Tuberc Respir Dis.
2008 Oct;65(4):328-333.
Recurrent Desquamative Interstitial Pneumonia with Fibrotic Lung Disease
- Affiliations
-
- 1Department of Internal Medicine, College of Medicine, Hallym University, Seoul, Korea. ekmo@hallym.or.kr
- 2Department of Thoracic Surgery, College of Medicine, Hallym University, Seoul, Korea.
- 3Department of Pathology, College of Medicine, Hallym University, Seoul, Korea.
Abstract
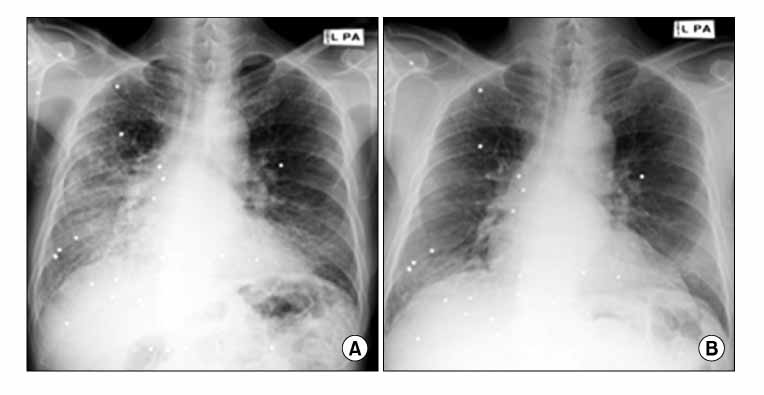
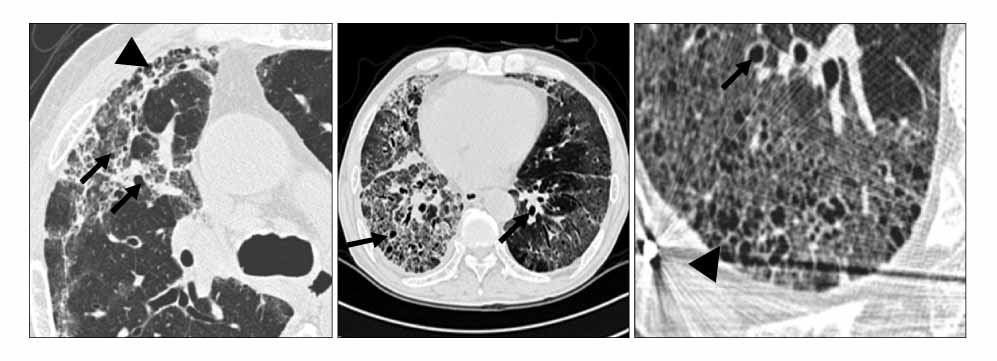
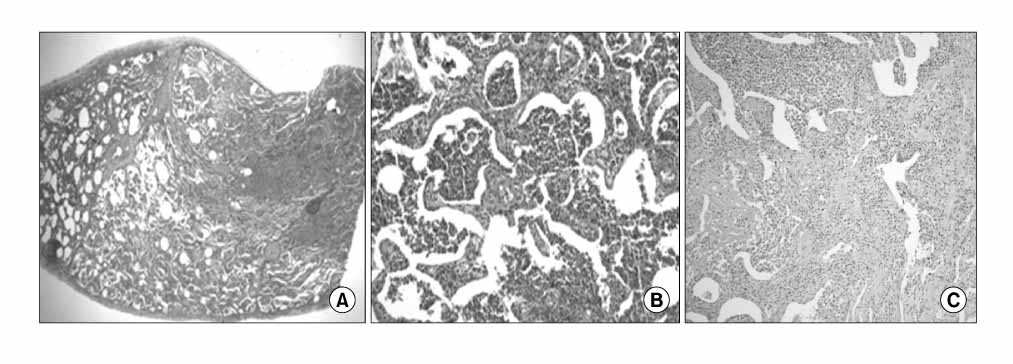
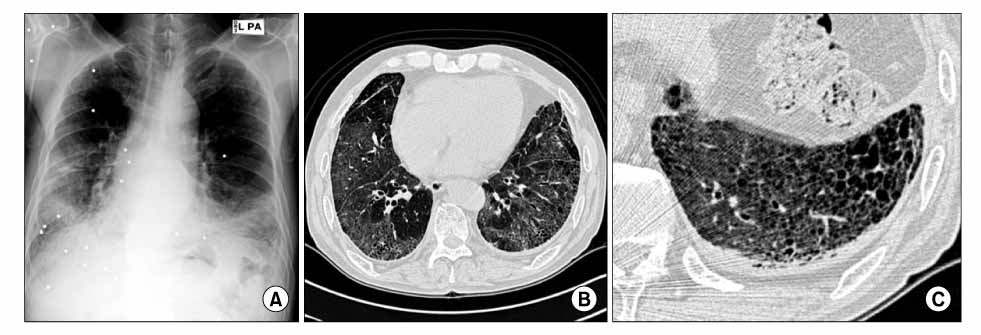
- Desquamative interstitial pneumonia is an uncommon form of interstitial lung diseases and it has a good prognosis compared with other types of idiopathic interstitial pneumonia. A 69-year old man was admitted to our hospital because of a 3-month history of dyspnea. The patient presented with hypoxemia. High-resolution computerized tomography of the patient showed ground glass opacity and traction bronchiectasis with subpleural early honeycombing on the both lung fields. The pathologic findings of the video-assisted thoracoscopy lung biopsy were compatible with desquamative interstitial pneumonia, and irregularly distributed interstitial fibrosis and inflammation were observed at the peripheral parenchyme. Oral predinsolone was started; his symptoms and chest x-ray were improved, and so he stopped taking the prednisolone. Ten months later, the desquamative interstitial pneumonia recurred. We report here on a case of recurrent desquamative interstitial pneumonia with fibrotic lung disease.
