Korean J Urol.
2013 Jun;54(6):399-403.
Prepubertal Testicular Tumors in Korea: A Single Surgeon's Experience of More Than 20 Years
- Affiliations
-
- 1Department of Pediatric Urology, Seoul National University Hospital, Seoul, Korea. urodori9@snu.ac.kr
- 2Department of Urology, Armed Forces Capital Hospital, Seongnam, Korea.
Abstract
- PURPOSE
To present clinical and histological features of prepubertal testicular tumors through the analysis of the long-term experiences of a single surgeon.
MATERIALS AND METHODS
The charts of 48 children treated for testicular tumors from 1986 to 2010 were retrospectively reviewed. All patients underwent radical orchiectomy. The patients' ages, clinical presentations, histopathological findings, kinetics of tumor markers, and outcomes were recorded.
RESULTS
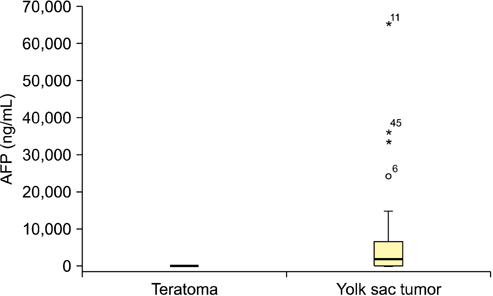
The patients' median age at the initial diagnosis was 19.5 months (range, 3 to 84 months). All patients presented with either a palpable mass (76%) or scrotal size discrepancy (24%). Compared with a palpable mass, scrotal size discrepancy led to delay in diagnosis by 5 months. Regarding histology, yolk sac tumors and teratomas accounted for 53% and 36% of the tumors, respectively. The mean preoperative alpha-fetoprotein (AFP) level was significantly higher in patients with yolk sac tumors than in those with teratomas (4,600 ng/mL vs. 6.3 ng/mL), and only one patient with a teratoma had a preoperative AFP value higher than 20 ng/mL. Following radical orchiectomy, 72%, 8%, and 16% of patients with a yolk sac tumor showed normalization, persistent elevation, and relapse after transient lowering of AFP, respectively. Preoperative AFP was greater in patients with non-normalization than in those with normalization. Five of six patients with non-normalization showed evidence of either vascular invasion or endolymphatic tumor emboli.
CONCLUSIONS
We found a higher number of yolk sac tumors than teratomas in patients with prepubertal testicular tumors. AFP was the most useful marker in the diagnosis and follow-up of childhood yolk sac tumors. Relapsed yolk sac tumors often showed pathological evidence of aggressiveness.
MeSH Terms
Figure
Reference
-
1. Brosman SA. Testicular tumors in prepubertal children. Urology. 1979; 13:581–588.2. Ross JH, Rybicki L, Kay R. Clinical behavior and a contemporary management algorithm for prepubertal testis tumors: a summary of the Prepubertal Testis Tumor Registry. J Urol. 2002; 168(4 Pt 2):1675–1678.3. Oottamasathien S, Thomas JC, Adams MC, DeMarco RT, Brock JW 3rd, Pope JC 4th. Testicular tumours in children: a single-institutional experience. BJU Int. 2007; 99:1123–1126.4. Pohl HG, Shukla AR, Metcalf PD, Cilento BG, Retik AB, Bagli DJ, et al. Prepubertal testis tumors: actual prevalence rate of histological types. J Urol. 2004; 172(6 Pt 1):2370–2372.5. Metcalfe PD, Farivar-Mohseni H, Farhat W, McLorie G, Khoury A, Bagli DJ. Pediatric testicular tumors: contemporary incidence and efficacy of testicular preserving surgery. J Urol. 2003; 170(6 Pt 1):2412–2415.6. Gleason AM. Racial disparities in testicular cancer: impact on health promotion. J Transcult Nurs. 2006; 17:58–64.7. Walsh TJ, Davies BJ, Croughan MS, Carroll PR, Turek PJ. Racial differences among boys with testicular germ cell tumors in the United States. J Urol. 2008; 179:1961–1965.8. Bray F, Ferlay J, Devesa SS, McGlynn KA, Moller H. Interpreting the international trends in testicular seminoma and nonseminoma incidence. Nat Clin Pract Urol. 2006; 3:532–543.9. Lee SD. Korean Society of Pediatric Urology. Epidemiological and clinical behavior of prepubertal testicular tumors in Korea. J Urol. 2004; 172:674–678.10. Chen YS, Kuo JY, Chin TW, Wei CF, Chen KK, Lin AT, et al. Prepubertal testicular germ cell tumors: 25-year experience in Taipei Veterans General Hospital. J Chin Med Assoc. 2008; 71:357–361.11. Kanto S, Saito H, Ito A, Satoh M, Saito S, Arai Y. Clinical features of testicular tumors in children. Int J Urol. 2004; 11:890–893.12. Foster RS, Hermans B, Bihrle R, Donohue JP. Clinical stage I pure yolk sac tumor of the testis in adults has different clinical behavior than juvenile yolk sac tumor. J Urol. 2000; 164:1943–1944.13. Baniel J, Foster RS, Gonin R, Messemer JE, Donohue JP, Einhorn LH. Late relapse of testicular cancer. J Clin Oncol. 1995; 13:1170–1176.14. Kay R. Prepubertal Testicular Tumor Registry. J Urol. 1993; 150(2 Pt 2):671–674.15. Agarwal PK, Palmer JS. Testicular and paratesticular neoplasms in prepubertal males. J Urol. 2006; 176:875–881.16. Treiyer A, Blanc G, Stark E, Haben B, Treiyer E, Steffens J. Prepubertal testicular tumors: frequently overlooked. J Pediatr Urol. 2007; 3:480–483.17. Wu JT, Book L, Sudar K. Serum alpha fetoprotein (AFP) levels in normal infants. Pediatr Res. 1981; 15:50–52.18. Dieckmann KP, Albers P, Classen J, De Wit M, Pichlmeier U, Rick O, et al. Late relapse of testicular germ cell neoplasms: a descriptive analysis of 122 cases. J Urol. 2005; 173:824–829.19. Ayala AG, Ro JY. Testicular tumors: clinically relevant histological findings. Semin Urol Oncol. 1998; 16:72–81.20. Ikeda H, Matsuyama S, Suzuki N, Takahashi A, Kuroiwa M, Nagashima K, et al. Treatment of a stage I testicular yolk sac tumor with vascular invasion. Acta Paediatr Jpn. 1995; 37:537–540.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Overview of Pediatric Testicular Tumors in Korea
- Penile circumference and stretched penile length in prepubertal children: A retrospective, single-center pilot study
- A Case of Bilateral Primary Testicular Tumors
- Ultrasonographic Findings of Torsed Testicular Appendages in Prepubertal Children
- The Pathological Anatomy of Intermittent Testicular Torsion