Korean J Androl.
2011 Apr;29(1):33-42. 10.5534/kja.2011.29.1.33.
The Changes of Testis and the Effects of Anthocyanin on Spermatogenesis in Rat Induced Varicocele
- Affiliations
-
- 1Department of Urology, The Catholic University of Korea College of Medicine, Seoul, Korea. ksw1227@catholic.ac.kr
- 2Korea Bio Medical Science Institute, Seoul, Korea.
- KMID: 2298624
- DOI: http://doi.org/10.5534/kja.2011.29.1.33
Abstract
- PURPOSE
Varicocele is known as a main cause of primary male infertility and it supposed to be associated with oxidative stress. Anthocyanin is known as a natural plant pigment and novel antioxidant. This study was designed to investigate the effects of anthocyanin on a rat model of varicocele.
MATERIALS AND METHODS
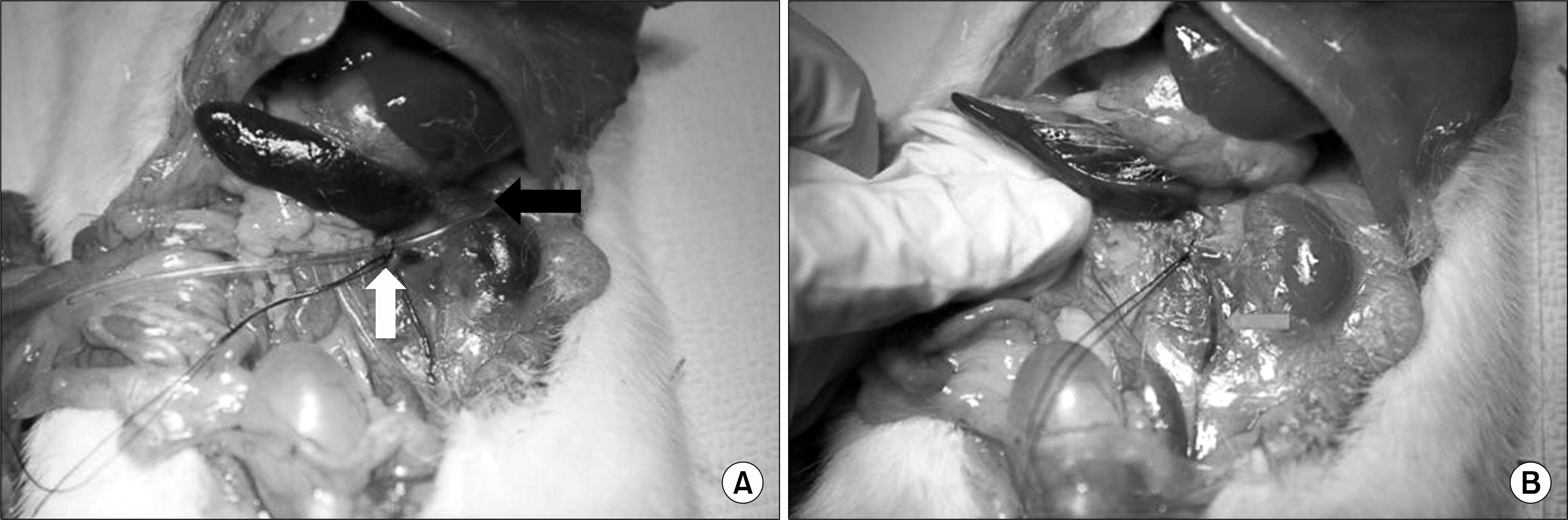
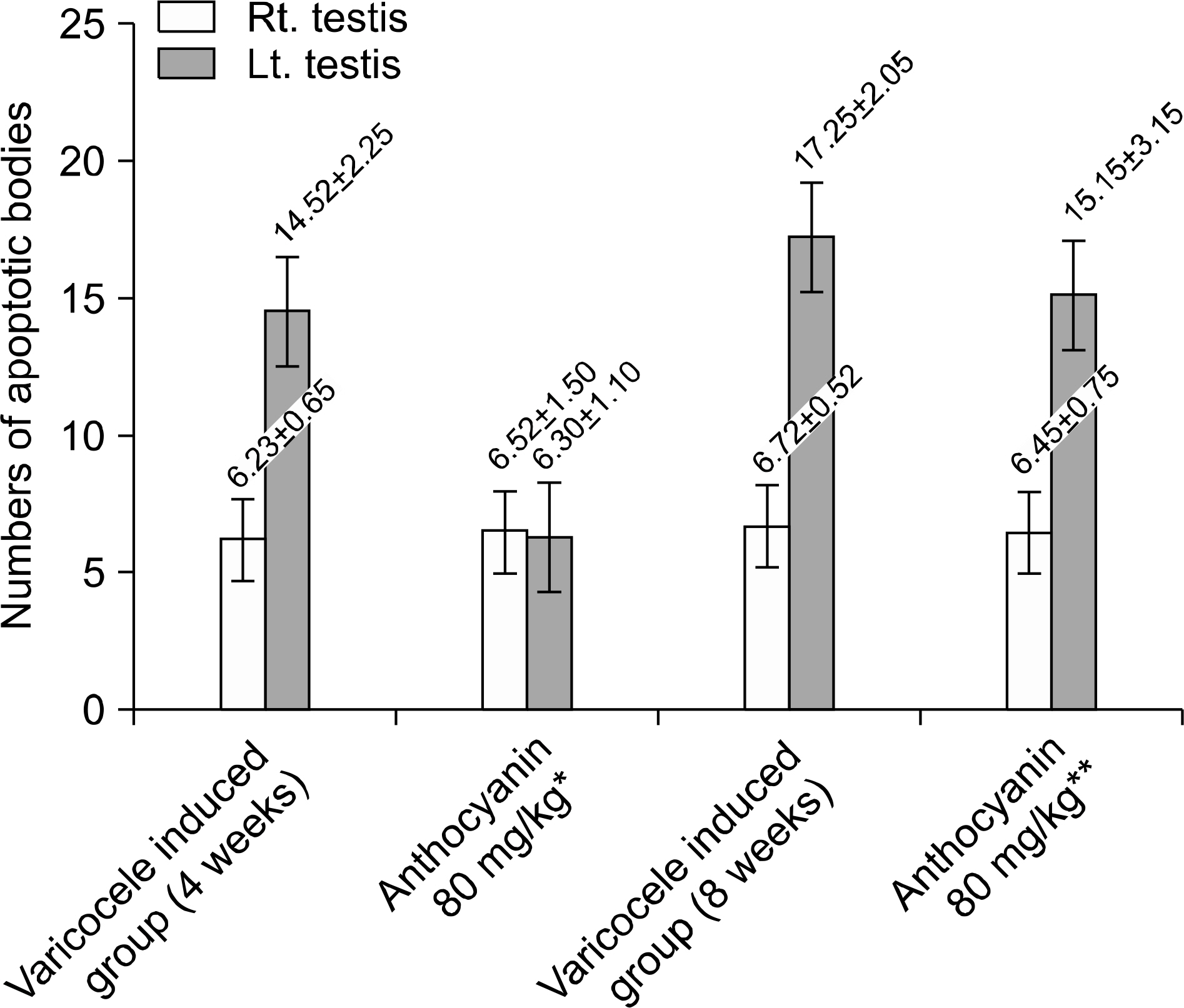
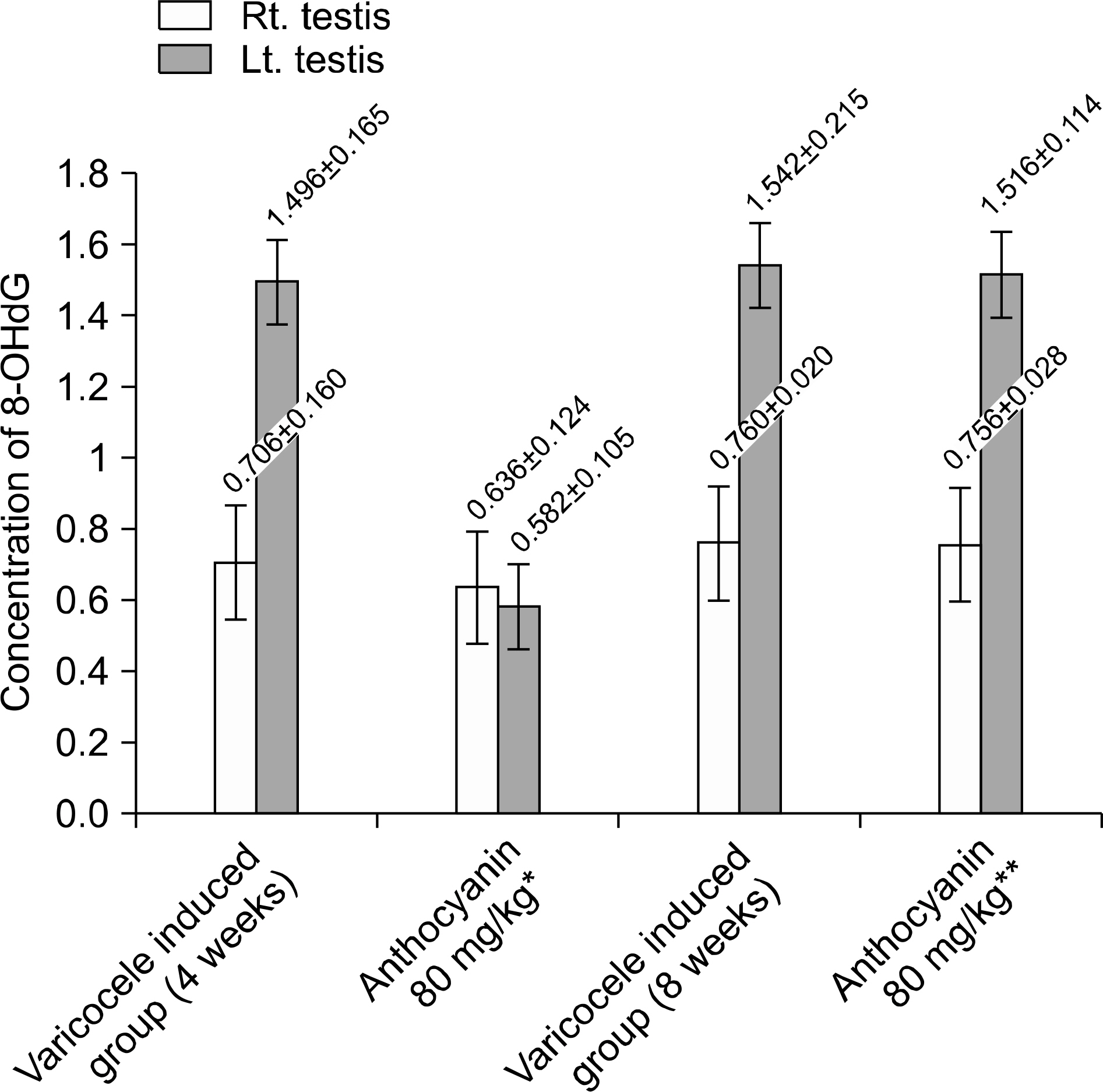
Twenty four male rats, induced varicocele by partial obstruction of left renal vein, were divided into four experimental groups: the group induced varicocele for four weeks without anthocyanin, the group received anthocyanin (80 mg/kg) right after varicocele induction, group induced varicocele for eight weeks without anthocyanin, and the group received anthocyanin (80 mg/kg) after four weeks observation following varicocele induction. After anthocyanin treatment, testes from the rats in all groups were removed, weighed, and subjected to histological examination. Apoptosis in the testes was measured by the TUNEL assay. And the oxidative stress was evaluated by measurement of 8-hydroxy-2'-deoxyguanosine (8-OHdG).
RESULTS
Induction of varicocele led to decreasing left testis weight, decreasing spermatogenic cell density significantly (p<0.05). Also it led to increasing apoptotic body counts and increasing concentration of 8-OHdG significantly (p<0.05). However administration of anthocyanin right after varicocele induction prevent this change meaningfully (p<0.05). In group received anthocyanin after four weeks observation following varicocele induction, interestingly, there was no significant difference in testis weight, spermatogenic cell density, apoptotic body count and concentration of 8-OHdG compared to group induced varicocele for eight weeks without anthocyanin administration.
