Lab Anim Res.
2010 Sep;26(3):225-232. 10.5625/lar.2010.26.3.225.
Neuronal Hyperexcitability Mediates Below-Level Central Neuropathic Pain after Spinal Cord Injury in Rats
- Affiliations
-
- 1Koatech Co., Pyeongtaek, Korea.
- 2Department of Anesthesiology and Pain Medicine, School of Dentistry, Kyungpook National University, Daegu, Korea.
- 3Department of Neurosurgery, Kyungpook National University Hospital, Daegu, Korea.
- 4Department of Oral physiology, School of Dentistry and BK21, Kyungpook National University, Daegu, Korea.
- 5Department of Neuroscience and Cell Biology, University of Texas Medical Branch at Galveston, Galveston, USA. ysgwak@utmb.edu
- KMID: 2312071
- DOI: http://doi.org/10.5625/lar.2010.26.3.225
Abstract
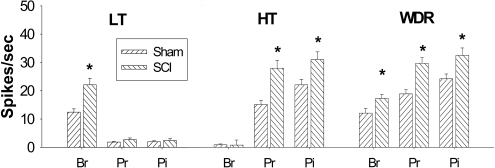
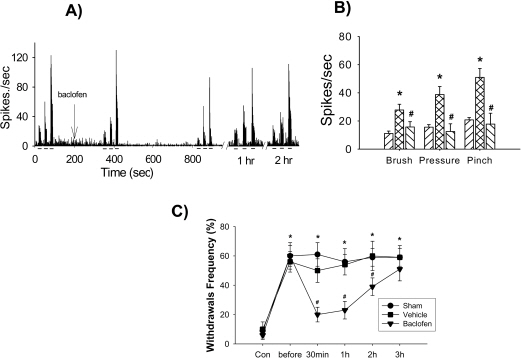
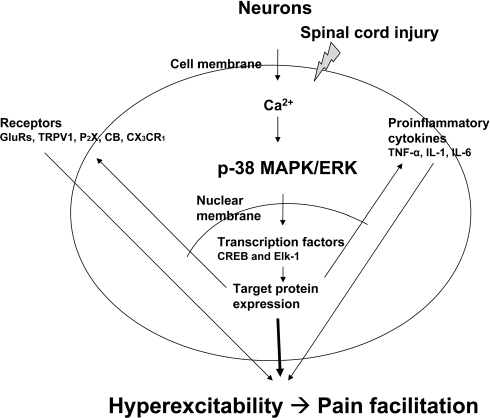
- Spinal cord injury often leads to central neuropathic pain syndromes, such as allodynic and hyperalgesic behaviors. Electrophysiologically, spinal dorsal horn neurons show enhanced activity to non-noxious and noxious stimuli as well as increased spontaneous activity following spinal cord injury, which often called hyperexcitability or central sensitization. Under hyperexcitable states, spinal neurons lose their ability of discrimination and encoding somatosensory information followed by abnormal somatosensory recognition to non-noxious and noxious stimuli. In the present review, we summarize a variety of pathophysiological mechanisms of neuronal hyperexcitability for treating or preventing central neuropathic pain syndrome following spinal cord injury.
MeSH Terms
Figure
Reference
-
Bennett A.D.., Everhart A.W.., Hulsebosch C.E.2000. Intrathecal administration of an NMDA or a non-NMDA receptor antagonist reduces mechanical but not thermal allodynia in a rodent model of chronic central pain after spinal cord injury. Brain Res. 859:72–82.
ArticleBrambilla R.., Hurtado A.., Persaud T.., Esham K.., Pearse D.D.., Oudega M.., Bethea J.R.2009. Transgenic inhibition of astroglial NF-kappa B leads to increased axonal sparing and sprouting following spinal cord injury. J. Neurochem. 110:765–778.Carlton S.M.., Du J.., Tan H.Y.., Nesic O.., Hargett G.L.., Bopp A.C.., Yamani A.., Lin Q.., Willis W.D.., Hulsebosch, Hulsebosch, , Willis, W.D. and Hulsebosch C.E.2009. Peripheral and central sensitization in remote spinal cord regions contribute to central neuropathic pain after spinal cord injury. Pain. 147:265–276.
ArticleChristensen M.D.., Hulsebosch C.E.1997. Spinal cord injury and anti-NGF treatment results in changes in CGRP density and distribution in the dorsal horn in the rat. Exp. Neurol. 147:463–475.
ArticleChu K.L.., Faltynek C.R.., Jarvis M.F.., McGaraughty S.2004. Increased WDR spontaneous activity and receptive field size in rats following a neuropathic or inflammatory injury: implications for mechanical sensitivity. Neurosci. Lett. 372:123–126.
Article123-126. Chung J.M.., Surmeier D.J.., Lee D.J.., Sorkin L.S.., Honda C.N.., Tsong Y.., Willis W.D.1986. Classification of primate spinothalamic and somatosensory thalamic neurons based on cluster analysis. J. Neurophysiol. 56:308–327.Crown E.D.., Gwak Y.S.., Ye Z.., Johnson K.M.., Hulsebosch C.E.2008. Activation of p38 MAP kinase is involved in central neuropathic pain following spinal cord injury. Exp. Neurol. 213:257–267.
