Korean J Urol.
2008 Jun;49(6):526-532.
The Value and Limitations of Intravesical Prostaglandin E2 (PGE2)-induced Bladder Hyperactivity as an Overactive Bladder Model in Normal, Conscious Sprague-Dawley Rats
- Affiliations
-
- 1Department of Urology, Inha University College of Medicine by BK21 Project, Incheon, Korea. lt11@inha.ac.kr
Abstract
-
PURPOSE: Establishing an appropriate animal model is essential for investigating the yet unknown mechanisms of overactive bladder(OAB). Prostanoids are an already well known intrinsic cause of overactive bladder in both animal and human. Awake animal models with prostanoids are already being used as an OAB model, but there is no standardization of methods, and especially for the concentration of the administrated prostanoids. So in this study, we tried to objectively establish the standardized concentration of prostanoids and its effect on urination through urodynamic studies with using non-anesthetized Dawley rats.
MATERIALS AND METHODS
We divided 18 female rats(215-280g) into 3 groups of six rats each and we injected 30micrometer, 50micrometer or 100micrometer of PGE2, respectively. A catheter was placed inside the bladder through an incision in the abdominal wall. After three days, cystometry was performed with the arts in an awake state. During cystometry, we administrated saline into the bladder to identify the usual voiding status of the rat. In comparison, the saline with PGE2 at 3 different concentrations(30, 50, 100micrometer) was administrated into the bladder(10ml/h).
RESULTS
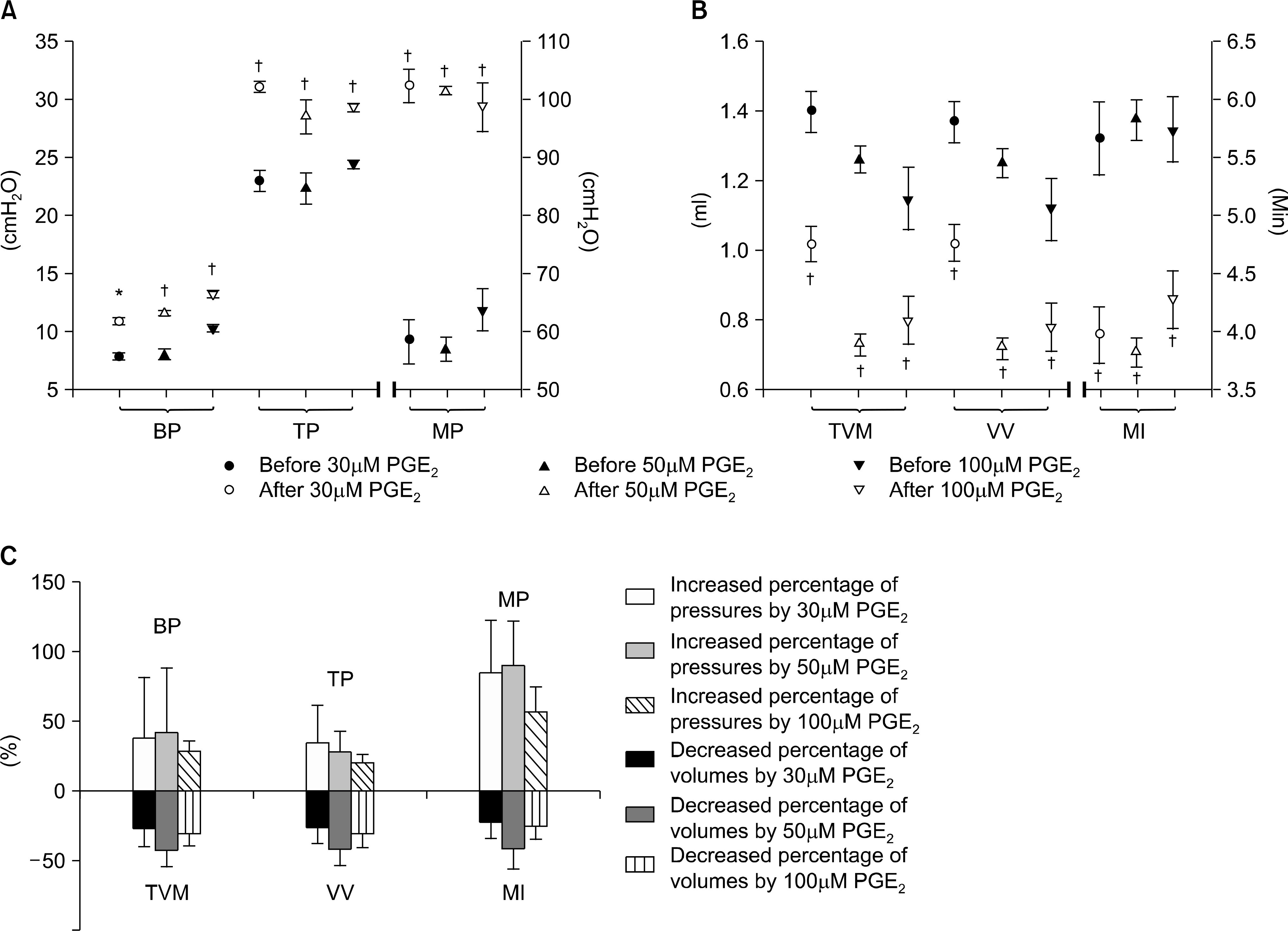
Each group of the 30, 50, 100micrometer PGE2 administered rats showed an increased level of the basal pressure, the threshold pressure and the maximal pressure compared to the state before administration of PGE2. Also, the bladder capacity, voided volume and micturition interval decreased by a statistically acceptable amount, like was seen in the OAB model. There was a trend that showed a greater increase in the pressure parameters and a greater decrease in the volume parameters in the 50micrometer PGE2 group compared to the 30micrometer PGE2 group, but there were no differences between the 50micrometer and 100micrometer groups.
