Lab Anim Res.
2012 Mar;28(1):55-60. 10.5625/lar.2012.28.1.55.
Anti-Helicobacter pylori effects of IgY from egg york of immunized hens
- Affiliations
-
- 1College of Veterinary Medicine, Chungbuk National University, Cheongju, Korea. solar93@cbu.ac.kr
- 2Department of Clinical Laboratory Medicine, Chungbuk National University Hospital, Cheongju, Korea.
- 3Department of Biomedical Laboratory Science, Daejeon University, Daejeon, Korea.
- KMID: 2312093
- DOI: http://doi.org/10.5625/lar.2012.28.1.55
Abstract
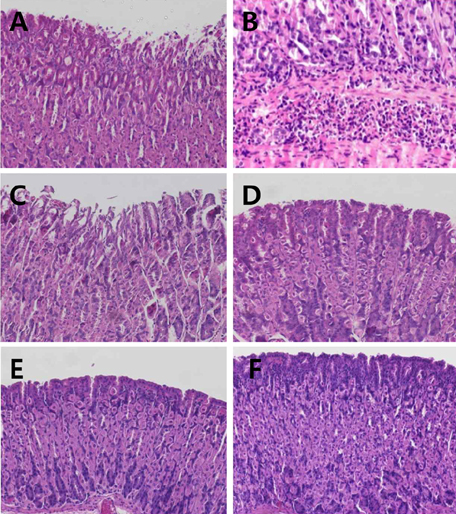
- Effects of egg york containing IgY specific for Helicobacter pylori on the bacterial growth and intragastric infection were investigated in comparison with a proton-pump inhibitor pantoprazole. For in vitro anti-bacterial activity test, H. pylori (1x108 CFU/mL) was incubated with a serially diluted IgY for 3 days. As a result, IgY fully inhibited the bacterial growth at 16 mg/mL, which was determined to a minimal inhibitory concentration. In vivo elimination study, male C57BL/6 mice were infected with the bacteria by intragastric inoculation (1x108 CFU/mouse) 3 times at 2-day intervals, and 2 weeks later, orally treated twice a day with 50, 100, 200 or 500 mg/kg IgY for 18 days. After the final administration, biopsy sample of the gastric mucosa was assayed for the bacterial identification via urease, oxidase, catalase, nitrate reduction and H2S tests in addition to microscopic examination for mucosal inflammation. In CLO kit test, 75, 50, 12.5 and 12.5% of the animals revealed positive reaction following treatment with 50, 100, 200 and 500 mg/kg IgY, respectively, resulting in a superior efficacy at 200 mg/kg than 30 mg/kg pantoprazole that displayed 75% elimination. The CLO test results were confirmed by bacterial identification. Microscopic examination revealed that H. pylori infection caused severe gastric mucosal inflammation, which were not observed in the CLO-negative mice following treatment with IgY or pantoprazole. Taken together, IgY inhibited the growth of H. pylori, and improved gastritis and villi injuries by eliminating the bacteria from the stomach. The results indicate that IgY could be a good candidate overcoming tolerance of antibiotics for the treatment of H. pylori-mediated gastric ulcers.
