J Pathol Transl Med.
2024 May;58(3):134-140. 10.4132/jptm.2024.03.18.
The importance of histomorphological features and ERG expression in the diagnosis of malignancy in cases with atypical small acinar proliferation
- Affiliations
-
- 1Department of Pathology, Faculty of Medicine, Karadeniz Technical University, Trabzon, Türkiye
- 2Department of Pathology, Kanuni Training and Research Hospital, Health Sciences University, Trabzon, Türkiye
- KMID: 2555539
- DOI: http://doi.org/10.4132/jptm.2024.03.18
Abstract
- Background
Atypical small acinar proliferation (ASAP) cases typically require rebiopsy, which are invasive and associated with increased risk of complications. Our aim in this study was to determine the importance of laboratory and histological findings and E-26 transformation-specific-related gene (ERG) expression in the diagnosis of malignancy.
Methods
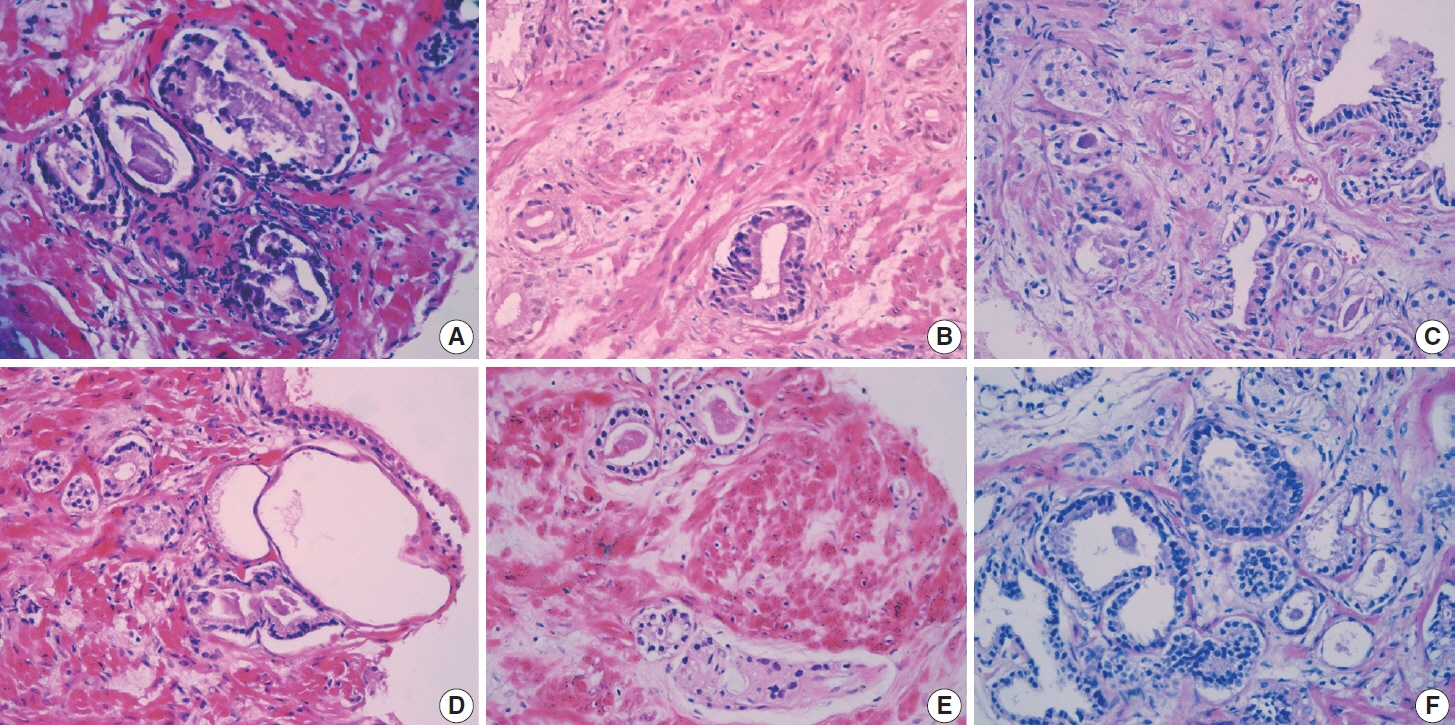
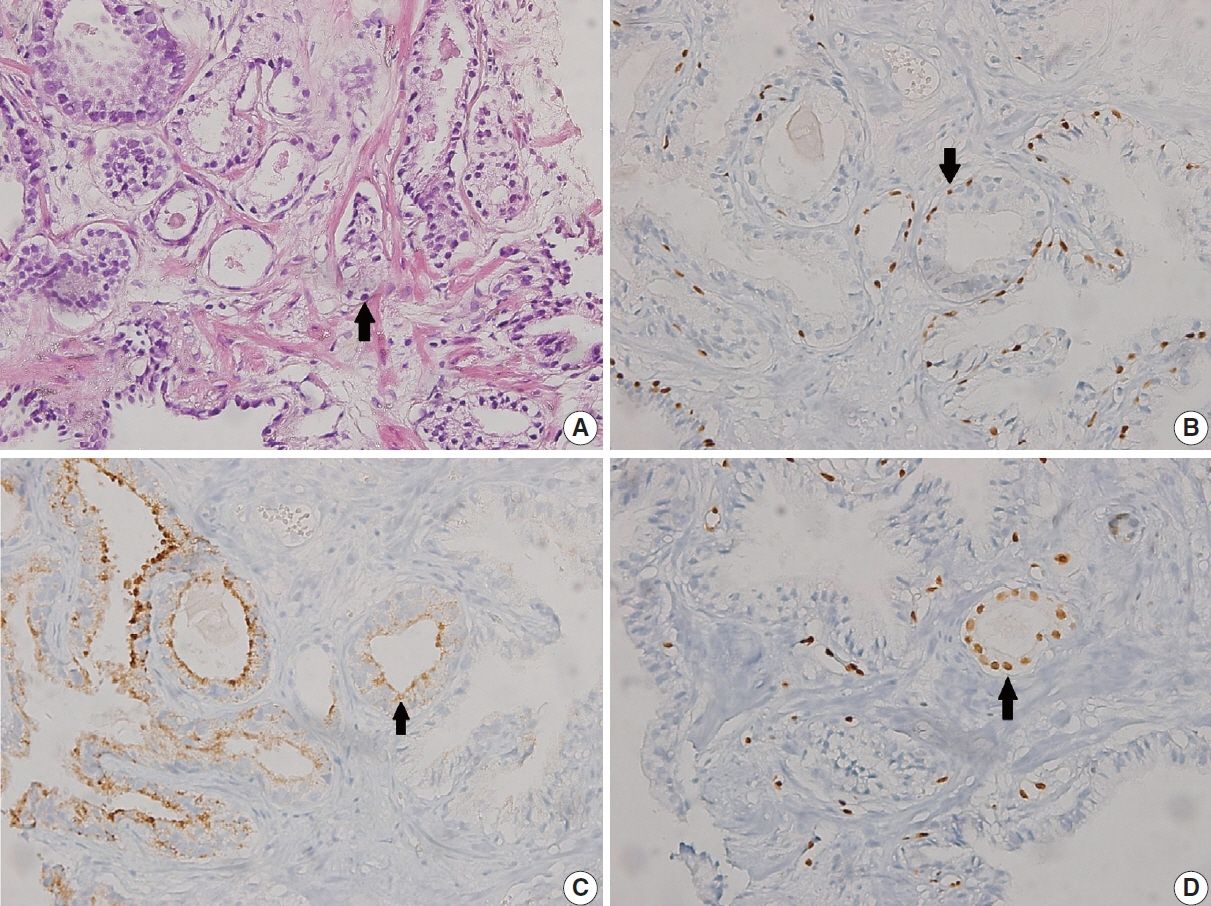
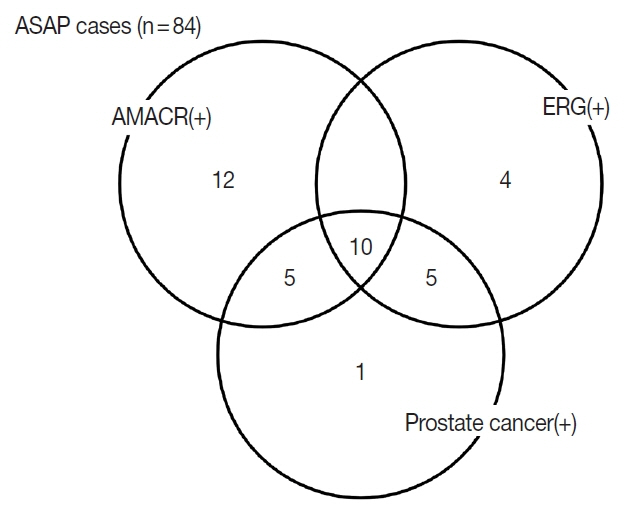
Between March 2016 and March 2022, 84 patients who were diagnosed with ASAP on biopsy or rebiopsy were included in the study. Clinical-laboratory features of age, serum prostate-specific antigen level, and histopathological features were compared and included multifocality, number of suspicious acini, nuclear enlargement, nucleolar prominence, hyperchromasia, cytoplasmic amphophilia, luminal amorphous acellular secretion, crystalloid presence, infiltrative appearance, inflammation, atrophy, α-methyl acyl-CoA racemase, p63, and/or high molecular weight cytokeratin were analyzed. In addition, ERG expression was evaluated immunohistochemically.
Results
Statistically significant correlation was found between nucleolar prominence, nuclear hyperchromasia, crystalloid presence, infiltrative pattern, and prostate cancer (p < .001). In 19 of 84 cases (22.6%) ERG was positive in the nucleus. Prostate cancer was diagnosed at rebiopsy in 15 of the 19 ERG-positive cases (78.9%). A statistically significant correlation was found between ERG positivity and prostate cancer (p= .002).