CONCLUSIONS
In the normal awake rats, PGE2 induced overactive bladder to a statistically significant amount for all concentrations(30, 50, 100micrometer). Among these groups, the concentration of 50micrometer provoked OAB most effectively, and the higher concentration of PGE2(100micrometer) did not provoke a more efficient OAB, which might have been due to the characteristics of the intrinsic material in the bladders. Thus, we recommend PGE2 50micrometer for efficient induction of OAB.
Keyword
MeSH Terms
Figure
Reference
-
1. Andersson KE. Antimuscarinics for treatment of overactive bladder. Lancet Neurol. 2004; 3:46–53.
Article2. Andersson KE, Appell R, Awad SA, Chapple C, Druts H, Finkbeiner A, et al. Pharmacological treatment of urinary incontinence. Abrams P, Cardozo L, Khoury S, Wein A, editors. editors.Incontinence. Plymouth: Health Publication Ltd.;2002. p. 481–91.3. Andersson KE. Overactive bladder-pharmacological aspects. Scand J Urol Nephrol. 2002; 210(Suppl):72–81.
Article4. Abrams P, Cardozo L, Fall M, Griffiths D, Rosier P, Ulmsten U, et al. The standardisation of terminology of lower urinary tract function: report from the Standardisation Sub-committee of the International Continence Society. Neurourol Urodyn. 2002; 21:167–78.
Article5. Schröder A, Uvelius B, Newgreen D, Andersson KE. Bladder overactivity in mice after 1 week of outlet obstruction. Mainly afferent dysfunction? J Urol. 2003; 170:1017–21.6. Takeda H, Yamazaki Y, Igawa Y, Kaidoh K, Akahane S, Miyata H, et al. Effect of ß3-adrenoceptor stimulation on prostaglandin (E2)-induced bladder hyperactivity and on the cardiovascular system in conscious rats. Neurourol Urodyn. 2002; 21:558–65.7. Meini S, Lecci A, Cucchi P, Catalioto RM, Criscuoli M, Maggi CA. Inflammation modifies the role of cyclooxygenases in the contractile response of the rat detrusor smooth muscle to kinin agonists. J Pharmacol Exp Ther. 1998; 287:137–43.8. Schröder A, Newgreen D, Andersson KE. Detrusor responses to prostaglandin E2 and bladder outlet obstruction in wild-type and EP1 receptor knockout mice. J Urol. 2004; 172:1166–70.9. Pinna C, Zanardo R, Puglisi L. Prostaglandin-release impairment in the bladder epithelium of streptozotocin-induced diabetic rats. Eur J Pharmacol. 2000; 388:267–73.
Article10. Wheeler MA, Hausladen DA, Yoon JH, Weiss RM. Prostaglandin E2 production and cyclooxygenase-2 induction in human urinary tract infections and bladder cancer. J Urol. 2002; 168:1568–72.
Article11. Palea S, Toson G, Pietra C, Trist DG, Artibani W, Romano O, et al. Pharmacological characterization of thromboxane and prostanoid receptors in human isolated urinary bladder. Br J Pharmacol. 1998; 124:865–72.
Article12. Morikawa K, Ichihashi M, Kakiuchi M, Yamauchi T, Kato H, Ito Y, et al. Effects of various drugs on bladder function in conscious rats. Jpn J Pharmacol. 1989; 50:369–76.
Article13. Pandita RK, Fujiwara M, Alm P, Andersson KE. Cystometric evaluation of bladder function in non-anesthetized mice with and without bladder outlet obstruction. J Urol. 2000; 164:1385–9.
Article14. Pandita RK, Andersson KE. Intravesical adenosine triphosphate stimulates the micturation reflex in awake, freely moving rats. J Urol. 2002; 168:1230–4.15. Gu BJ, Ishizuka O, Igawa Y, Nishizawa O, Andersson KE. Role of supraspinal tachykinins for micturition in conscious rats with and without bladder outlet obstruction. Naunyn Schmiedeberg's Arch Pharmacol. 2000; 361:543–8.
Article16. Ishizuka O, Mattiasson A, Andersson KE. Prostaglandin E2-induced bladder hyperactivity in normal, conscious rats: involvement of tachykinins? J Urol. 1995; 153:2034–8.17. Lee T, Hedlund P, Newgreen D, Andersson KE. Urodynamic effects of a novel EP (1) receptor antagonist in normal rats and rats with bladder outlet obstructruction. J Urol. 2007; 177:1562–7.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The Different Mechanisms of Awake Micturitions between Male and Female Rats Using an Overactive Model with Intravesical PGE2 Instillation
- Urodynamic Effects of Propiverine on Detrusor Overactivity and Abdominal Straining during Voiding in Awake Rats with Intravesical Prostaglandin E2 Instillation
- Intravesical PGE2 Administration in Conscious Rats as an Experimental Model of Detrusor Overactivity Observed by Simultaneous Registrations of Intravesical and Intraabdominal Pressures
- Application and Limitations of Awake Cystometry in Sprague-Dawley Rats with Partial Bladder Outlet Obstruction as a Model of Overactive Bladder or Obstruction
- Effects of Intravesical Instillation of Cyclooxygenase-2 Inhibitor on Cyclophosphamide-induced Overactive Bladder