Korean J Urol.
2010 Jun;51(6):398-402.
Pathologic Results of Radical Prostatectomies in Patients with Simultaneous Atypical Small Acinar Proliferation and Prostate Cancer
- Affiliations
-
- 1Department of Urology, Seoul Veterans Hospital, Seoul, Korea. urodoct@hotmail.com
- 2Department of Pathology, Seoul Veterans Hospital, Seoul, Korea.
Abstract
- PURPOSE
The incidence of adenocarcinoma on a subsequent biopsy following a diagnosis of atypical small acinar proliferation (ASAP) ranges from 34% to 60%. We reexamined radical prostatectomy (RP) specimens of patients diagnosed as having synchronous ASAP with prostate cancer (PCa) to evaluate pathological entities and the clinical significance of ASAP.
MATERIALS AND METHODS
From January 2007 to December 2008, a total of 118 patients who had been diagnosed with adenocarcinoma on prostate needle biopsy underwent RP. Forty-six of the 118 patients (39%) were diagnosed as having synchronous ASAP with PCa on the prostate needle biopsy. Using whole-mount sections and prostate mapping, we evaluated the RP specimens that were close sections to the ASAP on prostate needle biopsy. All tissues were examined by immunohistochemistry with high molecular weight cytokeratin (34betaE12), p63, and AMACR/P504S added to initial H&E stains by one pathologist.
RESULTS
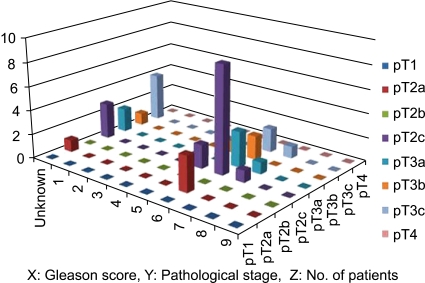
Thirty-six of the 46 patients (78%) were diagnosed as having adenocarcinoma at sites of ASAP on the initial prostate needle biopsies. The Gleason score was 5 to 6 in 22 patients (61%), 7 in 3 (8%), and unknown due to multifocal and microfocal lesions in 11 (31%). The tumor volume of 14 of the 36 patients (39%) was 0.5 cc or less and was unknown due to multifocal and microfocal lesions in 8 (22%).
CONCLUSIONS
Most ASAP on initial prostate needle biopsy was a true pathological entity, in other words, prostatic adenocarcinoma. Aggressive approaches including more extended repeat biopsy with additional biopsy of the site of the ASAP are needed to diagnose PCa in patients with ASAP.
MeSH Terms
Figure
Reference
-
1. Bostwick DG, Srigley J, Grignon D, Maksem J, Humphrey P, van der Kwast TH, et al. Atypical adenomatous hyperplasia of the prostate: morphologic criteria for its distinction from well-differentiated carcinoma. Hum Pathol. 1993; 24:819–832. PMID: 8375853.
Article2. Epstein JI, Potter SR. The pathological interpretation and sig nificance of prostate needle biopsy findings: implications and current controversies. J Urol. 2001; 166:402–410. PMID: 11458037.3. Montironi R, Scattoni V, Mazzucchelli R, Lopez-Beltran A, Bostwick DG, Montorsi F. Atypical foci suspicious but not diagnostic of malignancy in prostate needle biopsies (also referred to as "atypical small acinar proliferation suspicious for but not diagnostic of malignancy"). Eur Urol. 2006; 50:666–674. PMID: 16930809.4. Oh JW, Kim YB, Yang SO, Lee JK, Kim YJ, Jung TY, et al. Prostate cancer detection rate of rebiopsy in patients with an initial diagnosis of atypical small acinar proliferation of the prostate. Korean J Urol. 2009; 50:237–240.
Article5. Ramey JR, Halpern EJ, Gomella LG. Wein AJ, Kavoussi LR, Novick AC, Partin AW, Peters CA, editors. Further commentary: ultrasonography and biopsy of the prostate. Campbell-Walsh urology. 2007. 9th ed. Philadelphia: Saunders;p. 2883–2895.6. Yun JH, Cho HD, Kim DS, Lee CH. The usefulness of P504S/34βE12 immunostaining for the detection of prostate cancer. Korean J Urol. 2007; 48:677–683.
Article7. Jiang Z, Li C, Fischer A, Dresser K, Woda BA. Using an AMACR (P504S)/34betaE12/p63 cocktail for the detection of small focal prostate carcinoma in needle biopsy specimens. Am J Clin Pathol. 2005; 123:231–236. PMID: 15842047.8. Zhou M, Aydin H, Kanane H, Epstein JI. How often does alpha-methylacyl-CoA-racemase contribute to resolving an atypical diagnosis on prostate needle biopsy beyond that provided by basal cell markers? Am J Surg Pathol. 2004; 28:239–243. PMID: 15043314.
Article9. Iczkowski KA. Current prostate biopsy interpretation: criteria for cancer, atypical small acinar proliferation, high-grade prostatic intraepithelial neoplasia, and use of immunostains. Arch Pathol Lab Med. 2006; 130:835–843. PMID: 16740037.
Article10. Schlesinger C, Bostwick DG, Iczkowski KA. High-grade prostatic intraepithelial neoplasia and atypical small acinar proliferation: predictive value for cancer in current practice. Am J Surg Pathol. 2005; 29:1201–1207. PMID: 16096410.11. Brausi M, Castagnetti G, Dotti A, De Luca G, Olmi R, Cesinaro AM. Immediate radical prostatectomy in patients with atypical small acinar proliferation. Over treatment? J Urol. 2004; 172:906–908. PMID: 15310995.
