Tuberc Respir Dis.
2015 Apr;78(2):85-91. 10.4046/trd.2015.78.2.85.
Does the Mean Arterial Pressure Influence Mortality Rate in Patients with Acute Hypoxemic Respiratory Failure under Mechanical Ventilation?
- Affiliations
-
- 1Department of Internal Medicine, Keimyung University School of Medicine, Daegu, Korea. wichoi@dsmc.or.kr
- 2Department of Internal Medicine, Mother Thereza University Hospital, Tirana, Albania.
- KMID: 2320599
- DOI: http://doi.org/10.4046/trd.2015.78.2.85
Abstract
- BACKGROUND
In sepsis patients, target mean arterial pressures (MAPs) greater than 65 mm Hg are recommended. However, there is no such recommendation for patients receiving mechanical ventilation. We aimed to evaluate the influence of MAP over the first 24 hours after intensive care unit (ICU) admission on the mortality rate at 60 days post-admission in patients showing acute hypoxemic respiratory failure under mechanical ventilation.
METHODS
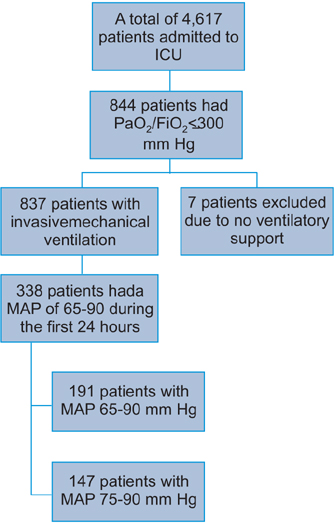
This prospective, multicenter study included 22 ICUs and compared the mortality and clinical outcomes in patients showing acute hypoxemic respiratory failure with high (75-90 mm Hg) and low (65-74.9 mm Hg) MAPs over the first 24 hours of admission to the ICU.
RESULTS
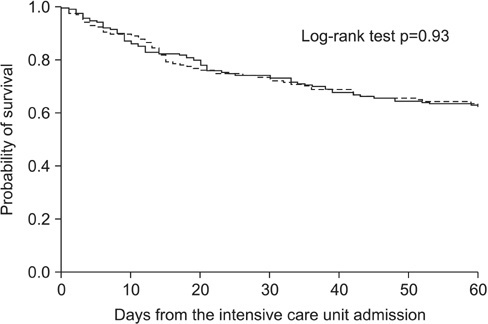
Of the 844 patients with acute hypoxemic respiratory failure, 338 had a sustained MAP of 65-90 mm Hg over the first 24 hours of admission to the ICU. At 60 days, the mortality rates in the low (26.2%) and high (24.5%) MAP groups were not significantly different. The ICU days, hospital days, and 60-day mortality rate did not differ between the groups.
CONCLUSION
In the first 24 hours of ICU admission, MAP range between 65 and 90 mm Hg in patients with acute hypoxemic respiratory failure under mechanical ventilation may not cause significantly differences in 60-day mortality.
MeSH Terms
Figure
Reference
-
1. ARDS Definition Task Force. Ranieri VM, Rubenfeld GD, Thompson BT, Ferguson ND, Caldwell E, et al. Acute respiratory distress syndrome: the Berlin Definition. JAMA. 2012; 307:2526–2533.2. Vincent JL, Akca S, De Mendonca A, Haji-Michael P, Sprung C, Moreno R, et al. The epidemiology of acute respiratory failure in critically ill patients(*). Chest. 2002; 121:1602–1609.3. Vasilyev S, Schaap RN, Mortensen JD. Hospital survival rates of patients with acute respiratory failure in modern respiratory intensive care units: an international, multicenter, prospective survey. Chest. 1995; 107:1083–1088.4. Lewandowski K, Metz J, Deutschmann C, Preiss H, Kuhlen R, Artigas A, et al. Incidence, severity, and mortality of acute respiratory failure in Berlin, Germany. Am J Respir Crit Care Med. 1995; 151:1121–1125.5. Antonelli M, Levy M, Andrews PJ, Chastre J, Hudson LD, Manthous C, et al. Hemodynamic monitoring in shock and implications for management. International Consensus Conference, Paris, France, 27-28 April 2006. Intensive Care Med. 2007; 33:575–590.6. Dunser MW, Ruokonen E, Pettila V, Ulmer H, Torgersen C, Schmittinger CA, et al. Association of arterial blood pressure and vasopressor load with septic shock mortality: a post hoc analysis of a multicenter trial. Crit Care. 2009; 13:R181.7. Sakr Y, Dubois MJ, De Backer D, Creteur J, Vincent JL. Persistent microcirculatory alterations are associated with organ failure and death in patients with septic shock. Crit Care Med. 2004; 32:1825–1831.8. LeDoux D, Astiz ME, Carpati CM, Rackow EC. Effects of perfusion pressure on tissue perfusion in septic shock. Crit Care Med. 2000; 28:2729–2732.9. Bourgoin A, Leone M, Delmas A, Garnier F, Albanese J, Martin C. Increasing mean arterial pressure in patients with septic shock: effects on oxygen variables and renal function. Crit Care Med. 2005; 33:780–786.10. West JB. Invited review: pulmonary capillary stress failure. J Appl Physiol (1985). 2000; 89:2483–2489.11. Dreyfuss D, Saumon G. Ventilator-induced lung injury: lessons from experimental studies. Am J Respir Crit Care Med. 1998; 157:294–323.12. Esteban A, Anzueto A, Frutos F, Alia I, Brochard L, Stewart TE, et al. Characteristics and outcomes in adult patients receiving mechanical ventilation: a 28-day international study. JAMA. 2002; 287:345–355.13. Parker JC, Hernandez LA, Peevy KJ. Mechanisms of ventilator-induced lung injury. Crit Care Med. 1993; 21:131–143.14. Levy MM, Artigas A, Phillips GS, Rhodes A, Beale R, Osborn T, et al. Outcomes of the Surviving Sepsis Campaign in intensive care units in the USA and Europe: a prospective cohort study. Lancet Infect Dis. 2012; 12:919–924.15. Lim SY, Koh SO, Jeon K, Na S, Lim CM, Choi WI, et al. Validation of SAPS3 admission score and its customization for use in Korean intensive care unit patients: a prospective multicentre study. Respirology. 