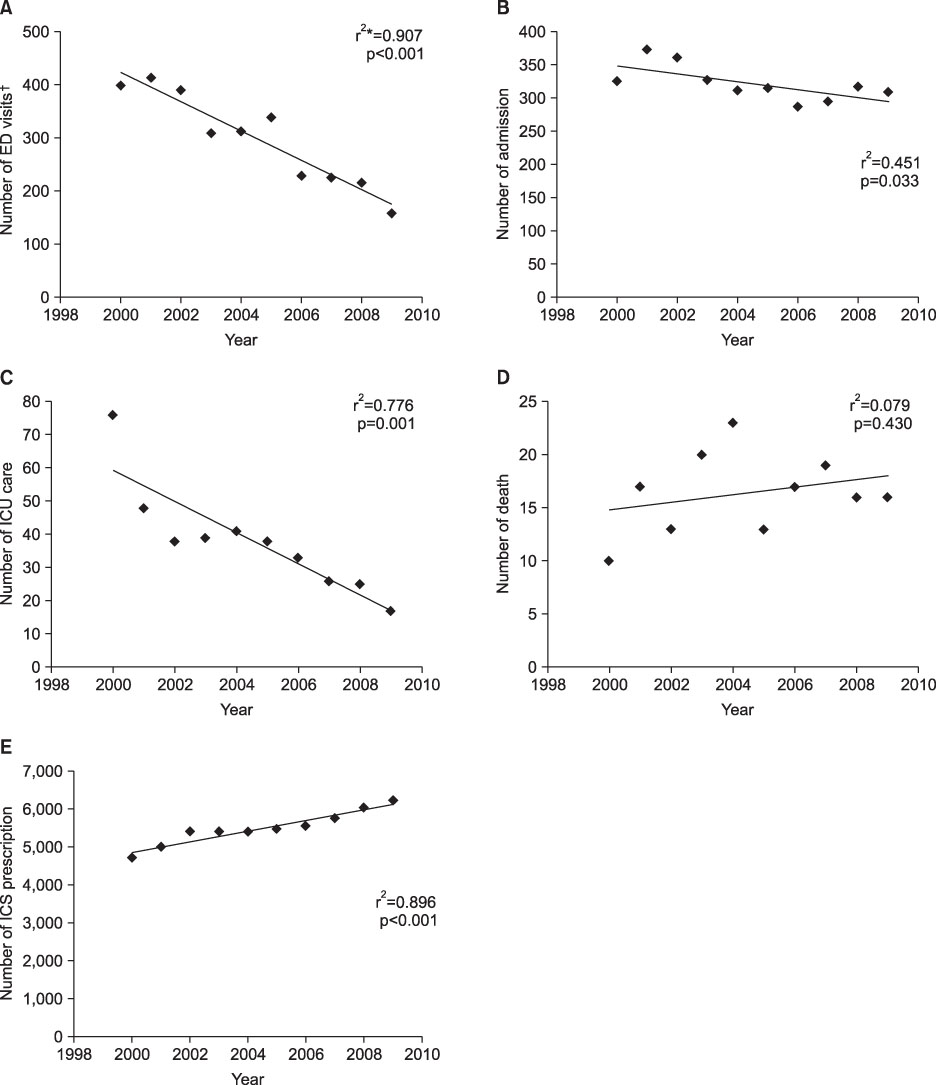
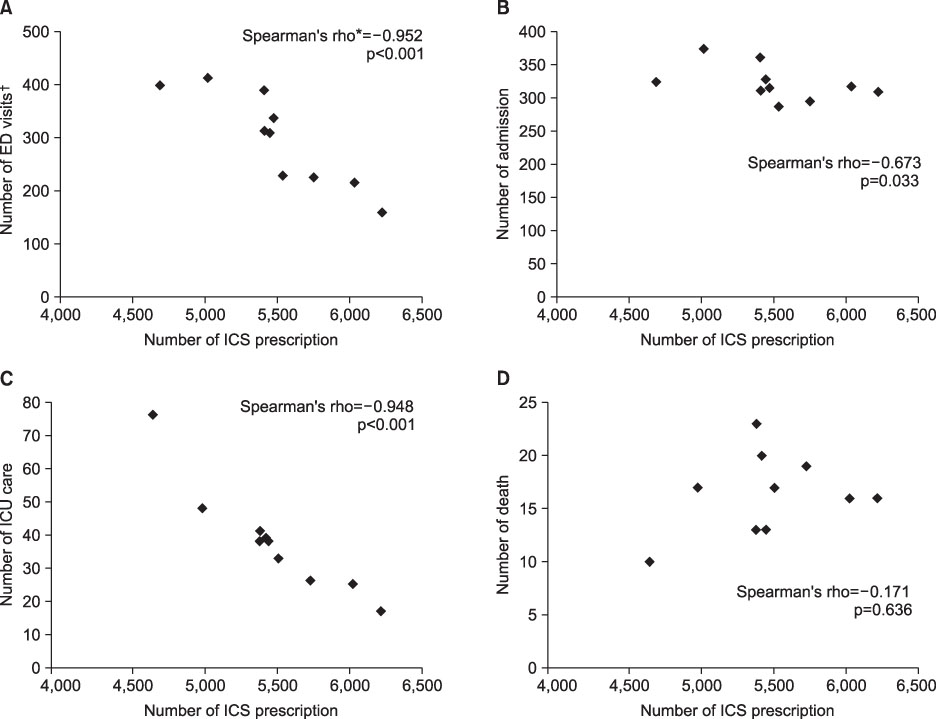
We retrospectively analyzed the database of adult asthma patients who had visited a tertiary referral hospital, the Asan Medical Center between January 2000 and December 2009. The number of emergency department (ED) visits, admissions, intensive care unit (ICU) care, deaths, and ICS prescriptions were analyzed to evaluate the time trend of asthma exacerbation as a function of the ICS prescription rate during the ten years.
RESULTS
The numbers of ED visits, admissions, and episodes of ICU care decreased during the ten years (p<0.001, p=0.033, p=0.001, respectively) while the number of ICS prescriptions increased (p<0.001). We found a correlation between the number of ICS prescriptions and the number of ED visits, admissions, or ICU care. For these outcomes, the correlation coefficients were r=-0.952, p<0.001; r=-0.673, p=0.033; r=-0.948, p<0.001, respectively.
CONCLUSION
The number of ICS prescriptions increased during the past ten years while the number of asthma exacerbations decreased. Our results also showed a negative correlation between the ICS prescription rate and asthma exacerbation in the clinical practice setting. In other words, an increase in ICS prescription may be a major cause of a decrease in asthma exacerbations.
Keyword
MeSH Terms
Figure
Reference
-
1. Global Initiative for Asthma (GINA). Global strategy for asthma management and prevention, updated 2010 [Internet]. c2010. cited 2011 May 13. Capetown, South Africa: GINA;Available from: http://www.ginasthma.org/download.asp?intId=430.2. Barnes PJ. How corticosteroids control inflammation: Quintiles Prize Lecture 2005. Br J Pharmacol. 2006. 148:245–254.3. Juniper EF, Kline PA, Vanzieleghem MA, Ramsdale EH, O'Byrne PM, Hargreave FE. Effect of long-term treatment with an inhaled corticosteroid (budesonide) on airway hyperresponsiveness and clinical asthma in nonsteroid-dependent asthmatics. Am Rev Respir Dis. 1990. 142:832–836.4. Haahtela T, Järvinen M, Kava T, Kiviranta K, Koskinen S, Lehtonen K, et al. Comparison of a beta 2-agonist, terbutaline, with an inhaled corticosteroid, budesonide, in newly detected asthma. N Engl J Med. 1991. 