CONCLUSIONS
These results suggest that anthocyanin is effective in decreasing the oxidative stress of testis in rat induced varicocele and may be effective in making a healthy sperm in patient of varicocele in early stage. However in patient under way in advanced stage, it is supposed that the anthocyanin cannot help having a protective effect from oxidative stress narrowly unless the condition of oxidative stress by varicocele is corrected. Further studies are needed to better understand the mechanisms and actions of anthocyanin and varicocele, and these studies may lead to the clinical application of anthocyanin in preventing male infertility by varicocele.
Keyword
MeSH Terms
Figure
Reference
-
1). Gorelick JI, Goldstein M. Loss of fertility in men with varicocele. Fertil Steril. 1993; 59:613–6.2). Naughton CK, Nangia AK, Agarwal A. Pathophysiology of varicoceles in male infertility. Hum Reprod Update. 2001; 7:473–81.3). Hendin BN, Kolettis PN, Sharma RK, Thomas AJ Jr, Agarwal A. Varicocele is associated with elevated spermatozoa reactive oxygen species production and diminished seminal plasma antioxidant capacity. J Urol. 1999; 161:1831–4.4). Fujisawa M, Hiramine C, Tanaka H, Okada H, Arakawa S, Kamidono S. Decrease in apoptosis of germ cells in the testes of infertile men with varicocele. World J Urol. 1999; 17:296–300.
Article5). Jang H, Ha US, Kim SJ, Yoon BI, Han DS, Yuk SM, et al. Anthocyanin extracted from black soybean reduces prostate weight and promotes apoptosis in the prostatic hyperplasia-induced rat mode. J Agric Food Chem. 2010; 58:12686–91.6). Saypol DC, Howards SS, Turner TT, Miller ED Jr. Influence of surgically induced varicocele in testicular blood flow, temperature, and histology in adult rats and dogs. J Clin Invest. 1981; 68:39–45.7). Goldstein M. Surgical management of male infertility and other scrotal disorders. Walsh PC, Retik AB, Vaughan ED, Wein AJ, editors. Campbell's urology. 7th ed.Philadelphia: Saunders;1998. p. 1384–71.8). Hagood PG, Mehan DJ, Worischeck JH, Andrus GH, Parra RO. Laparoscopic varicocelectomy: preliminary report of a new technique. J Urol. 1992; 147:73–6.
Article9). Ralph DJ, Timoney AG, Parker C, Pryor JP. Laparoscopic varicocele ligation. Br J Urol. 1993; 72:230–3.
Article10). Jarow JP, Assimos DG, Pittaway DE. Effectiveness of laparoscopic varicocelectomy. Urology. 1993; 42:544–7.
Article11). Turek PJ, Lipshultz LI. The varicocele controversies II: diagnosis and management. AUA Update Series. 1995; 14:114–9.12). Cohen MS, Plaine L, Brown IS. The role of internal spermatic vein plasma catecholamine determination in sub-fertile men with varicoceles. Fertil Steril. 1975; 26:1243–9.13). Goldstein M, Eid JF. Elevation of intratesticular and scrotal temperature in men with varicocele. J Urol. 1989; 142:743–5.14). Shin JW, Kim SW, Paick JS. Effect of varicocele treatments in adolescents: changes of semen parameters after early varicocelectomy. Korean J Urol. 2005; 46:481–6.15). Lyon RP, Marshall S, Scott MP. Varicocele in childhood and adolescence implication in adulthood infertility? Urology. 1982; 19:641–4.
Article16). Park SP, Nam HJ, Park HJ, Park NC. Correlation between duration of varicocele and testicular damage in an experimental rat model. Korean J Androl. 2009; 27:18–24.17). Sharma RK, Agarwal A. Role of reactive oxygen species in male infertility. Urology. 1996; 48:835–50.
