Korean J Urol.
2008 Sep;49(9):837-843.
The Different Mechanisms of Awake Micturitions between Male and Female Rats Using an Overactive Model with Intravesical PGE2 Instillation
- Affiliations
-
- 1Department of Urology, Inha University College of Medicine by BK21 Project, Incheon, Korea. lt11@inha.ac.kr
Abstract
-
PURPOSE: We wanted to obtain informations on the different mechanisms of awake micturitions between male and female rats by using an overactive model with intravesical PGE2 instillation.
MATERIALS AND METHODS
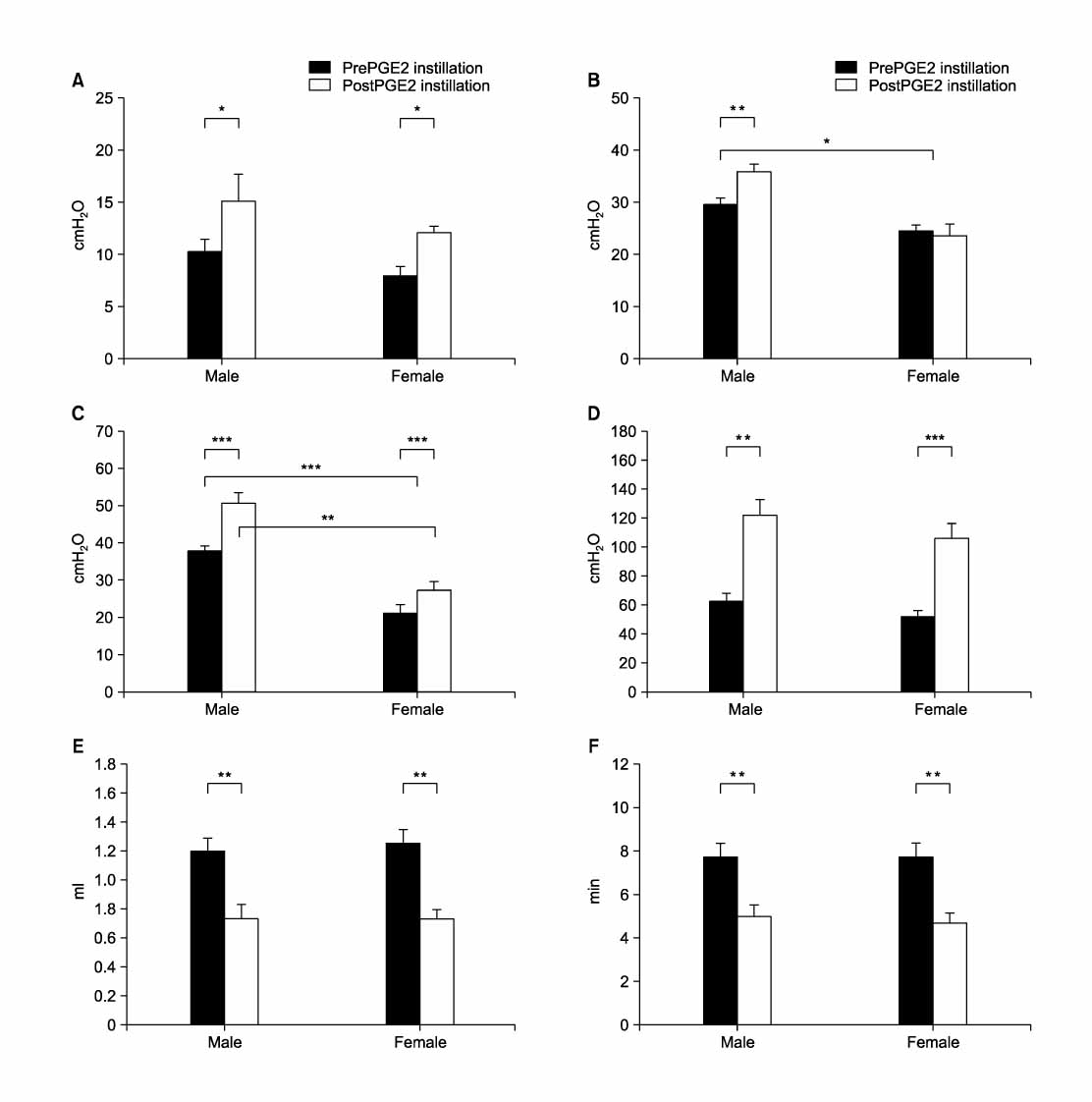
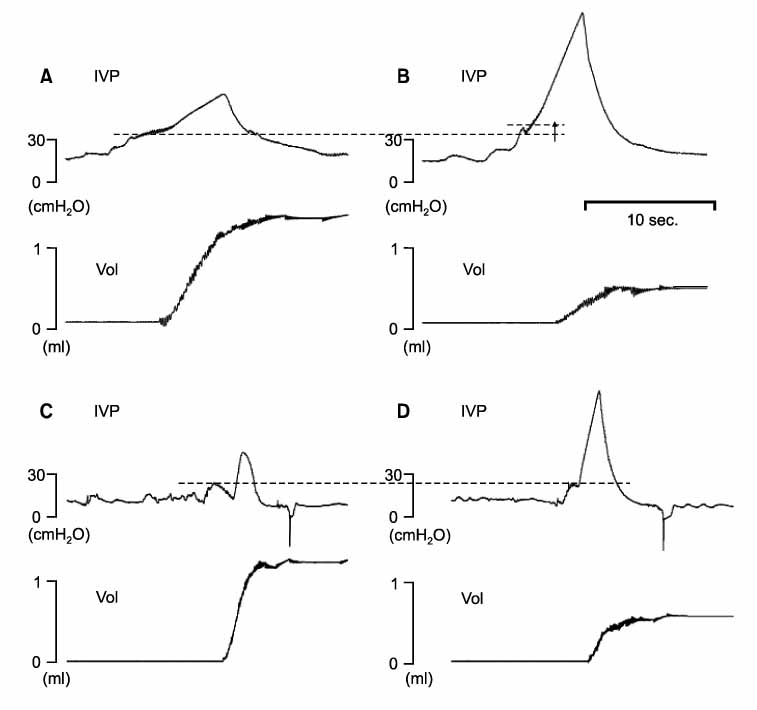
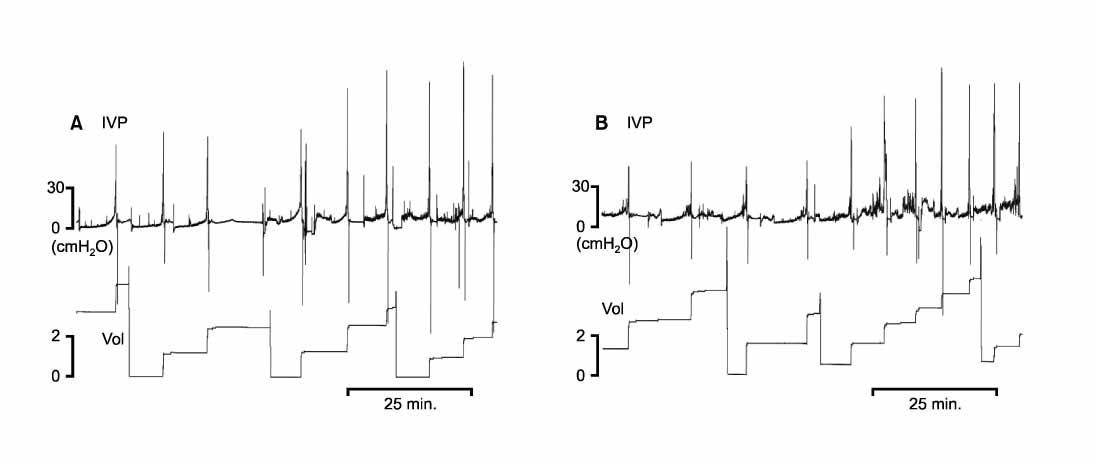
Sprague Dawley rats(6 male, 6 female) were used. A catheter was implanted into the bladder to record the intravesical pressure. Three days later, the awake cystometry was performed, and PGE2 was given intravesically to induce detrusor overactivity(DO). With using the conventional pressure and volume parameters, a new parameter of flow pressure was investigated.
RESULTS
When recorded as the flow pressure, the male rats exhibited higher urethral resistance than did the female rats in the normal state. The male rats showed higher urethral resistances after DO was induced, than those before the DO. However, the female rats did not show increased urethral resistance after DO was induced.
CONCLUSIONS
An increase in urethral resistance through the outlet region was induced in male rats after intravesical PGE2 instillation, but this didn't occur in female rats. This result indicates that overactive bladder has different mechanisms and responses in different genders.