Keyword
MeSH Terms
-
2-Pyridinylmethylsulfinylbenzimidazoles
Animals
Anti-Bacterial Agents
Bacteria
Biopsy
Catalase
Gastric Mucosa
Gastritis
Helicobacter pylori
Humans
Immunoglobulins
Inflammation
Male
Mice
Ovum
Oxidoreductases
Stomach
Stomach Ulcer
Urease
2-Pyridinylmethylsulfinylbenzimidazoles
Anti-Bacterial Agents
Catalase
Immunoglobulins
Oxidoreductases
Urease
Figure
Reference
-
1. Wallace JL, Granger DN. The cellular and molecular basis of gastric mucosal defense. FASEB J. 1996. 10(7):731–740.2. Neal MJ. Medical Pharmacology at a Glance. 2003. 3rd ed. London: Blackwell Publishing Inc;30–31.3. Isobe H, Okajima K, Harada N, Liu W, Okabe H. Activated protein C reduces stress-induced gastric mucosal injury in rats by inhibiting the endothelial cell injury. J Thromb Haemost. 2004. 2(2):313–320.4. Byun SK, Lee YE, Shin SH, Jang JY, Choi BI, Park DS, Jeon JH, Nahm SS, Hwang SY, Kim YB. The role of corticosteroids in stress-induced gastric ulceration in rats. Lab Anim Res. 2007. 23:127–131.5. Slomiany BL, Piotrowski J, Slomiany A. Induction of tumor necrosis factor-alpha and apoptosis in gastric mucosal injury by indomethacin: effect of omeprazole and ebrotidine. Scand J Gastroenterol. 1997. 32(7):638–642.6. Filaretova L, Tanaka A, Miyazawa T, Kato S, Takeuchi K. Mechanisms by which endogenous glucocorticoid protects against indomethacin-induced gastric injury in rats. Am J Physiol Gastrointest Liver Physiol. 2002. 283(5):G1082–G1089.7. Cao H, Wang MW, Jia JH, Wang QG, Cheng MS. Comparison of the effects of pantoprazole enantimers on gastric mucosal lesions and gastric epithelial cells in rats. J Health Sci. 2004. 50:1–8.8. Rao ChV, Ojha SK, Radhakrishnan K, Govindarajan R, Rastogi S, Mehrotra S, Pushpangadan P. Antiulcer activity of Utleria salicifolia rhizome extract. J Ethnopharmacol. 2004. 91(2-3):243–249.9. Kim YR, Lee MR, Kim YH, Jang BJ, Park SC, Han SH, Kim BH, Ryoo ZY, Kim KS. Effect of Opuntiahumifusa extract on indomethacin-induced gastric ulcer in Sprague Dawley rat. Lab Anim Res. 2005. 21:375–578.10. Raffin RP, Colomé LM, Schapoval EE, Jornada DS, Pohlmann AR, Guterres SS. Gastro-resistant microparticles containing sodium pantoprazole: stability and in vivo anti-ulcer activity. Open Drug Deliv J. 2007. 1:28–35.11. Dias PC, Foglio MA, Possenti A, de Carvalho JE. Antiulcerogenic activity of crude hydroalcoholic extract of Rosmarinus officinalis L. J Ethnopharmacol. 2000. 69(1):57–62.12. Cantarella G, Martinez G, Cutuli VM, Loreto C, D'Alcamo M, Prato A, Amico-Roxas M, Bernardini R, Clementi G. Adrenomedullin modulates COX-2 and HGF expression in reserpine-injuried gastric mucosa in the rat. Eur J Pharmacol. 2005. 518(2-3):221–226.13. Cantarella G, Martinez G, Di Benedetto G, Loreto C, Musumeci G, Prato A, Lempereur L, Matera M, Amico-Roxas M, Bernardini R, Clementi G. Protective effects of amylin on reserpine-induced gastric damage in the rat. Pharmacol Res. 2007. 56(1):27–34.14. Işbil Büyükcoşkun N, Gulec G, Ozluk K. Protective effect of centrally-injected glucagon-like peptide-1 on reserpine-induced gastric mucosal lesions in rat: possible mechanisms. Turk J Gastroenterol. 2006. 17(1):1–6.15. Pope AJ, Toseland CD, Rushant B, Richardson S, McVey M, Hills J. Effect of potent urease inhibitor, fluorofamide, on Helicobacter sp. in vivo and in vitro. Dig Dis Sci. 1998. 