Tuberc Respir Dis.
2009 Jul;67(1):21-26.
Prediction of Intubation after Bronchoscopy with Non-invasive Positive Pressure Ventilation Support in Patients with Acute Hypoxemic Respiratory Failure
- Affiliations
-
- 1Division of Pulmonary and Critical Care Medicine, Department of Medicine, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea. kjeon@skku.edu
Abstract
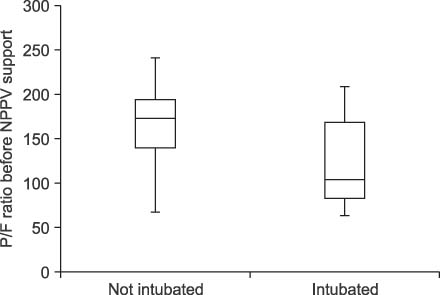
- BACKGROUND
Non-invasive positive pressure ventilation (NPPV) ensures adequate gas exchange during bronchoscopy in spontaneously breathing, hypoxemic patients, thus avoiding endotracheal intubation. However, in some patients, endotracheal intubation is eventually required after bronchoscopy. This study investigated the incidence of intubation and predictors of a need for emergency intubation prior to NPPV bronchoscopy initiation. METHODS: On a retrospective basis, we reviewed the medical records of 36 patients (median age, 55 years; interquartile range [IQR], 43~65 years) with acute hypoxemic respiratory failure who required NPPV during bronchoscopy between January 2005 and October 2007. RESULTS: All patients were hypoxemic (median PaO2/FiO2 ratio 155; IQR 90~190), but tolerated bronchoscopy with NPPV support. SOFA score and SAPS II score immediately before NPPV initiation were 4 (3~7) and 36 (30~42), respectively. Seventeen (47%) patients needed endotracheal intubation at a median time of 22 (2~50) hours after bronchoscopy. Patients who needed intubation after bronchoscopy had a higher in-hospital mortality (11 [65%] vs. 4 [21%], p=0.017). Upon multiple logistic regression analysis, the need for intubation after bronchoscopy was independently associated with a PaO2/FiO2 ratio (OR, 0.961; 95% CI, 0.924~0.999; p=0.047) immediately before NPPV initiation for bronchoscopy. CONCLUSION: The severity of the hypoxemia immediately prior to NPPV initiation for bronchoscopy was associated with the need for intubation after bronchoscopy in patients with hypoxemic respiratory failure.
MeSH Terms
Figure
Reference
-
1. Pue CA, Pacht ER. Complications of fiberoptic bronchoscopy at a university hospital. Chest. 1995. 107:430–432.2. Goldstein RA, Rohatgi PK, Bergofsky EH, Block ER, Daniele RP, Dantzker DR, et al. Clinical role of bronchoalveolar lavage in adults with pulmonary disease. Am Rev Respir Dis. 1990. 142:481–486.3. Albertini R, Harrel JH, Moser KM. Hypoxemia during fiberoptic bronchoscopy. Chest. 1974. 65:117–118.4. Trouillet JL, Guiguet M, Gibert C, Fagon JY, Dreyfuss D, Blanchet F, et al. Fiberoptic bronchoscopy in ventilated patients. Evaluation of cardiopulmonary risk under midazolam sedation. Chest. 1990. 97:927–933.5. Antonelli M, Conti G, Riccioni L, Meduri GU. Noninvasive positive-pressure ventilation via face mask during bronchoscopy with BAL in high-risk hypoxemic patients. Chest. 1996. 110:724–728.6. Maitre B, Jaber S, Maggiore SM, Bergot E, Richard JC, Bakthiari H, et al. Continuous positive airway pressure during fiberoptic bronchoscopy in hypoxemic patients: a randomized double-blind study using a new device. Am J Respir Crit Care Med. 2000. 162:1063–1067.7. Hilbert G, Gruson D, Vargas F, Valentino R, Favier JC, Portel L, et al. Bronchoscopy with bronchoalveolar lavage via the laryngeal mask airway in high-risk hypoxemic immunosuppressed patients. Crit Care Med. 2001. 29:249–255.8. Antonelli M, Conti G, Rocco M, Arcangeli A, Cavaliere F, Proietti R, et al. Noninvasive positive-pressure ventilation vs. conventional oxygen supplementation in hypoxemic patients undergoing diagnostic bronchoscopy. Chest. 2002. 121:1149–1154.9. An CH, Lim SY, Suh GY, Park GY, Park JW, Jeong SH, et al. Continuous positive airway pressure during bronchoalveolar lavage in patients with severe hypoxemia. Tuberc Respir Dis. 2003. 54:71–79.10. Antonelli M, Pennisi MA, Conti G, Bello G, Maggiore SM, Michetti V, et al. Fiberoptic bronchoscopy during noninvasive positive pressure ventilation delivered by helmet. Intensive Care Med. 2003. 29:126–129.11. Lindholm CE, Ollman B, Snyder J, Millen E, Grenvik A. Flexible fiberoptic bronchoscopy in critical care medicine: diagnosis, therapy and complications. Crit Care Med. 1974. 2:250–261.12. Lindholm CE, Ollman B, Snyder JV, Millen EG, Grenvik A. Cardiorespiratory effects of flexible fiberoptic bronchoscopy in critically ill patients. Chest. 1978. 74:362–368.13. Matsushima Y, Jones RL, King EG, Moysa G, Alton JD. Alterations in pulmonary mechanics and gas exchange during routine fiberoptic bronchoscopy. Chest. 1984. 86:184–188.14. Estes RJ, Meduri GU. The pathogenesis of ventilator-associated pneumonia: I. Mechanisms of bacterial transcolonization and airway inoculation. Intensive Care Med. 1995. 21:365–383.15. Stauffer JL, Olson DE, Petty TL. Complications and consequences of endotracheal intubation and tracheotomy: a prospective study of 150 critically ill adult patients. Am J Med. 1981. 70:65–76.16. Brochard L. Noninvasive ventilation for acute respiratory failure. JAMA. 2002. 288:932–935.17. Schettino G, Altobelli N, Kacmarek RM. Noninvasive positive-pressure ventilation in acute respiratory failure outside clinical trials: experience at the Massachusetts General Hospital. Crit Care Med. 2008. 36:441–447.18. Wood KA, Lewis L, Von Harz B, Kollef MH. The use of noninvasive positive pressure ventilation in the emergency department: results of a randomized clinical trial. Chest. 1998. 113:1339–1346.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Treatment of acute respiratory failure: noninvasive mechanical ventilation
- Non-invasive ventilation for surgical patients with acute respiratory failure
- Mechanical Ventilation of the Children
- Treatment of acute respiratory failure: invasive mechanical ventilation
- Does the Mean Arterial Pressure Influence Mortality Rate in Patients with Acute Hypoxemic Respiratory Failure under Mechanical Ventilation?