Keyword
MeSH Terms
Figure
Reference
-
1. Abrams P, Cardozo L, Fall M, Griffiths D, Rosier P, Ulmsten U, et al. The standardisation of terminology of lower urinary tract function: report from the Standardisation Sub-committee of the International Continence Society. Neurourol Urodyn. 2002. 21:167–178.2. Milsom I, Abrams P, Cardozo L, Roberts RG, Thuroff J, Wein AJ. How widespread are the symptoms of an overactive bladder and how are they managed? A population-based prevalence study. BJU Int. 2001. 87:760–766.3. Davila GW, Neimark M. The overactive bladder: prevalence and effects on quality of life. Clin Obstet Gynecol. 2002. 45:173–181.4. Lee KS, Lee YS. Overactive bladder. Korean J Urol. 2007. 48:1191–1208.5. Stewart WF, Van Rooyen JB, Cundiff GW, Abrams P, Herzog AR, Corey R, et al. Prevalence and burden of overactive bladder in the United States. World J Urol. 2003. 20:327–336.6. Knutson T, Edlund C, Fall M, Dahlstrand C. BPH with coexisting overactive bladder dysfunction--an everyday urological dilemma. Neurourol Urodyn. 2001. 20:237–247.7. Streng T, Santti R, Talo A. Similarities and differences in female and male rat voiding. Neurourol Urodyn. 2002. 21:136–141.8. Streng T, Santti R, Andersson KE, Talo A. The role of the rhabdosphincter in female rat voiding. BJU Int. 2004. 94:138–142.9. Lee T, Andersson KE, Streng T, Hedlund P. Simultaneous registration of intraabdominal and intravesical pressures during cystometry in conscious rats-effects of bladder outlet obstruction and intravesical PGE2. Neurourol Urodyn. 2008. 27:88–95.10. Conte B, Maggi CA, Giachetti A, Parlani M, Lopez G, Manzini S. Intraurethral capsaicin produces reflex activation of the striated urethral sphincter in urethane-anesthetized male rats. J Urol. 1993. 150:1271–1277.11. Andersson KE. Bladder activation: afferent mechanisms. Urology. 2002. 59:5 Suppl 1. 43–50.12. Andersson KE, Hedlund P. Pharmacologic perspective on the physiology of the lower urinary tract. Urology. 2002. 60:5 Suppl 1. 13–20.13. Chung JS, Yoo HS, Lee T. Urethral dysfunction in a non-insulin dependent diabetes mellitus rat model. Korean J Urol. 2006. 47:1007–1012.14. Hernandez RD, Hurwitz RS, Foote JE, Zimmern PE, Leach GE. Nonsurgical management of threatened upper urinary tracts and incontinence in children with myelomeningocele. J Urol. 1994. 152:1582–1585.15. Bruschini H, Almeida FG, Srougi M. Upper and lower urinary tract evaluation of 104 patients with myelomeningocele without adequate urological management. World J Urol. 2006. 24:224–228.16. Schroder A, Newgreen D, Andersson KE. Detrusor responses to prostaglandin E2 and bladder outlet obstruction in wild-type and Ep1 receptor knockout mice. J Urol. 2004. 172:1166–1170.17. Jordan C. Androgen receptor (AR) immunoreactivity in rat pudendal motoneurons: implications for accessory proteins. Horm Behav. 1997. 32:1–10.18. McKenna KE, Nadelhaft I. The organization of the pudendal nerve in the male and female rat. J Comp Neurol. 1986. 248:532–549.19. Kontani H, Shiraoya C. Sex differences in urethral pressure response to electrical stimulation of the hypogastric nerves in rats. J Urol. 2000. 163:1364–1368.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Intravesical PGE2 Administration in Conscious Rats as an Experimental Model of Detrusor Overactivity Observed by Simultaneous Registrations of Intravesical and Intraabdominal Pressures
- Urodynamic Effects of Propiverine on Detrusor Overactivity and Abdominal Straining during Voiding in Awake Rats with Intravesical Prostaglandin E2 Instillation
- The Value and Limitations of Intravesical Prostaglandin E2 (PGE2)-induced Bladder Hyperactivity as an Overactive Bladder Model in Normal, Conscious Sprague-Dawley Rats
- Dissimilar Effects of Tolterodine on Detrusor Overactivity in Awake Rats with Chemical Cystitis and Partial Bladder Outlet Obstruction
- Effects of Intravesical Instillation of Cyclooxygenase-2 Inhibitor on Cyclophosphamide-induced Overactive Bladder