43(1):109–119.16. Hahm KB, Kim DH, Lee KM, Lee JS, Surh YJ, Kim YB, Yoo BM, Kim JH, Joo HJ, Cho YK, Nam KT, Cho SW. Effect of long-term administration of rebamipide on Helicobacter pylori infection in mice. Aliment Pharmacol Ther. 2003. 18:24–38.17. Aristoteli LP, O'Rourke JL, Danon S, Larsson H, Mellgard B, Mitchell H, Lee A. Urea, fluorofamide, and omeprazole treatments alter helicobacter colonization in the mouse gastric mucosa. Helicobacter. 2006. 11(5):460–468.18. Coghlan JG, Gilligan D, Humphries H, McKenna D, Dooley C, Sweeney E, Keane C, O'Morain C. Campylobacter pylori and recurrence of duodenal ulcers--a 12-month follow-up study. Lancet. 1987. 2(8568):1109–1111.19. Graham DY, Evans DG, Evans DJ Jr. Campylobacter pylori. The organism and its clinical relevance. J Clin Gastroenterol. 1989. 11:43–48.20. Wotherspoon AC, Ortiz-Hidalgo C, Falzon MR, Isaacson PG. Helicobacter pylori-associated gastritis and primary B-cell gastric lymphoma. Lancet. 1991. 338(8776):1175–1176.21. Cover TL, Blaser MJ. Helicobacter pylori and gastroduodenal disease. Annu Rev Med. 1992. 43:135–145.22. Lee A, Fox J, Hazell S. Pathogenicity of Helicobacter pylori: a perspective. Infect Immun. 1993. 61(5):1601–1610.23. Marshall BJ. Helicobacter pylori in peptic ulcer: have Koch's postulates been fulfilled. Ann Med. 1995. 27(5):565–568.24. Hahm KB, Kim DH, Lee KM, Lee JS, Surh YJ, Kim YB, Yoo BM, Kim JH, Joo HJ, Cho YK, Nam KT, Cho SW. Effect of long-term administration of rebamipide on Helicobacter pylori infection in mice. Aliment Pharmacol Ther. 2003. 18:24–38.25. Zhang Z, Liu ZQ, Zheng PY, Tang FA, Yang PC. Influence of efflux pump inhibitors on the multidrug resistance of Helicobacter pylori. World J Gastroenterol. 2010. 16(10):1279–1284.26. Takeuchi K, Konaka A, Nishijima M, Kato S, Yasuhiro T. Effects of pantoprazole, a novel H+/K+-ATPase inhibitor, on duodenal ulcerogenic and healing responses in rats: a comparative study with omeprazole and lansoprazole. J Gastroenterol Hepatol. 1999. 14(3):251–257.27. Cao H, Wang MW, Sun LX, Ikejima T, Hu ZQ, Zhao WH. Pharmacodynamic comparison of pantoprazole enantiomers: inhibition of acid-related lesions and acid secretion in rats and guinea-pigs. J Pharm Pharmacol. 2005. 57(7):923–927.28. Konturek SJ, Brzozowski T, Radecki T. Protective action of omeprazole, a benzimidazole derivative, on gastric mucosal damage by aspirin and ethanol in rats. Digestion. 1983. 27(3):159–164.29. Murakami I, Satoh H, Asano S, Maeda R. Role of capsaicin-sensitive sensory neurons and nitric oxide in the protective effect of lansoprazole, a proton pump inhibitor, on the gastric mucosa in rats. Jpn J Pharmacol. 1996. 72(2):137–147.30. Cao H, Wang MW, Jia JH, Wang QG, Cheng MS. Comparison of the effects of pantoprazole enantimers on gastric mucosal lesions and gastric epithelial cells in rats. J Health Sci. 2004. 50:1–8.31. Daw MA, Deegan P, Leen E, O'Moráin C. Short report: the effect of omeprazole on Helicobacter pylori and associated gastritis. Aliment Pharmacol Ther. 1991. 5(4):435–439.32. Iwahi T, Satoh H, Nakao M, Iwasaki T, Yamazaki T, Kubo K, Tamura T, Imada A. Lansoprazole, a novel benzimidazole proton pump inhibitor, and its related compounds have selective activity against Helicobacter pylori. Antimicrob Agents Chemother. 1991. 