Article18). Aitken RJ, Buckingham D, West K, Wu FC, Zikopoulos K, Richardson DW. Differential contribution of leukocytes and spermatozoa to the generation of reactive oxygen species in the ejaculates oligozoospermic patients and fertile donors. J Reprod Fertil. 1992; 94:451–62.19). de Lamirande E, Jiang H, Zini A, Kodama H, Gagnon C. Reactive oxygen species and sperm physiology. Rev Reprod. 1997; 2:48–54.
Article20). Aitken RJ, Clarkson JS. Cellular basis of defective sperm function and its association with the genesis of reactive oxygen species by human spermatozoa. J Reprod Fertil. 1987; 81:459–69.
Article21). Atessahin A, Karahan I, Türk G, Gür S, YIlmaz S, ÇeribasI AO. Protective role of lycopene on cisplatin-induced changes in sperm characteristics, testicular damage and oxidative stress in rats. Reprod Toxicol. 2006; 21:42–7.22). Ateşşahin A, Türk G, Karahan I, Yilmaz S, Ceribaşi AO, Bulmuş O. Lycopene prevents adriamycin-induced testicular toxicity in rats. Fertil Steril. 2006; 85:1216–22.23). Türk G, Ateşşahin A, Sönmez M, Yüce A, Ceribaşi AO. Lycopene protects against cyclosporine A-induced testicular toxicity in rats. Theriogenology. 2007; 67:778–85.
Article24). Sumner MD, Elliott-Eller M, Weidner G, Daubenmier JJ, Chew MH, Marlin R, et al. Effects of pomegranate juice consumption on myocardial perfusion in patients with coronary heart diseases. Am J Cardiol. 2005; 96:810–4.25). Rosenblat M, Hayek T, Aviram M. Anti-oxidative effects of pomegranate juice (PJ) consumption by diabetic patients on serum and on macrophages. Atherosclerosis. 2006; 187:363–71.
Article26). Sönmez M, Türk G, Yüce A. The effect of ascorbic acid supplementation on sperm quality, lipid peroxidation and testosterone levels of male Wistar rats. Theriogenology. 2005; 63:2063–72.
Article27). Sönmez M, Yüce A, Türk G. The protective effects of melatonin and vitamin E on antioxidant enzyme activities and epididymal sperm characteristics of homocysteine treated male rats. Reprod Toxicol. 2007; 23:226–31.
Article28). Wang SY, Jiao H. Scavenging capacity of berry crops on superoxide radicals, hydrogen peroxide, hydroxyl radicals, and singlet oxygen. J Agric Food Chem. 2000; 48:5677–84.
Article29). Shih PH, Yeh CT, Yen GC. Effects of anthocyanidin on the inhibition of proliferation and induction of apoptosis in human gastric adenocarcinoma cells. Food Chem Toxicol. 2005; 55:1557–66.
Article30). de Lamirande E, Jiang H, Zini A, Kodama H, Gagnon C. Reactive oxygen species and sperm physiology. Rev Reprod. 1997; 2:48–54.
Article31). Henkel R. The impact of oxidants on sperm functions. Andrologia. 2005; 37:205–6.32). Agarwal A, Allamaneni SS. Sperm DNA damage assessment: a test whose time has come. Fertil Steril. 2005; 84:850–3.
Article33). Saleh RA, Agarwal A, Sharma RK, Said TM, Sikka SC, Thomas AJ Jr. Evaluation of nuclear DNA damage in spermatozoa from infertile men with varicocele. Fertil Steril. 2003; 80:1431–6.
Article34). Agarwal A, Said TM. Oxidative stress, DNA damage and apoptosis in male infertility: a clinical approach. BJU Int. 2005; 95:503–7.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Testicular histology and volume according to the grade in adults with varicocele
- The Effects of Experimental Varicocele on Testis in Adolescent Rats
- Testis Biopsy in lnfertile Men with Azoospermia
- Cortisol and catecholamine in internal spermatic vein: are they toxic materials responsible for impairment of the spermatogenesis in varicocele?
- The Expression of P53 and Phosphorylation of H2AX in Germ Cells of Varicocele Rats