325:388–392.5. van Essen-Zandvliet EE, Hughes MD, Waalkens HJ, Duiverman EJ, Pocock SJ, Kerrebijn KF. The Dutch Chronic Non-specific Lung Disease Study Group. Effects of 22 months of treatment with inhaled corticosteroids and/or beta-2-agonists on lung function, airway responsiveness, and symptoms in children with asthma. Am Rev Respir Dis. 1992. 146:547–554.6. Pauwels RA, Löfdahl CG, Postma DS, Tattersfield AE, O'Byrne P, Barnes PJ, et al. Formoterol and Corticosteroids Establishing Therapy (FACET) International Study Group. Effect of inhaled formoterol and budesonide on exacerbations of asthma. N Engl J Med. 1997. 337:1405–1411.7. Ernst P, Spitzer WO, Suissa S, Cockcroft D, Habbick B, Horwitz RI, et al. Risk of fatal and near-fatal asthma in relation to inhaled corticosteroid use. JAMA. 1992. 268:3462–3464.8. Donahue JG, Weiss ST, Livingston JM, Goetsch MA, Greineder DK, Platt R. Inhaled steroids and the risk of hospitalization for asthma. JAMA. 1997. 277:887–891.9. Barnes PJ. Current issues for establishing inhaled corticosteroids as the antiinflammatory agents of choice in asthma. J Allergy Clin Immunol. 1998. 101:S427–S433.10. Blais L, Suissa S, Boivin JF, Ernst P. First treatment with inhaled corticosteroids and the prevention of admissions to hospital for asthma. Thorax. 1998. 53:1025–1029.11. Blais L, Ernst P, Boivin JF, Suissa S. Inhaled corticosteroids and the prevention of readmission to hospital for asthma. Am J Respir Crit Care Med. 1998. 158:126–132.12. Suissa S, Ernst P, Benayoun S, Baltzan M, Cai B. Low-dose inhaled corticosteroids and the prevention of death from asthma. N Engl J Med. 2000. 343:332–336.13. Davidsen JR, Søndergaard J, Hallas J, Siersted HC, Lykkegaard J, Andersen M. Increased use of inhaled corticosteroids among young Danish adult asthmatics: an observational study. Respir Med. 2010. 104:1817–1824.14. Rabe KF, Vermeire PA, Soriano JB, Maier WC. Clinical management of asthma in 1999: the Asthma Insights and Reality in Europe (AIRE) study. Eur Respir J. 2000. 16:802–807.15. Partridge MR, van der Molen T, Myrseth SE, Busse WW. Attitudes and actions of asthma patients on regular maintenance therapy: the INSPIRE study. BMC Pulm Med. 2006. 6:13.16. Cazzoletti L, Marcon A, Janson C, Corsico A, Jarvis D, Pin I, et al. Asthma control in Europe: a real-world evaluation based on an international population-based study. J Allergy Clin Immunol. 2007. 