J Dent Anesth Pain Med.
2015 Sep;15(3):129-134.
Comparison of the hemodynamic effects of propofol and ketamine as anesthetic induction agents during high-dose remifentanil administration: a single-center retrospective comparative study
- Affiliations
-
- 1Division of Clinical Physiology, Department of Translational Medical Sciences, Nagasaki University Graduate School of Biomedical Sciences, Nagasaki, Japan. sanuki@nagasaki-u.ac.jp
- 2Department of Dental Anesthesiology, Nagasaki University Hospital, Nagasaki, Japan.
- 3Division of Clinical Oral Oncology, Department of Translational Medical Sciences, Nagasaki University Graduate School of Biomedical Sciences, Nagasaki, Japan.
- 4Division of Regenerative Oral Surgery, Department of Translational Medical Sciences, Nagasaki University Graduate School of Biomedical Sciences, Nagasaki, Japan.
Abstract
- BACKGROUND
We hypothesized that ketamine, when administered as the anesthetic induction agent, may prevent cardiovascular depression during high-dose remifentanil administration, unlike propofol. To test our hypothesis, we retrospectively compared the hemodynamic effects of ketamine, during high-dose remifentanil administration, with those of propofol.
METHODS
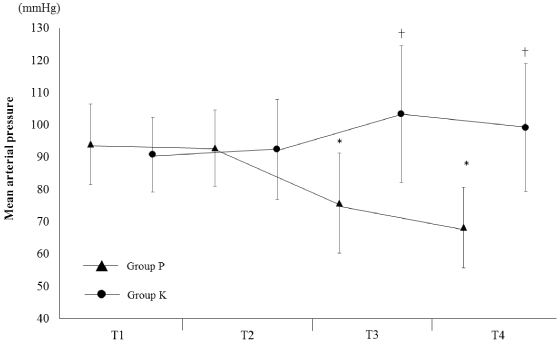
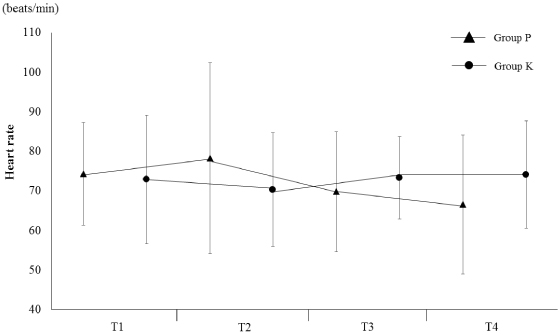
Thirty-eight patients who underwent oral surgery at the Nagasaki University Hospital between April 2014 and June 2015 were included in this study. Anesthesia was induced by the following procedure: First, high-dose remifentanil (0.3-0.5 µg/kg/min) was administered 2-3 min before anesthesia induction; next, the anesthetic induction agent, either propofol (Group P) or ketamine (Group K), was administered. Mean arterial pressure (MAP) and the heart rate were recorded by the automated anesthesia recording system at four time points: immediately before the administration of high-dose remifentanil (T1); immediately before the administration of propofol or ketamine (T2); 2.5 min (T3), and 5 min (T4) after the administration of the anesthetic induction agent.
RESULTS
In Group P, the MAP at T3 (75.7 ± 15.5 mmHg, P = 0.0015) and T4 (68.3 ± 12.5 mmHg, P < 0.001) were significantly lower than those at T1 (94.0 ± 12.4 mmHg). However, the MAP values in the K group were very similar (P = 0.133) at all time points. The heart rates in both Groups P (P = 0.254) and K (P = 0.859) remained unchanged over time.
CONCLUSIONS
We showed that ketamine, when administered as the anesthetic induction agent during high-dose remifentanil administration, prevents cardiovascular depression.
MeSH Terms
Figure
Reference
-
1. Kurata Y. High-dose remifentanil anesthesia. J Clin Anesth. 2008; 32:1692–1696.2. Albertin A, Casati A, Federica L, Roberto V, Travaglini V, Bergonzi P, et al. The effect-site concentration of remifentanil blunting cardiovascular responses to tracheal intubation and skin incision during bispectral index-guided propofol anesthesia. Anesth Analg. 2005; 101:125–130.
Article3. Kortelainen J, Koskinen M, Mustola S, Seppänen T. Effects of remifentanil on the spectrum and quantitative parameters of electroencephalogram in propofol anesthesia. Anesthesiology. 2009; 111:574–583.
Article4. Tweed WA, Minuck M, Mymin D. Circulatory responses to ketamine anesthesia. Anesthesiology. 1972; 37:613–619.
Article5. Haas DA, Harper DG. Ketamine: a review of its pharmacologic properties and use in ambulatory anesthesia. Anesth Prog. 1992; 3:61–68.6. Ogletree ML, Sprung J, Moravec CS. Effects of remifentanil on the contractility of failing human heart muscle. J Cardiothorac Vasc Anesth. 2005; 19:763–767.
Article7. Duman A, Saide Sahin A, Esra Atalik K, Öztin Ögün C, Basri Ulusoy H, Durgut K, et al. The in vitro effects of remifentanil and fentanyl on isolated human right atria and saphenous veins. J Cardiothorac Vasc Anesth. 2003; 17:465–469.
Article8. Sprung J, Schuetz SM, Stewart RW, Moravec CS. Effects of ketamine on the contractility of failing and nonfailing human heart muscles in vitro. Anesthesiology. 1998; 88:1202–1210.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Changes of Bispectral Index and Auditory Evoked Potential Index during General Anesthesia with Propofol, Midazolam and Ketamine
- Effect of Ketamine Pretreatment on Injection Pain and Hemodynamic Changes during Anesthesia Induction with Propofol
- Comparative Maternal and Neonatal Effects of Propofol, Propofol-Ketamine and Ketamine as Induction Agents in Cesarean Section
- The Effects of Different Doses of Remifentanil on Propofol Injection Pain: A Placebo Controlled Comparison of Ketamine
- What is an Optimal Effect Site Concentration of Remifentanil for Minimizing the Hemodynamic Change to Endotracheal Intubation using Light Wand?