Article12. Hodge KK, McNeal JE, Terris MK, Stamey TA. Random systematic versus directed ultrasound guided transrectal core biopsies of the prostate. J Urol. 1989; 142:71–74. PMID: 2659827.
Article13. Elabbady AA, Khedr MM. Extended 12-core prostate biopsy increases both the detection of prostate cancer and the accuracy of Gleason score. Eur Urol. 2006; 49:49–53. PMID: 16314035.
Article14. Bostwick DG, Montironi R. Evaluating radical prostatectomy specimens: therapeutic and prognostic importance. Virchows Arch. 1997; 430:1–16. PMID: 9037309.
Article15. Park SJ, Miyake H, Hara I, Eto H. Predictors of prostate cancer on repeat transrectal ultrasound-guided systematic prostate biopsy. Int J Urol. 2003; 10:68–71. PMID: 12588600.
Article16. Samaratunga H, Gardiner RA, Yaxley J, Brown I. Atypical prostatic glandular proliferations on needle biopsy: diagnostic implications, use of immunohistochemistry, and clinical significance. Anal Quant Cytol Histol. 2006; 28:104–110. PMID: 16637513.17. Mancuso PA, Chabert C, Chin P, Kovac P, Skyring T, Watt WH, et al. Prostate cancer detection in men with an initial diagnosis of atypical small acinar proliferation. BJU Int. 2007; 99:49–52. PMID: 17227491.
Article18. Fadare O, Wang S, Mariappan MR. Practice patterns of clinicians following isolated diagnoses of atypical small acinar proliferation on prostate biopsy specimens. Arch Pathol Lab Med. 2004; 128:557–560. PMID: 15086303.
Article19. Iczkowski KA, Chen HM, Yang XJ, Beach RA. Prostate cancer diagnosed after initial biopsy with atypical small acinar proliferation suspicious for malignancy is similar to cancer found on initial biopsy. Urology. 2002; 60:851–854. PMID: 12429314.
Article20. Chan TY, Epstein JI. Follow-up of atypical prostate needle biopsies suspicious for cancer. Urology. 1999; 53:351–355. PMID: 9933053.
Article21. Flury SC, Galgano MT, Mills SE, Smolkin ME, Theodorescu D. Atypical small acinar proliferation: biopsy artefact or distinct pathological entity? BJU Int. 2007; 99:780–785. PMID: 17378841.
Article22. Iczkowski KA, Bassler TJ, Schwob VS, Bassler IC, Kunnel BS, Orozco RE, et al. Diagnosis of "suspicious for malignancy" in prostate biopsies: predictive value for cancer. Urology. 1998; 51:749–757. PMID: 9610588.
Article23. Park S, Shinohara K, Grossfeld GD, Carroll PR. Prostate cancer detection in men with prior high grade prostatic intraepithelial neoplasia or atypical prostate biopsy. J Urol. 2001; 165:1409–1414. PMID: 11342887.
Article24. Vis AN, Van Der Kwast TH. Prostatic intraepithelial neoplasia and putative precursor lesions of prostate cancer: a clinical perspective. BJU Int. 2001; 88:147–157. PMID: 11446873.
Article25. Allan RW, Sanderson H, Epstein JI. Correlation of minute (0.5 MM or less) focus of prostate adenocarcinoma on needle biopsy with radical prostatectomy specimen: role of prostate specific antigen density. J Urol. 2003; 170:370–372. PMID: 12853777.
Article26. van Oort IM, Kok DE, Kiemeney LA, Hulsbergen-van de Kaa CA, Witjes JA. A single institution experience with biochemical recurrence after radical prostatectomy for tumors that on pathology are of small volume or "insignificant". Urol Oncol. 2009; 27:509–513. PMID: 18625570.
Article27. Lee SE, Kim DS, Lee WK, Park HZ, Lee CJ, Doo SH, et al. Application of the Epstein criteria for prediction of clinically insignificant prostate cancer in Korean men. BJU Int. 2009; Epub ahead of print.
Article28. Jeldres C, Suardi N, Walz J, Hutterer GC, Ahyai S, Lattouf JB, et al. Validation of the contemporary epstein criteria for insignificant prostate cancer in European men. Eur Urol. 2008; 54:1306–1313. PMID: 18083294.
Article29. Matsumoto K, Satoh T, Egawa S, Shimura S, Kuwao S, Baba S. Efficacy and morbidity of transrectal ultrasound-guided 12-core biopsy for detection of prostate cancer in Japanese men. Int J Urol. 2005; 12:353–360. PMID: 15948721.
Article30. Ploussard G, Plennevaux G, Allory Y, Salomon L, Azoulay S, Vordos D, et al. High-grade prostatic intraepithelial neoplasia and atypical small acinar proliferation on initial 21-core extended biopsy scheme: incidence and implications for patient care and surveillance. World J Urol. 2009; 27:587–592. PMID: 19373471.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Prostate Cancer Detection Rate of Rebiopsy in Patients with an Initial Diagnosis of Atypical Small Acinar Proliferation of the Prostate
- Significance of Atypical Small Acinar Proliferation and High-Grade Prostatic Intraepithelial Neoplasia in Prostate Biopsy
- The importance of histomorphological features and ERG expression in the diagnosis of malignancy in cases with atypical small acinar proliferation
- Predictive Factors of Prostate Cancer at Repeat Biopsy in Patients with an Initial Diagnosis of Atypical Small Acinar Proliferation of the Prostate
- Clinicopathological Significance of the Lymphovascular Invasion Detected in Specimens from Radical Retropubic Prostatectomies