MeSH Terms
Figure
Reference
-
1. Liebow AA, Steer A, Billingsley JG. Desquamative interstitial pneumonia. Am J Med. 1965. 39:369–404.2. Carrington CB, Gaensler EA, Coutu RE, Fitzgerald MX, Gupta RG. Usual and desquamative interstitial pneumonia. Chest. 1976. 69:261–263.3. Hartman TE, Primack SL, Kang EY, Swensen SJ, Hansell DM, McGuinness G, et al. Disease progression in usual interstitial pneumonia compared with desquamative interstitial pneumonia: assessment with serial CT. Chest. 1996. 110:378–382.4. Tubbs RR, Benjamin SP, Reich NE, McCormack LJ, Van Ordstrand HS. Desquamative interstitial pneumonitis: cellular phase of fibrosing alveolitis. Chest. 1977. 72:159–165.5. Akira M, Yamamoto S, Hara H, Sakatani M, Ueda E. Serial computed tomographic evaluation in desquamative interstitial pneumonia. Thorax. 1997. 52:333–337.6. Bjoraker JA, Ryu JH, Edwin MK, Myers JL, Tazelaar HD, Schroeder DR, et al. Prognostic significance of histopathologic subsets in idiopathic pulmonary fibrosis. Am J Respir Crit Care Med. 1998. 157:199–203.7. Davies G, Wells AU, du Bois RM. Respiratory bronchiolitis associated with interstitial lung disease and desquamative interstitial pneumonia. Clin Chest Med. 2004. 25:717–726.8. Kawabata Y, Takemura T, Hebisawa A, Ogura T, Yamaguchi T, Kuriyama T, et al. Eosinophilia in bronchoalveolar lavage fluid and architectural destruction are features of desquamative interstitial pneumonia. Histopathology. 2008. 52:194–202.9. Hartman TE, Primack SL, Swensen SJ, Hansell D, McGuinness G, Müller NL. Desquamative interstitial pneumonia: thin-section CT findings in 22 patients. Radiology. 1993. 187:787–790.10. Carrington CB, Gaensler EA, Coutu RE, FitzGerald MX, Gupta RG. Natural history and treated course of usual and desquamative interstitial pneumonia. N Engl J Med. 1978. 298:801–809.11. Lipworth B, Woodcock A, Addis B, Turner-Warwick M. Late relapse of desquamative interstitial pneumonia. Am Rev Respir Dis. 1987. 136:1253–1255.12. Chung JK, Kang HM, Kim KY, Han YC. A case of desquamative interstitial pneumonia. Korean J Med. 1981. 24:244–250.13. Kondoh Y, Taniguchi H, Kawabata Y, Yokoi T, Suzuki K, Takagi K. Acute exacerbation in idiopathic pulmonary fibrosis: analysis of clinical and pathologic findings in three cases. Chest. 1993. 103:1808–1812.14. Collard HR, Moore BB, Flaherty KR, Brown KK, Kaner RJ, King TE Jr, et al. Acute exacerbations of idiopathic pulmonary fibrosis. Am J Respir Crit Care Med. 2007. 176:636–643.15. Kim DS, Park JH, Park BK, Lee JS, Nicholson AG, Colby T. Acute exacerbation of idiopathic pulmonary fibrosis: frequency and clinical features. Eur Respir J. 2006. 27:143–150.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Idiopathic interstitial pneumonias: clinical findings, pathogenesis, pathology and radiologic findings
- Idiopathic Interstitial Pneumonias: Radiologic Findings
- Radiologic Diagnosis of Interstitial Lung Diseases
- Interstitial Lung Diseases in Collagen Vascular Diseases
- Idiopathic Interstitial Pneumonias: Radiologic-Pathologic Correlation