ArticleCrown E.D.., Ye Z.., Johnson K.M.., Xu G.Y.., McAdoo D.J.., Hulsebosch C.E.2006. Increases in the activated forms of ERK 1/2, p38MAPK, and CREB are correlated with the expression of at-level mechanical allodynia following spinal cord injury. Exp. Neurol. 199:397–407.Dougherty K.J.., Hochman S.2008. Spinal cord injury causes plasticity in a subpopulation of lamina ⅠGABAergic interneurons. J. Neurophysiol. 100:212–223.Dougherty P.M.., Willis W.D.1991. Enhancement of spinothalamic neuron responses to chemical and mechanical stimuli following combined micro-ionotophoretic application of N-methyl-D-aspartic acid and substance P. Pain. 47:85–93.Drew G.M.., Siddall P.J.., Duggan A.W.2001. Responses of spinal neurons to cutaneous and dorsal root stimuli in rats with mechanical allodynia after contusive spinal cord injury. Brain Res. 893:59–69.Erschbamer M.., Pernold K.., Olson. L.J.2007. Inhibiting epidermal growth factor receptor improves structural, locomotor, sensory, and bladder recovery from experimental spinal cord injury. Neuroscience. 27:6428–6435.
ArticleGenovese T.., Esposito E.., Mazzon E.., Di Paola R.., Meli R.., Bramanti P.., Piomelli D.., Calignano A.., Cuzzocrea S.2008. Effects of palmitoylethanolamide on signaling pathways implicated in the development of spinal cord injury. J. Pharmacol. Exp. Ther. 326:12–23.
ArticleGwak Y.S.., Crown E.D.., Unabia G.C.., Hulsebosch C.E.2008. Propentofylline attenuates allodynia, glial activation and modulates GABAergic tone after spinal cord injury in the rat. Pain. 138:410–422.
ArticleGwak Y.S.., Hulsebosch C.E.2009. Remote astrocytic and microglial activation modulates neuronal hyperexcitability and below-level neuropathic pain after spinal injury in rat. Neuroscience. 161:895–903.
ArticleGwak Y.S.., Hulsebosch C.E.2005. Upregulation of groupⅠmetabotropic glutamate receptors in neurons and astrocytes in the dorsal horn following spinal cord injury. Exp. Neurol. 195:236–243.195, 236-243. Gwak Y.S.., Kim H.K.., Kim H.Y.., Leem J.W.2010. Bilateral hyperexcitability of thalamic VPL neurons following unilateral spinal injury in rats. J. Physiol. Sci. 60-. 59–66.Gwak Y.S.., Tan H.Y.., Nam T.S.., Paik K.S.., Hulsebosch C.E.., Leem J.W.2006. Activation of spinal GABA receptors attenuates chronic central neuropathic pain after spinal cord injury. J Neurotrauma. 23:1111–1124.
ArticleGwak Y.S.., Nam T.S.., Paik K.S.., Hulsebosch C.E.., Leem J.W.2003. ).Attenuation of mechanical hyperalgesia following spinal cord injury by administration of antibodies to nerve growth factor in the rat. Neurosci. Lett. 336:117–120.
ArticleHains B.C.., Klein J.P.., Saab C.Y.., Craner M.J.., Black J.A.., Waxman S.G.2003. Upregulation of sodium channel Nav1.3 and functional involvement in neuronal hyperexcitability associated with central neuropathic pain after spinal cord injury. J. Neurosci. 23:8881–8892.
ArticleHains B.C.., Waxman S.G.2006. Activated microglia contribute to maintenance of chronic pain after spinal cord injury. J. Neurosci. 26:4308–4317.Hou S.., Duale H.., Rabchevsky A.G.2009. Intraspinal sprouting of unmyelinated pelvic afferents after complete spinal cord injury is correlated with autonomic dysreflexia induced by visceral pain. Neuroscience. 159:369–379.
ArticleChristensen M.D.., Hulsebosch C.E.1997. Spinal cord injury and anti-NGF treatment results in changes in CGRP density and distribution in the dorsal horn in the rat. Exp. Neurol. 147:463–475.
ArticleIaci J.F.., Vecchione A.M.., Zimber M.P.., Caggiano A.O.2007. Chondroitin sulfate proteoglycans in spinal cord contusion injury and the effects of chondroitinase treatment. J. Neurotrauma. 24:1743–1759.
ArticleInoue M.., Ma L.., Aoki J.., Ueda H.2008. Simultaneous stimulation of spinal NK1 and NMDA receptors produces LPC which unergoes ATX-mediated conversion to LPA, an initiator of neuropathic pain. J. Neurochem. 107:1556–1565.Ji R.R.., Kohno T.., Moore K.A.., Woolf C.J.2003. Central sensitization and LTP: do pain and memory share similar mechanisms? Trends Neurosci. 26:696–705.