Conclusions
Our findings suggest that evaluation of these markers during initial transrectal ultrasound biopsies may decrease and prevent unnecessary prostate rebiopsy.
Keyword
Figure
Reference
-
References
1. Yazici S, Kiziloz H, Bozaci AC, Baydar DE, Del Biondo D, Ozen H. Predictors of prostate cancer in ultrasound-guided transperineal saturation biopsy in Turkish men with multiple prior negative biopsies. Urologia. 2016; 83:71–6.
Article2. Mosquera JM, Mehra R, Regan MM, et al. Prevalence of TMPRSS2-ERG fusion prostate cancer among men undergoing prostate biopsy in the United States. Clin Cancer Res. 2009; 15:4706–11.3. Borboroglu PG, Comer SW, Riffenburgh RH, Amling CL. Extensive repeat transrectal ultrasound guided prostate biopsy in patients with previous benign sextant biopsies. J Urol. 2000; 163:158–62.
Article4. Sanguedolce F, Cormio A, Musci G, et al. Typing the atypical: diagnostic issues and predictive markers in suspicious prostate lesions. Crit Rev Clin Lab Sci. 2017; 54:309–25.
Article5. Kitagawa Y, Mizokami A, Namiki M. Trends of clinical symptoms and prognosis of middle-aged prostate cancer patients after instigation of prostate specific antigen-based population screening. Prostate Int. 2013; 1:65–8.
Article6. Chaux A, Albadine R, Toubaji A, et al. Immunohistochemistry for ERG expression as a surrogate for TMPRSS2-ERG fusion detection in prostatic adenocarcinomas. Am J Surg Pathol. 2011; 35:1014–20.
Article7. Mosquera JM, Perner S, Genega EM, et al. Characterization of TMPRSS2-ERG fusion high-grade prostatic intraepithelial neoplasia and potential clinical implications. Clin Cancer Res. 2008; 14:3380–5.8. Dell’Atti L, Galosi AB. The role of the serum testosterone levels as a predictor of prostate cancer in patients with atypical small acinar proliferation at the first prostate biopsy. Asian J Androl. 2018; 20:15–8.
Article9. Ryu JH, Kim YB, Lee JK, Kim YJ, Jung TY. Predictive factors of prostate cancer at repeat biopsy in patients with an initial diagnosis of atypical small acinar proliferation of the prostate. Korean J Urol. 2010; 51:752–6.
Article10. Kato T, Komiya A, Morii A, Iida H, Ito T, Fuse H. Analysis of repeated 24-core saturation prostate biopsy: inverse association between asymptomatic histological inflammation and prostate cancer detection. Oncol Lett. 2016; 12:1132–8.
Article11. Varma M, Lee MW, Tamboli P, et al. Morphologic criteria for the diagnosis of prostatic adenocarcinoma in needle biopsy specimens: a study of 250 consecutive cases in a routine surgical pathology practice. Arch Pathol Lab Med. 2002; 126:554–61.12. Bostwick DG, Meiers I. Atypical small acinar proliferation in the prostate: clinical significance in 2006. Arch Pathol Lab Med. 2006; 130:952–7.
Article13. Montironi R, Scattoni V, Mazzucchelli R, Lopez-Beltran A, Bostwick DG, Montorsi F. Atypical foci suspicious but not diagnostic of malignancy in prostate needle biopsies (also referred to as “atypical small acinar proliferation suspicious for but not diagnostic of malignancy”). Eur Urol. 2006; 50:666–74.14. Magi-Galluzzi C. Prostate cancer: diagnostic criteria and role of immunohistochemistry. Mod Pathol. 2018; 31(S1):S12–21.
Article15. Liu H, Shi J, Wilkerson M, Yang XJ, Lin F. Immunohistochemical evaluation of ERG expression in various benign and malignant tissues. Ann Clin Lab Sci. 2013; 43:3–9.16. Shah RB, Tadros Y, Brummell B, Zhou M. The diagnostic use of ERG in resolving an “atypical glands suspicious for cancer” diagnosis in prostate biopsies beyond that provided by basal cell and alpha-methylacyl-CoA-racemase markers. Hum Pathol. 2013; 44:786–94.17. Mehra R, Han B, Tomlins SA, et al. Heterogeneity of TMPRSS2 gene rearrangements in multifocal prostate adenocarcinoma: molecular evidence for an independent group of diseases. Cancer Res. 2007; 67:7991–5.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Prostate Cancer Detection Rate of Rebiopsy in Patients with an Initial Diagnosis of Atypical Small Acinar Proliferation of the Prostate
- Tuberculosis of the Lower Lumbar Spine with an Atypical Radiological Presentation: A Case Mimicking a Malignancy
- Significance of Atypical Small Acinar Proliferation and High-Grade Prostatic Intraepithelial Neoplasia in Prostate Biopsy
- ERG Immunohistochemistry and Clinicopathologic Characteristics in Korean Prostate Adenocarcinoma Patients
- Evaluation of cytopathologic diagnosis of lung carcinoma