Tuberc Respir Dis.
2009 Sep;67(3):205-211.
Semi-quantitative Procalcitonin Assay in Critically ill Patients with Respiratory infections
- Affiliations
-
- 1Department of Internal Medicine, Hallym University College of Medicine, Seoul, Korea. kimch2002@hallym.or.kr
Abstract
- BACKGROUND
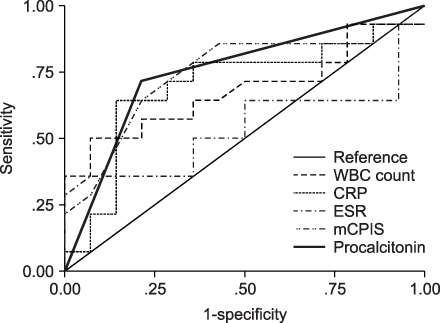
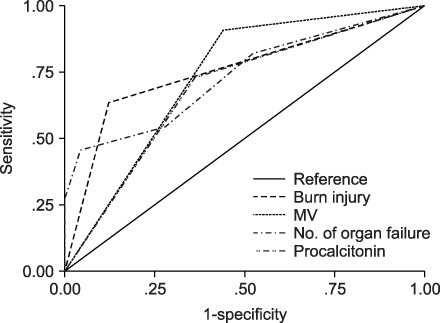
Serum procalcitonin level has been considered prognostic during sepsis and septic shock. We investigated the significance of procalcitonin in critically ill patients with respiratory infections. METHODS: The patients who had radiographically diagnosed diffuse lung infiltrations were enrolled on a prospective basis. Bronchoalveolar lavage (BAL) fluid for the purpose of quantitative cultures (> or =10(4) cfu/mL) was obtained from all patients. Serum procalcitonin levels determined by PCT-Q kit were measured on BAL day and classified as follows; <0.5 ng/mL, 0.5~2.0 ng/mL, 2.0~10.0 ng/mL and >10.0 ng/mL. We analyzed the patient's characteristics according to outcome; favorable or unfavorable, defined as death. RESULTS: Patients from the following categories were included: medical 17 (47.2%), surgical 9 (25%), and burned 10 (27.8%). APACHE II scores on admission to intensive care unit were 11.5+/-6.89 and 11 (30.6%) had unfavorable outcomes. A procalcitonin level > or =0.5 ng/mL was in 17 (47.2%) of all. On univariate analysis, the frequencies of burn injury, mechanical ventilation, multiple organ failure, and a procalcitonin level > or =0.5 ng/mL were more often increased in patients with unfavorable outcomes than in those with favorable outcomes (p<.05). Also, a higher procalcitonin range and ventilator-associated pneumonia (VAP) were more closely associated with an unfavorable outcome (p<.05). However in multivariate analysis, a strong predictor of unfavorable outcome was burn injury (p<.05). A procalcitonin level > or =0.5 ng/mL was more sensitive in predicting VAP than unfavorable outcome. CONCLUSION: A higher procalcitonin level seems to be associated with VAP, but further study is required to know that procalcitonin would be a prognostic marker in critically ill patients with respiratory infections.
Keyword
MeSH Terms
Figure
Reference
-
1. Vincent JL. Nosocomial infections in adult intensive-care units. Lancet. 2003. 361:2068–2077.2. Assicot M, Gendrel D, Carsin H, Raymond J, Guilbaud J, Bohuon C. High serum procalcitonin concentrations in patients with sepsis and infection. Lancet. 1993. 341:515–518.3. Aouifi A, Piriou V, Bastien O, Blanc P, Bouvier H, Evans R, et al. Usefulness of procalcitonin for diagnosis of infection in cardiac surgical patients. Crit Care Med. 2000. 28:3171–3176.4. Dandona P, Nix D, Wilson MF, Aljada A, Love J, Assicot M, et al. Procalcitonin increase after endotoxin injection in normal subjects. J Clin Endocrinol Metab. 1994. 79:1605–1608.5. Wanner GA, Keel M, Steckholzer U, Beier W, Stocker R, Ertel W. Relationship between procalcitonin plasma levels and severity of injury, sepsis, organ failure, and mortality in injured patients. Crit Care Med. 2000. 28:950–957.6. Nylén ES, Snider RH Jr, Thompson KA, Rohatgi P, Becker KL. Pneumonitis-associated hyperprocalcitoninemia. Am J Med Sci. 1996. 312:12–18.7. Oberhoffer M, Stonans I, Russwurm S, Stonane E, Vogelsang H, Junker U, et al. Procalcitonin expression in human peripheral blood mononuclear cells and its modulation by lipopolysaccharides and sepsis-related cytokines in vitro. J Lab Clin Med. 1999. 134:49–55.8. Duflo F, Debon R, Monneret G, Bienvenu J, Chassard D, Allaouchiche B. Alveolar and serum procalcitonin: diagnostic and prognostic value in ventilator-associated pneumonia. Anesthesiology. 2002. 