Usefulness of Measuring Thyroid Stimulating Antibody at the Time of Antithyroid Drug Withdrawal for Predicting Relapse of Graves Disease
- Affiliations
-
- 1Department of Internal Medicine, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea. wongukim@amc.seoul.kr
- 2Department of Internal Medicine, Cancer Center, Dongnam Institute of Radiological & Medical Sciences, Busan, Korea.
- 3Department of Nuclear Medicine, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea.
- KMID: 2308861
- DOI: http://doi.org/10.3803/EnM.2016.31.2.300
Abstract
- BACKGROUND
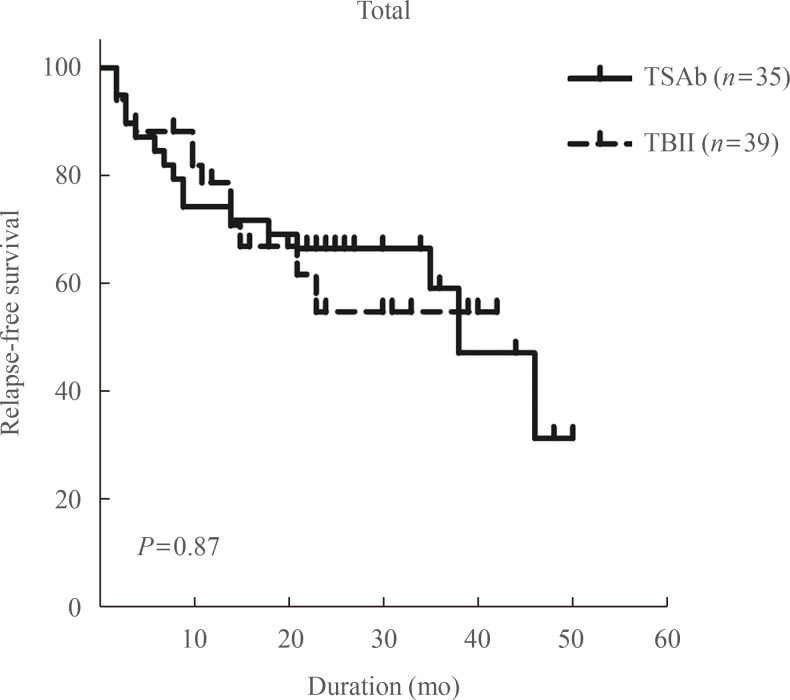
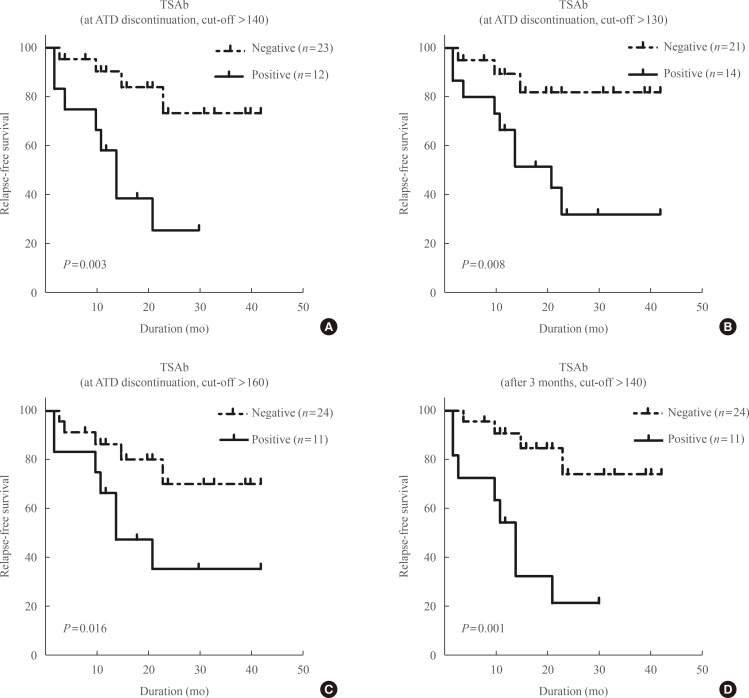
Hyperthyroidism relapse in Graves disease after antithyroid drug (ATD) withdrawal is common; however, measuring the thyrotropin receptor antibody (TRAb) at ATD withdrawal in order to predict outcomes is controversial. This study compared measurement of thyroid stimulatory antibody (TSAb) and thyrotropin-binding inhibitory immunoglobulin (TBII) at ATD withdrawal to predict relapse.