120:1360–1367.17. Backer V, Nolte H, Pedersen L, Dam N, Harving H. Unawareness and undertreatment of asthma: follow-up in a different geographic area in Denmark. Allergy. 2009. 64:1179–1184.18. Kaplan A, Ryan D. The role of budesonide/formoterol for maintenance and relief in the management of asthma. Pulm Pharmacol Ther. 2010. 23:88–96.19. Mun JS, Choi IS, Sim MK. Recent trend in prevalence and severity of acute asthma in an emergency room. Korean J Asthma Allergy Clin Immunol. 2005. 25:284–290.20. Russo MJ, McConnochie KM, McBride JT, Szilagyi PG, Brooks AM, Roghmann KJ. Increase in admission threshold explains stable asthma hospitalization rates. Pediatrics. 1999. 104:454–462.21. Peat JK, van den Berg RH, Mellis CM, Leeder SR, Woolcock AJ. Changes in the prevalence of asthma and allergy in Australian children 1982-1992. Am Rev Respir Dis. 1993. 147:A800.22. International Consensus Report on Diagnosis and Management of Asthma (NIH publication 92-3091). 1992. Bethesda, MD: US Department of Health and Human Services, Public Health Service, National Institutes of Health.23. Shin TS, Lee GJ, Yoon HS. A survey of the distribution of allergic diseases in primary schoolchildren. Allergy. 1990. 10:201–212.24. Kemp A, Björkstén B. Immune deviation and the hygiene hypothesis: a review of the epidemiological evidence. Pediatr Allergy Immunol. 2003. 14:74–80.25. Suh JK, Lee SR, Lee SY, Lee SH, Cho JY, Shim JJ, et al. Clinical Characteristics of Asthmatic Patients Who Visited Emergency Room. Tuberc Respir Dis. 1997. 44:290–297.26. Wennergren G, Kristjánsson S, Strannegård IL. Decrease in hospitalization for treatment of childhood asthma with increased use of antiinflammatory treatment, despite an increase in prevalence of asthma. J Allergy Clin Immunol. 1996. 97:742–748.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- An experimental asthma exacerbation following discontinuation of inhaled corticosteroids treatment in patients with controlled asthma
- Clinical outcomes after recovery from severe asthma exacerbation: the third report
- Inhaled Corticosteroids Is Not Associated with the Risk of Pneumonia in Asthma
- Expert consensus on oral corticosteroid use and tapering in severe asthma management
- The effect of Combination Therapy of Inhaled Corticosteroids and Long-acting Beta2-agonists on Acute Exacerbation in Moderate to Severe COPD Patients