Tuberc Respir Dis.
2011 Jan;70(1):36-42.
Evaluation of Respiratory Parameters in Patients with Acute Lung Injury Receiving Adaptive Support Ventilation
- Affiliations
-
- 1Department of Pulmonary and Critical Care Medicine, Ajou University School of Medicine, Suwon, Korea. parkkj@ajou.ac.kr
Abstract
- BACKGROUND
Adaptive support ventilation (ASV), an automated closed-loop ventilation mode, adapts to the mechanical characteristics of the respiratory system by continuous measurement and adjustment of the respiratory parameters. The adequacy of ASV was evaluated in the patients with acute lung injury (ALI).
METHODS
A total of 36 patients (19 normal lungs and 17 ALIs) were enrolled. The patients' breathing patterns and respiratory mechanics parameters were recorded under the passive ventilation using the ASV mode.
RESULTS
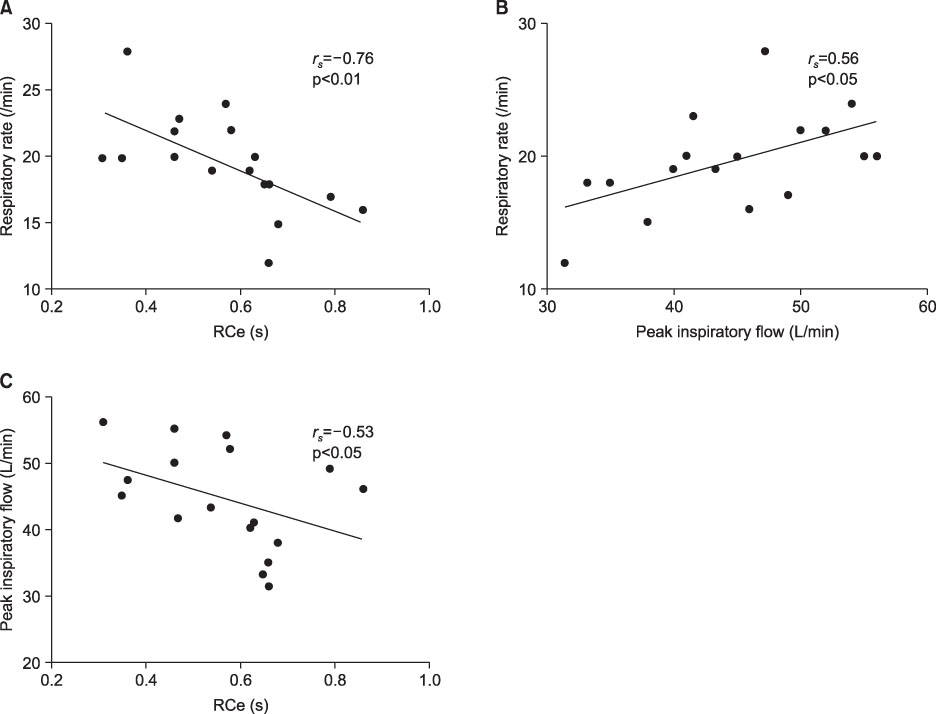
The ALI patients showed lower tidal volumes and higher respiratory rates (RR) compared to patients with normal lungs (7.1+/-0.9 mL/kg vs. 8.6+/-1.3 mL/kg IBW; 19.7+/-4.8 b/min vs. 14.6+/-4.6 b/min; p<0.05, respectively). The expiratory time constant (RCe) was lower in ALI patients than in those with normal lungs, and the expiratory time/RCe was maintained above 3 in both groups. In all patients, RR was correlated with RCe and peak inspiratory flow (rs=-0.40; rs=0.43; p<0.05, respectively). In ALI patients, significant correlations were found between RR and RCe (rs=-0.76, p<0.01), peak inspiratory flow and RR (rs=-0.53, p<0.05), and RCe and peak inspiratory flow (rs=-0.53, p<0.05).
CONCLUSION
ASV was found to operate adequately according to the respiratory mechanical characteristics in the ALI patients. Discrepancies with the ARDS Network recommendations, such as a somewhat higher tidal volume, have yet to be addressed in further studies.