METHODS
This retrospective study enrolled patients with Graves disease who were treated with ATDs and whose serum thyroid-stimulating hormone levels were normal after receiving low-dose ATDs. ATD therapy was stopped irrespective of TRAb positivity after an additional 6 months of receiving the minimum dose of ATD therapy. Patients were followed using thyroid function tests and TSAb (TSAb group; n=35) or TBII (TBII group; n=39) every 3 to 6 months for 2 years after ATD withdrawal.
RESULTS
Twenty-eight patients (38%) relapsed for a median follow-up of 21 months, and there were no differences in baseline clinical characteristics between groups. In the TSAb group, relapse was more common in patients with positive TSAb at ATD withdrawal (67%) than patients with negative TSAb (17%; P=0.007). Relapse-free survival was shorter in TSAb-positive patients. In the TBII group, there were no differences in the relapse rate and relapse-free survivals according to TBII positivity. For predicting Graves disease relapse, the sensitivity and specificity of TSAb were 63% and 83%, respectively, whereas those of TBII were 28% and 65%.
CONCLUSION
TSAb at ATD withdrawal can predict the relapse of Graves hyperthyroidism, but TBII cannot. Measuring TSAb at ATD withdrawal can assist with clinical decisions making for patients with Graves disease.
Keyword
MeSH Terms
-
Follow-Up Studies
Graves Disease*
Humans
Hyperthyroidism
Immunoglobulins
Immunoglobulins, Thyroid-Stimulating*
Prognosis
Receptors, Thyrotropin
Recurrence*
Retrospective Studies
Sensitivity and Specificity
Thyroid Function Tests
Thyroid Gland*
Thyrotropin
Immunoglobulins
Immunoglobulins, Thyroid-Stimulating
Receptors, Thyrotropin
Thyrotropin
Figure
Cited by 7 articles
-
Graves' Disease: Can It Be Cured?
Wilmar M. Wiersinga
Endocrinol Metab. 2019;34(1):29-38. doi: 10.3803/EnM.2019.34.1.29.The Recurrence Rate of Graves' Disease among Patients with Subclinical Thyrotoxicosis after Initial Remission with Antithyroid Agents
Myoung Sook Shim, Soo Min Nam, Jin Sae Yoo, Hae Kyung Kim, Sang Jun Lee, Mi Young Lee
Int J Thyroidol. 2017;10(2):77-81. doi: 10.11106/ijt.2017.10.2.77.Medical Treatment of Graves' Disease
Hyun-Kyung Chung
Int J Thyroidol. 2019;12(2):79-84. doi: 10.11106/ijt.2019.12.2.79.Changes in Thyroid Peroxidase and Thyroglobulin Antibodies Might Be Associated with Graves' Disease Relapse after Antithyroid Drug Therapy
Yun Mi Choi, Mi Kyung Kwak, Sang Mo Hong, Eun-Gyoung Hong
Endocrinol Metab. 2019;34(3):268-274. doi: 10.3803/EnM.2019.34.3.268.Antithyroid Drug Treatment in Graves’ Disease
Jae Hoon Chung
Endocrinol Metab. 2021;36(3):491-499. doi: 10.3803/EnM.2021.1070.The Early Changes in Thyroid-Stimulating Immunoglobulin Bioassay over Anti-Thyroid Drug Treatment Could Predict Prognosis of Graves’ Disease
Jin Yu, Han-Sang Baek, Chaiho Jeong, Kwanhoon Jo, Jeongmin Lee, Jeonghoon Ha, Min Hee Kim, Jungmin Lee, Dong-Jun Lim
Endocrinol Metab. 2023;38(3):338-346. doi: 10.3803/EnM.2023.1664.Dynamic Risk Model for the Medical Treatment of Graves’ Hyperthyroidism according to Treatment Duration
Meihua Jin, Chae A Kim, Min Ji Jeon, Won Bae Kim, Tae Yong Kim, Won Gu Kim
Endocrinol Metab. 2024;39(4):579-589. doi: 10.3803/EnM.2024.1918.
Reference
-
1. Bahn Chair RS, Burch HB, Cooper DS, Garber JR, Greenlee MC, Klein I, et al. Hyperthyroidism and other causes of thyrotoxicosis: management guidelines of the American Thyroid Association and American Association of Clinical Endocrinologists. Thyroid. 2011; 21:593–646. PMID: 21510801.
Article2. Moon JH, Yi KH. The diagnosis and management of hyperthyroidism in Korea: consensus report of the Korean Thyroid Association. Endocrinol Metab (Seoul). 2013; 28:275–279. PMID: 24396691.