96:74–79.9. Chastre J, Fagon JY, Bornet-Lecso M, Calvat S, Dombret MC, al Khani R, et al. Evaluation of bronchoscopic techniques for the diagnosis of nosocomial pneumonia. Am J Respir Crit Care Med. 1995. 152:231–240.10. Clinical Laboratory Standards Institute. CLSI document M100-S18. Performance standards for antimicrobial susceptibility testing; eighteenth informational supplement. 2008. Wayne: Clinical and Laboratory Standards Institute.11. Niederman MS, Mandell LA, Anzueto A, Bass JB, Broughton WA, Campbell GD, et al. Guidelines for the management of adults with community-acquired pneumonia: diagnosis, assessment of severity, antimicrobial therapy, and prevention. Am J Respir Crit Care Med. 2001. 163:1730–1754.12. American Thoracic Society. Guidelines for the management of adults with hospital-acquired, ventilator-associated, and healthcare-associated pneumonia. Am J Respir Crit Care Med. 2005. 171:388–416.13. Luna CM, Blanzaco D, Niederman MS, Matarucco W, Baredes NC, Desmery P, et al. Resolution of ventilator-associated pneumonia: prospective evaluation of the clinical pulmonary infection score as an early clinical predictor of outcome. Crit Care Med. 2003. 31:676–682.14. Chastre J, Fagon JY. Ventilator-associated pneumonia. Am J Respir Crit Care Med. 2002. 165:867–903.15. Dennesen PJ, van der Ven AJ, Kessels AG, Ramsay G, Bonten MJ. Resolution of infectious parameters after antimicrobial therapy in patients with ventilator-associated pneumonia. Am J Respir Crit Care Med. 2001. 163:1371–1375.16. Ioanas M, Ferrer M, Cavalcanti M, Ferrer R, Ewig S, Filella X, et al. Causes and predictors of nonresponse to treatment of intensive care unit-acquired pneumonia. Crit Care Med. 2004. 32:938–945.17. Luyt CE, Guérin V, Combes A, Trouillet JL, Ayed SB, Bernard M, et al. Procalcitonin kinetics as a prognostic marker of ventilator-associated pneumonia. Am J Respir Crit Care Med. 2005. 171:48–53.18. Meisner M, Tschaikowsky K, Palmaers T, Schmidt J. Comparison of procalcitonin (PCT) and C-reactive protein (CRP) plasma concentrations at different SOFA scores during the course of sepsis and MODS. Crit Care. 1999. 3:45–50.19. Shirani KZ, Pruitt BA Jr, Mason AD Jr. The influence of inhalation injury and pneumonia on burn mortality. Ann Surg. 1987. 205:82–87.20. von Heimburg D, Stieghorst W, Khorram-Sefat R, Pallua N. Procalcitonin: a sepsis parameter in severe burn injuries. Burns. 1998. 24:745–750.21. Mandi Y, Farkas G, Takacs T, Boda K, Lonovics J. Diagnostic relevance of procalcitonin, IL-6, and sICAM-1 in the prediction of infected necrosis in acute pancreatitis. Int J Pancreatol. 2000. 28:41–49.22. Nylen ES, O'Neill W, Jordan MH, Snider RH, Moore CF, Lewis M, et al. Serum procalcitonin as an index of inhalation injury in burns. Horm Metab Res. 1992. 24:439–443.23. Jensen JU, Heslet L, Jensen TH, Espersen K, Steffensen P, Tvede M. Procalcitonin increase in early identification of critically ill patients at high risk of mortality. Crit Care Med. 2006. 34:2596–2602.24. Gibot S, Cravoisy A, Levy B, Bene MC, Faure G, Bollaert PE. Soluble triggering receptor expressed on myeloid cells and the diagnosis of pneumonia. N Engl J Med. 2004. 350:451–458.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Usefulness of Semi-quantitative Procalcitonin Assay in Critically Ill Patients with Bacterial Pneumonia
- Prognostic Value of Serum Procalcitonin level for the Diagnosis of Bacterial Infections in Critically-ill Patients
- Procalcitonin to Guide Antibiotic Therapy for Critically Ill Patients in Korea
- Experience of Treating Critically Ill COVID-19 Patients in Daegu, South Korea
- Risk factors associated with development of coinfection in critically Ill patients with COVID-19