35(3):490–496.33. Hunt RH. Eradication of H. pylori infection. Am J Med. 1996. 100:42–51.34. Mobley HL, Hausinger RP. Microbial ureases: significance, regulation, and molecular characterization. Microbiol Rev. 1989. 53(1):85–108.35. Shin JH, Yang M, Nam SW, Kim JT, Myung NH, Bang WG, Roe IH. Use of egg yolk-derived immunoglobulin as an alternative to antibiotic treatment for control of Helicobacter pylori infection. Clin Diagn Lab Immunol. 2002. 9(5):1061–1066.36. Shin JH, Roe IH, Kim HG. Production of anti-Helicobacter pylori urease-specific immunoglobulin in egg yolk using an antigenic epitope of H. pylori urease. J Med Microbiol. 2004. 53:31–34.37. Malekshahi ZV, Gargari SL, Rasooli I, Ebrahimizadeh W. Treatment of Helicobacter pylori infection in mice with oral administration of egg yolk-driven anti-UreC immunoglobulin. Microb Pathog. 2011. 51(5):366–372.38. Attallah AM, Abbas AT, Ismail H, Abdel-Raouf M, El-Dosoky I. Efficacy of passive immunization with IgY antibodies to a 58-kDa H. pylori antigen on severe gastritis in BALB/c mouse model. J Immunoassay Immunochem. 2009. 30(4):359–377.39. Nomura S, Suzuki H, Masaoka T, Kurabayashi K, Ishii H, Kitajima M, Nomoto K, Hibi T. Effect of dietary anti-urease immunoglobulin Y on Helicobacter pylori infection in Mongolian gerbils. Helicobacter. 2005. 10(1):43–52.40. Lee KA, Chang SK, Lee YJ, Lee JH, Koo NS. Acid stability of anti-Helicobacter pyroli IgY in aqueous polyol solution. J Biochem Mol Biol. 2002. 35(5):488–493.41. Shin JH, Nam SW, Kim JT, Yoon JB, Bang WG, Roe IH. Identification of immunodominant Helicobacter pylori proteins with reactivity to H. pylori-specific egg-yolk immunoglobulin. J Med Microbiol. 2003. 52:217–222.42. Kazimierczuk K, Cova L, Ndeboko B, Szczyrk U, Targosz A, Brzozowski T, Sirko A. Genetic immunization of ducks for production of antibodies specific to Helicobacter pylori UreB in egg yolks. Acta Biochim Pol. 2005. 52(1):261–266.43. Horie K, Horie N, Abdou AM, Yang JO, Yun SS, Chun HN, Park CK, Kim M, Hatta H. Suppressive effect of functional drinking yogurt containing specific egg yolk immunoglobulin on Helicobacter pylori in humans. J Dairy Sci. 2004. 87(12):4073–4079.44. Suzuki H, Nomura S, Masaoka T, Goshima H, Kamata N, Kodama Y, Ishii H, Kitajima M, Nomoto K, Hibi T. Effect of dietary anti-Helicobacter pylori-urease immunoglobulin Y on Helicobacter pylori infection. Aliment Pharmacol Ther. 2004. 20:185–192.45. Pope AJ, Toseland CD, Rushant B, Richardson S, McVey M, Hills J. Effect of potent urease inhibitor, fluorofamide, on Helicobacter sp. in vivo and in vitro. Dig Dis Sci. 1998. 43(1):109–119.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Production of specific IgY Helicobacter pylori recombinant OipA protein and assessment of its inhibitory effects towards attachment of H. pylori to AGS cell line
- The Promising Effect of Egg Yolk Antibody (Immunoglobulin Yolk) on the Treatment of Helicobacter pylori-associated Gastric Diseases
- Hens immunized with live attenuated Salmonella strains expressing virulence-associated genes in avian pathogenic Escherichia coli passively transfer maternal antibodies to chicks
- Production of Egg Yolk Antibodies Specific to House Dust Mite Proteins
- Therapeutic Effect of Anti-Rotavirus Chicken Egg Yolk Immunoglobulin (IgY) on Diarrhea by Infection of Rotavirus