Keyword
MeSH Terms
Figure
Reference
-
1. Otis AB, Fenn WO, Rahn H. Mechanics of breathing in man. J Appl Physiol. 1950. 2:592–607.2. Brunner JX, Iotti GA. Adaptive support ventilation (ASV). Minerva Anestesiol. 2002. 68:365–368.3. Campbell RS, Branson RD, Johannigman JA. Adaptive support ventilation. Respir Care Clin N Am. 2001. 7:425–440.4. Laubscher TP, Frutiger A, Fanconi S, Jutzi H, Brunner JX. Automatic selection of tidal volume, respiratory frequency and minute ventilation in intubated ICU patients as start up procedure for closed-loop controlled ventilation. Int J Clin Monit Comput. 1994. 11:19–30.5. Arnal JM, Wysocki M, Nafati C, Donati S, Granier I, Corno G, et al. Automatic selection of breathing pattern using adaptive support ventilation. Intensive Care Med. 2008. 34:75–81.6. Iotti GA, Polito A, Belliato M, Pasero D, Beduneau G, Wysocki M, et al. Adaptive support ventilation versus conventional ventilation for total ventilatory support in acute respiratory failure. Intensive Care Med. 2010. 36:1371–1379.7. Petter AH, Chioléro RL, Cassina T, Chassot PG, Müller XM, Revelly JP. Automatic "respirator/weaning" with adaptive support ventilation: the effect on duration of endotracheal intubation and patient management. Anesth Analg. 2003. 97:1743–1750.8. Burns KE, Lellouche F, Lessard MR. Automating the weaning process with advanced closed-loop systems. Intensive Care Med. 2008. 34:1757–1765.9. Linton DM, Potgieter PD, Davis S, Fourie AT, Brunner JX, Laubscher TP. Automatic weaning from mechanical ventilation using an adaptive lung ventilation controller. Chest. 1994. 106:1843–1850.10. Sulemanji D, Marchese A, Garbarini P, Wysocki M, Kacmarek RM. Adaptive support ventilation: an appropriate mechanical ventilation strategy for acute respiratory distress syndrome? Anesthesiology. 2009. 111:863–870.11. The Acute Respiratory Distress Syndrome Network. Ventilation with lower tidal volumes as compared with traditional tidal volumes for acute lung injury and the acute respiratory distress syndrome. N Engl J Med. 2000. 342:1301–1308.12. Dongelmans DA, Schultz MJ. Adaptive support ventilation: an inappropriate mechanical ventilation strategy for acute respiratory distress syndrome? Anesthesiology. 2010. 112:1295. author reply 1295-6.13. Choi IS, Koh YS, Leem CM, Choi JE, Hong SB. A comparison of adaptive support ventilation (ASV) and conventional volume-controlled ventilation on respiratory mechanics in acute lung injury/ARDS. Korean J Crit Care Med. 2009. 24:59–63.14. Bernard GR, Artigas A, Brigham KL, Carlet J, Falke K, Hudson L, et al. Consensus Committee. Report of the American-European Consensus conference on acute respiratory distress syndrome: definitions, mechanisms, relevant outcomes, and clinical trial coordination. J Crit Care. 1994. 9:72–81.15. Knaus WA, Draper EA, Wagner DP, Zimmerman JE. APACHE II: a severity of disease classification system. Crit Care Med. 1985. 13:818–829.16. Ferreira FL, Bota DP, Bross A, Mélot C, Vincent JL. Serial evaluation of the SOFA score to predict outcome in critically ill patients. JAMA. 2001. 286:1754–1758.17. Devine BJ. Gentamicin therapy. Drug Intell Clin Pharm. 1974. 8:650–655.18. Slutsky AS. Consensus conference on mechanical ventilation--January 28-30, 1993 at Northbrook, Illinois, USA. Part 2. Intensive Care Med. 1994. 20:150–162.19. Ramsay MA, Savege TM, Simpson BR, Goodwin R. Controlled sedation with alphaxalone-alphadolone. Br Med J. 1974. 2:656–659.20. Iotti GA, Braschi A, Brunner JX, Smits T, Olivei M, Palo A, et al. Respiratory mechanics by least squares fitting in mechanically ventilated patients: applications during paralysis and during pressure support ventilation. Intensive Care Med. 1995. 21:406–413.21. Kallet RH, Jasmer RM, Pittet JF, Tang JF, Campbell AR, Dicker R, et al. Clinical implementation of the ARDS network protocol is associated with reduced hospital mortality compared with historical controls. Crit Care Med. 2005. 33:925–929.22. Hager DN, Krishnan JA, Hayden DL, Brower RG. ARDS Clinical Trials Network. Tidal volume reduction in patients with acute lung injury when plateau pressures are not high. Am J Respir Crit Care Med. 2005. 172:1241–1245.23. Gattinoni L, Vagginelli F, Chiumello D, Taccone P, Carlesso E. Physiologic rationale for ventilator setting in acute lung injury/acute respiratory distress syndrome patients. Crit Care Med. 2003. 31:S300–S304.24. Marini JJ, Gattinoni L. Ventilatory management of acute respiratory distress syndrome: a consensus of two. Crit Care Med. 2004. 32:250–255.25. Gattinoni L, Pesenti A. The concept of "baby lung". Intensive Care Med. 2005. 31:776–784.26. Kacmarek RM. Lung protection: the cost in some is increased work of breathing. Is it too high? Respir Care. 2005. 50:1614–1616.27. Deans KJ, Minneci PC, Cui X, Banks SM, Natanson C, Eichacker PQ. Mechanical ventilation in ARDS: one size does not fit all. Crit Care Med. 2005. 33:1141–1143.28. Jardin F. Tidal volume reduction in patients with acute lung injury when plateau pressures are not high. Am J Respir Crit Care Med. 2006. 173:685–686. author reply 687.29. Amato MB, Barbas CS, Medeiros DM, Schettino Gde P, Lorenzi Filho G, Kairalla RA, et al. Beneficial effects of the "open lung approach" with low distending pressures in acute respiratory distress syndrome. A prospective randomized study on mechanical ventilation. Am J Respir Crit Care Med. 1995. 152:1835–1846.30. Weiler N, Eberle B, Heinrichs W. Adaptive lung ventilation (ALV) during anesthesia for pulmonary surgery: automatic response to transitions to and from one-lung ventilation. J Clin Monit Comput. 1998. 14:245–252.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Ventilator-Induced Lung Injury
- Brain and Lung: Lung Injury in Patients with Brain Injury
- The Relationship between Early Changes in Respiratory Parameters and the Prognosis in Children with Acute Lung Injury
- Non-invasive ventilation for surgical patients with acute respiratory failure
- A Comparison of Adaptive Support Ventilation (ASV) and Conventional Volume-Controlled Ventilation on Respiratory Mechanics in Acute Lung Injury/ARDS