Article3. Kamath C, Adlan MA, Premawardhana LD. The role of thyrotrophin receptor antibody assays in Graves' disease. J Thyroid Res. 2012; 2012:525936. PMID: 22577596.
Article4. Kim WB. Clinical applications of thyrotropin binding inhibitor immunoglobulin (TBII) assays. J Korean Endocr Soc. 2008; 23:174–178.
Article5. Weetman AP, McGregor AM. Autoimmune thyroid disease: further developments in our understanding. Endocr Rev. 1994; 15:788–830. PMID: 7705281.
Article6. Feldt-Rasmussen U, Schleusener H, Carayon P. Meta-analysis evaluation of the impact of thyrotropin receptor antibodies on long term remission after medical therapy of Graves' disease. J Clin Endocrinol Metab. 1994; 78:98–102. PMID: 8288723.
Article7. Massart C, Hody B, Mouchel L, Edan G, Nicol M. Assays for thyrotropin-receptor binding and thyroid-stimulating antibodies in sera from patients with Graves' disease. Clin Chem. 1986; 32:1332–1335. PMID: 2872980.
Article9. Mazza E, Carlini M, Flecchia D, Blatto A, Zuccarini O, Gamba S, et al. Long-term follow-up of patients with hyperthyroidism due to Graves' disease treated with methimazole. Comparison of usual treatment schedule with drug discontinuation vs continuous treatment with low methimazole doses: a retrospective study. J Endocrinol Invest. 2008; 31:866–872. PMID: 19092290.
Article10. Orgiazzi J, Madec AM. Reduction of the risk of relapse after withdrawal of medical therapy for Graves' disease. Thyroid. 2002; 12:849–853. PMID: 12487766.
Article11. Zingrillo M, D'Aloiso L, Ghiggi MR, Di Cerbo A, Chiodini I, Torlontano M, et al. Thyroid hypoechogenicity after methimazole withdrawal in Graves' disease: a useful index for predicting recurrence? Clin Endocrinol (Oxf). 1996; 45:201–206. PMID: 8881453.
Article12. Varsamidis K, Varsamidou E, Mavropoulos G. Doppler ultrasonography in predicting relapse of hyperthyroidism in Graves' disease. Acta Radiol. 2000; 41:45–48. PMID: 10665869.
Article13. Prakash R. Prediction of remission in Graves' disease treated with long-term carbimazole therapy: evaluation of technetium-99m thyroid uptake and TSH concentrations as prognostic indicators. Eur J Nucl Med. 1996; 23:118–122. PMID: 8925844.
Article14. Hwang S, Shin DY, Song MK, Lee EJ. High cut-off value of a chimeric TSH receptor (Mc4)-based bioassay may improve prediction of relapse in Graves' disease for 12 months. Endocrine. 2015; 48:89–95. PMID: 24968734.15. Maugendre D, Massart C. Clinical value of a new TSH binding inihibitory activity assay using human TSH receptors in the follow-up of antithyroid drug treated Graves disease Comparison with thyroid stimulating antibody bioassay. Clin Endocrinol (Oxf). 2001; 54:89–96. PMID: 11167931.
Article16. Schott M, Morgenthaler NG, Fritzen R, Feldkamp J, Willenberg HS, Scherbaum WA, et al. Levels of autoantibodies against human TSH receptor predict relapse of hyperthyroidism in Graves' disease. Horm Metab Res. 2004; 36:92–96. PMID: 15002058.
Article17. Quadbeck B, Hoermann R, Hahn S, Roggenbuck U, Mann K, Janssen OE. Binding, stimulating and blocking TSH receptor antibodies to the thyrotropin receptor as predictors of relapse of Graves' disease after withdrawal of antithyroid treatment. Horm Metab Res. 2005; 37:745–750. PMID: 16372228.
Article18. Quadbeck B, Hoermann R, Roggenbuck U, Hahn S, Mann K, Janssen OE, et al. Sensitive thyrotropin and thyrotropinreceptor antibody determinations one month after discontinuation of antithyroid drug treatment as predictors of relapse in Graves' disease. Thyroid. 2005; 15:1047–1054. PMID: 16187913.
Article19. Schott M, Eckstein A, Willenberg HS, Nguyen TB, Morgenthaler NG, Scherbaum WA. Improved prediction of relapse of Graves' thyrotoxicosis by combined determination of TSH receptor and thyroperoxidase antibodies. Horm Metab Res. 2007; 39:56–61. PMID: 17226115.