2013; 18:989–995.16. Bernard GR. Quantification of organ dysfunction: seeking standardization. Crit Care Med. 1998; 26:1767–1768.17. National Heart, Lung, and Blood Institute Acute Respiratory Distress Syndrome (ARDS) Clinical Trials Network. Wheeler AP, Bernard GR, Thompson BT, Schoenfeld D, Wiedemann HP, et al. Pulmonary-artery versus central venous catheter to guide treatment of acute lung injury. N Engl J Med. 2006; 354:2213–2224.18. Brower RG, Lanken PN, MacIntyre N, Matthay MA, Morris A, Ancukiewicz M, et al. Higher versus lower positive end-expiratory pressures in patients with the acute respiratory distress syndrome. N Engl J Med. 2004; 351:327–336.19. Dellinger RP, Levy MM, Rhodes A, Annane D, Gerlach H, Opal SM, et al. Surviving sepsis campaign: international guidelines for management of severe sepsis and septic shock: 2012. Crit Care Med. 2013; 41:580–637.20. Asfar P, Meziani F, Hamel JF, Grelon F, Megarbane B, Anguel N, et al. High versus low blood-pressure target in patients with septic shock. N Engl J Med. 2014; 370:1583–1593.21. Meade MO, Cook DJ, Guyatt GH, Slutsky AS, Arabi YM, Cooper DJ, et al. Ventilation strategy using low tidal volumes, recruitment maneuvers, and high positive end-expiratory pressure for acute lung injury and acute respiratory distress syndrome: a randomized controlled trial. JAMA. 2008; 299:637–645.22. Annane D, Vignon P, Renault A, Bollaert PE, Charpentier C, Martin C, et al. Norepinephrine plus dobutamine versus epinephrine alone for management of septic shock: a randomised trial. Lancet. 2007; 370:676–684.23. De Backer D, Biston P, Devriendt J, Madl C, Chochrad D, Aldecoa C, et al. Comparison of dopamine and norepinephrine in the treatment of shock. N Engl J Med. 2010; 362:779–789.24. Myburgh JA, Higgins A, Jovanovska A, Lipman J, Ramakrishnan N, Santamaria J, et al. A comparison of epinephrine and norepinephrine in critically ill patients. Intensive Care Med. 2008; 34:2226–2234.25. Rivers E, Nguyen B, Havstad S, Ressler J, Muzzin A, Knoblich B, et al. Early goal-directed therapy in the treatment of severe sepsis and septic shock. N Engl J Med. 2001; 345:1368–1377.26. Russell JA, Walley KR, Singer J, Gordon AC, Hebert PC, Cooper DJ, et al. Vasopressin versus norepinephrine infusion in patients with septic shock. N Engl J Med. 2008; 358:877–887.27. Martin C, Saux P, Eon B, Aknin P, Gouin F. Septic shock: a goal-directed therapy using volume loading, dobutamine and/or norepinephrine. Acta Anaesthesiol Scand. 1990; 34:413–417.28. Dubin A, Pozo MO, Casabella CA, Palizas F Jr, Murias G, Moseinco MC, et al. Increasing arterial blood pressure with norepinephrine does not improve microcirculatory blood flow: a prospective study. Crit Care. 2009; 13:R92.29. Mercat A, Richard JC, Vielle B, Jaber S, Osman D, Diehl JL, et al. Positive end-expiratory pressure setting in adults with acute lung injury and acute respiratory distress syndrome: a randomized controlled trial. JAMA. 2008; 299:646–655.30. Erickson SE, Martin GS, Davis JL, Matthay MA, Eisner MD. NIH NHLBI ARDS Network. Recent trends in acute lung injury mortality: 1996-2005. Crit Care Med. 2009; 37:1574–1579.31. National Heart, Lung, and Blood Institute Acute Respiratory Distress Syndrome (ARDS) Clinical Trials Network. Matthay MA, Brower RG, Carson S, Douglas IS, Eisner M, et al. Randomized, placebo-controlled clinical trial of an aerosolized beta(2)-agonist for treatment of acute lung injury. Am J Respir Crit Care Med. 2011; 184:561–568.32. Rice TW, Wheeler AP, Thompson BT, deBoisblanc BP, Steingrub J, Rock P, et al. Enteral omega-3 fatty acid, gamma-linolenic acid, and antioxidant supplementation in acute lung injury. JAMA. 2011; 306:1574–1581.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Erratum: Does the Mean Arterial Pressure Influence Mortality Rate in Patients with Acute Hypoxemic Respiratory Failure under Mechanical Ventilation?
- Mechanical Ventilation of the Children
- Treatment of acute respiratory failure: invasive mechanical ventilation
- Current status of treatment of acute respiratory failure in Korea
- Treatment of acute respiratory failure: noninvasive mechanical ventilation