ArticleJi R.R.., Strichartz G.2004. Cell signaling and the genesis of neuropathic pain. Sci. STKE 2004. (252):reE14.Kawasaki Y.., Zhang L.., Cheng J.K.., Ji R.R.2008. Cytokine mechanisms of central sensitization: distinct and overlapping role of interleukin-1beta, interleukin-6, and tumor necrosis factor-alpha in regulating synaptic and neuronal activity in the superficial spinal cord. J. Neurosci. 28:5189–5194.Kim J.., Jung J.I.., Na H.S.., Hong S.K.., Yoon Y.W.2003. Effects of morphine on mechanical allodynia in a rat model of central neuropathic pain. Neuroreport. 14:1017–1020.
ArticleLabombarda F.., Coronel M.F.., Villar M.J.., Nicola A.F.., Gonzalez S.L.2008. Neuropathic pain and temporal expression of preprodynorphin, protein kinase C and N-methyl-D-aspartate receptor subunits after spinal cord injury. Neurosci. Lett. 447:115–119.Leem J.W.., Kim H.K.., Hulsebosch C.E.., Gwak Y.S.2010. Ionotropic glutamate receptors contribute to maintained neuronal hyperexcitability following spinal cord injury in rats. Exp. Neurol. 224:321–324.
ArticleLi J.., McRoberts J.A.., Nie J.., Ennes H.S.., Mayer E.A.2004. Electrophysiological characterization of N-methyl-D-aspartate receptors in rat dorsal root ganglia neurons. Pain. 109:443–452.Lin Z.P.., Zhu Y.L.., Johnson D.R.., Rice K.P.., Nottoli T.., Hains B.C.., McGrath J.., Waxman S.G.., Sartorelli A.C.2008. Disruption of Camp and prostaglandin E2 transport by multidrug resistance protein 4 deficiency alters cAMP-mediated signaling and nociceptive response. Mol. Pharmacol. 73:243–251.Liu J.., Wolfe D.., Hao S.., Huang S.., Glorioso J.C.., Mata M.., Fink. D.J.2004. Peripherally delivered glutamic acid decarboxylase gene therapy for spinal cord injury pain. Mol. Ther. 10:57–66.
ArticleLiu S.., Xu G.Y.., Johnson K.M.., Echetebu C.., Ye Z.S.., Hulsebosch C.E.., McAdoo D.J.2008. Regulation of interleukin-1beta by the interleukin-1 receptor antagonist in the glutamate-injured spinal cord: endogenous neuroprotection. Brain Res. 1231:63–74.McAdoo D.J.., Hughes M.G.., Nie L.., Shah B.., Clifton C.., Fullwood S.., Hulsebosch C.E.2005. The effect of glutamate receptor blockers on glutamate release following spinal cord injury. Lack of evidence for an ongoing feedback cascade of damage→glutamate release→damage→glutamate release→etc. Brain Res. 1038:92–99.Merskey H.., Bogduk D.1994. Classification of Chronic Pain, IASP Press, Seattle.Shim B.., Kim D.W.., Kim B.H.., Nam T.S.., Leem J.W.., Chung J.M.2005. Mechanical and heat sensitization of cutaneous nociceptors in rats with experimental peripheral neuropathy. Neuroscience. 132:193–201.
ArticleSiddall P.J.., Taylor D.A.., Cousins M.J.1997. Classification of pain following spinal cord injury. Spinal Cord. 35:69–75.
ArticleWillis W.D.., Coggeshall R.E.1991. Sensory Mechanism of the Spinal Cord, 2nd ed., Plenum Press, New York.Willis W.D.., Westland K.N.1997. Neuroanatomy of the pain system and of the pathways that modulate pain. J. Clin. Neurophysiol. 14:2–31.
ArticleWu W.P.., Hao J.X.., Ongini E.., Impagnatiello F.., Presotto C.., Wiesenfeld-Hallin Z.., Xu X.J.2004. A nitric oxide (NO)-releasing derivative of gabapentin, NCX8001, alleviates neuropathic pain-like behavior after spinal cord and peripheral nerve injury. Br. J. Pharmacol. 141:65–74.Yune T.Y.., Lee J.Y.., Jiang M.H.., Kim D.W.., Choi S.Y.., Oh T.H.2008. Systemic administration of PEP-1-SOD1 fusion protein improves functional recovery by inhibition of neuronal cell death after spinal cord injury. Free Radic. Biol. Med. 45:1190–1200.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Microsurgical DREZotomy for treatment of intractable central pain in patient with spinal cord injury
- Effect of the Combination of CI-988 and Morphine on Neuropathic Pain after Spinal Cord Injury in Rats
- Expression of protein kinase C-gamma mRNA on the spinal cord in a rat model of neuropathic pain
- Clinical Features of Central Neuropathic Pain after Contusive Spinal Cord Injury in Rats
- Spinal Gap Junction Channels in Neuropathic Pain