Article20. Okamoto Y, Tanigawa S, Ishikawa K, Hamada N. TSH receptor antibody measurements and prediction of remission in Graves' disease patients treated with minimum maintenance doses of antithyroid drugs. Endocr J. 2006; 53:467–472. PMID: 16820704.
Article21. Cappelli C, Gandossi E, Castellano M, Pizzocaro C, Agosti B, Delbarba A, et al. Prognostic value of thyrotropin receptor antibodies (TRAb) in Graves' disease: a 120 months prospective study. Endocr J. 2007; 54:713–720. PMID: 17675761.
Article22. Giuliani C, Cerrone D, Harii N, Thornton M, Kohn LD, Dagia NM, et al. A TSHR-LH/CGR chimera that measures functional thyroid-stimulating autoantibodies (TSAb) can predict remission or recurrence in Graves' patients undergoing antithyroid drug (ATD) treatment. J Clin Endocrinol Metab. 2012; 97:E1080–E1087. PMID: 22492869.
Article23. Takasu N, Yamashiro K, Komiya I, Ochi Y, Sato Y, Nagata A. Remission of Graves' hyperthyroidism predicted by smooth decreases of thyroid-stimulating antibody and thyrotropin-binding inhibitor immunoglobulin during antithyroid drug treatment. Thyroid. 2000; 10:891–896. PMID: 11081255.
Article24. Schott M, Minich WB, Willenberg HS, Papewalis C, Seissler J, Feldkamp J, et al. Relevance of TSH receptor stimulating and blocking autoantibody measurement for the prediction of relapse in Graves' disease. Horm Metab Res. 2005; 37:741–744. PMID: 16372227.
Article25. Barbesino G, Tomer Y. Clinical review: clinical utility of TSH receptor antibodies. J Clin Endocrinol Metab. 2013; 98:2247–2255. PMID: 23539719.26. Zophel K, Roggenbuck D, Schott M. Clinical review about TRAb assay's history. Autoimmun Rev. 2010; 9:695–700. PMID: 20594972.27. Tozzoli R, Bagnasco M, Giavarina D, Bizzaro N. TSH receptor autoantibody immunoassay in patients with Graves' disease: improvement of diagnostic accuracy over different generations of methods. Systematic review and meta-analysis. Autoimmun Rev. 2012; 12:107–113. PMID: 22776786.
Article28. Jeon MJ, Kim WG, Jang EK, Choi YM, Lee YM, Sung TY, et al. Thyroglobulin level in fine-needle aspirates for preoperative diagnosis of cervical lymph node metastasis in patients with papillary thyroid carcinoma: two different cutoff values according to serum thyroglobulin level. Thyroid. 2015; 25:410–416. PMID: 25607926.
Article29. Carella C, Mazziotti G, Sorvillo F, Piscopo M, Cioffi M, Pilla P, et al. Serum thyrotropin receptor antibodies concentrations in patients with Graves' disease before, at the end of methimazole treatment, and after drug withdrawal: evidence that the activity of thyrotropin receptor antibody and/or thyroid response modify during the observation period. Thyroid. 2006; 16:295–302. PMID: 16571093.
Article30. Huh JE, Suk JH, Kim MK, Choi IJ, Son SM, Kim IJ, et al. Clinical usefulness of the second generation TSH-binding inhibitory immunoglobulin assay using recombinant human TSH receptor in patients with Graves' disease. J Korean Endocr Soc. 2008; 23:179–185.
Article31. Lytton SD, Li Y, Olivo PD, Kohn LD, Kahaly GJ. Novel chimeric thyroid-stimulating hormone-receptor bioassay for thyroid-stimulating immunoglobulins. Clin Exp Immunol. 2010; 162:438–446. PMID: 21070207.
Article32. Lytton SD, Ponto KA, Kanitz M, Matheis N, Kohn LD, Kahaly GJ. A novel thyroid stimulating immunoglobulin bioassay is a functional indicator of activity and severity of Graves' orbitopathy. J Clin Endocrinol Metab. 2010; 95:2123–2131. PMID: 20237164.
Article33. Sun X, Shan Z, Teng W. Effects of increased iodine intake on thyroid disorders. Endocrinol Metab (Seoul). 2014; 29:240–247. PMID: 25309781.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Clinical Applications of TSH Receptor Antibodies in Thyroid Diseases
- Changes in Thyroid Peroxidase and Thyroglobulin Antibodies Might Be Associated with Graves' Disease Relapse after Antithyroid Drug Therapy
- Treatment of relapsed hyperthyroidism
- Clinical Implication of TSH Receptor Antibody Measurement
- Analysis of the markers related with relapse after withdrawal of antithyroid drug in patients with Graves' disease