Korean J Androl.
2011 Apr;29(1):21-26. 10.5534/kja.2011.29.1.21.
The Effects of 5-alpha Reductase Inhibitor on Contr action of Erectile Tissue and Secretion of Seminal Fluid in Male Rabbits: Preliminary Study
- Affiliations
-
- 1Department of Urology, Seoul Medical Center, Seoul, Korea.
- 2Department of Urology, Chung-Ang University College of Medicine, Seoul, Korea. saeckim@unitel.co.kr
- 3Department of Urology, Bioculture, Cheonan, Korea.
- KMID: 2298622
- DOI: http://doi.org/10.5534/kja.2011.29.1.21
Abstract
- PURPOSE
Adverse sexual experiences such as erectile dysfunction (ED), loss of libido, and ejaculation disorders have been consistent side effects of 5-alpha reductase inhibitors (5ARI). The aim of this study was to evaluate the effects of 5ARI (finasteride) treatment on semen parameters and contraction of the corpus cavernosum and seminal vesicles in male rabbits.
MATERIALS AND METHODS
Adult male New Zealand White rabbits (n=10) were randomized into 2 groups: finasteride-treatment (5ARI) group and vehicle-treatment (control) group. The 5ARI group received daily oral finasteride (10 mg/day) by gavage for 4~6 weeks, and the control group received the same concentration of the vehicle. The semen volume and semen parameters between the 2 groups were compared; thereafter, contraction or relaxation responses of smooth muscle strips of the corpus cavernosum and seminal vesicles were observed in an organ bath.
RESULTS
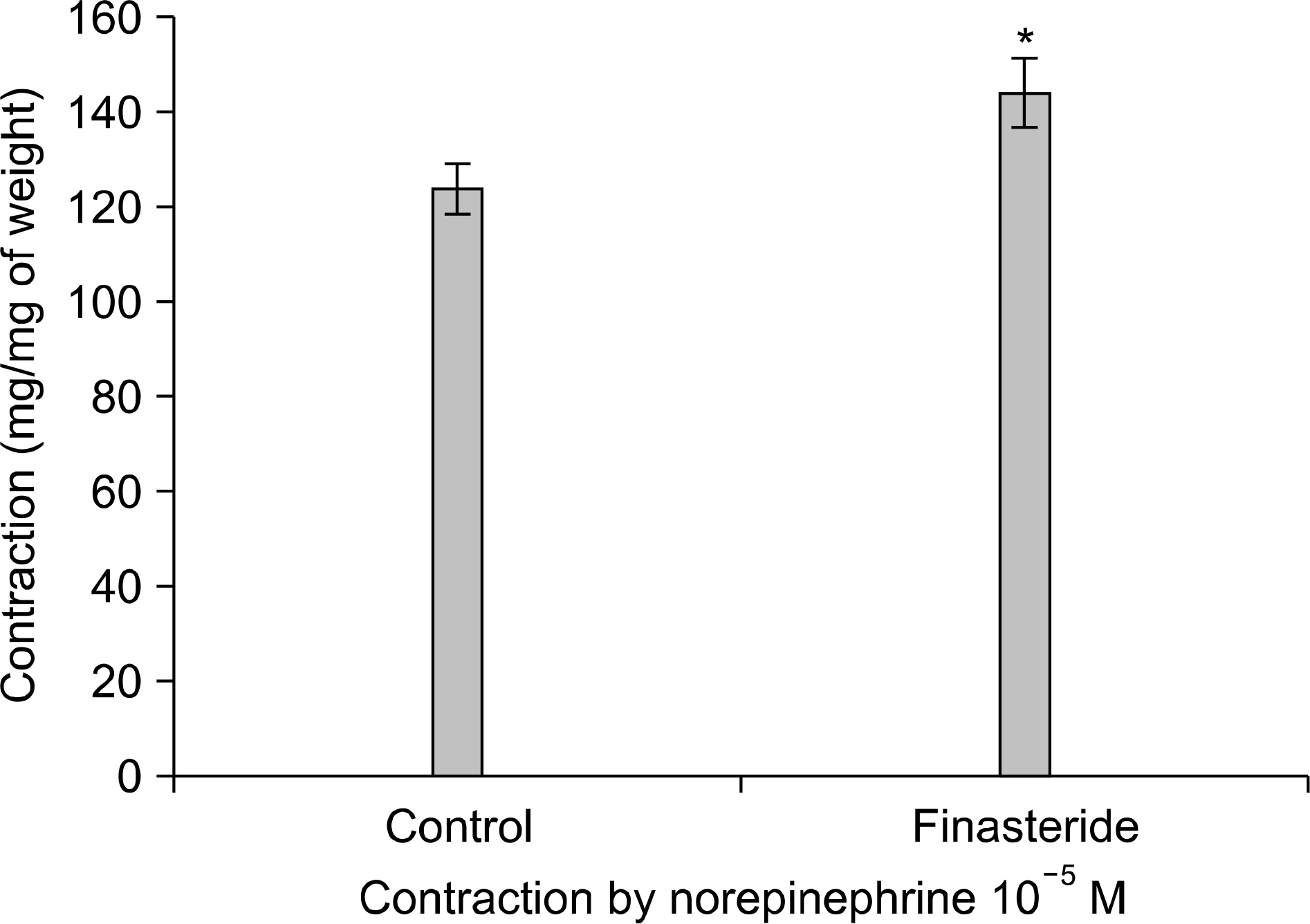
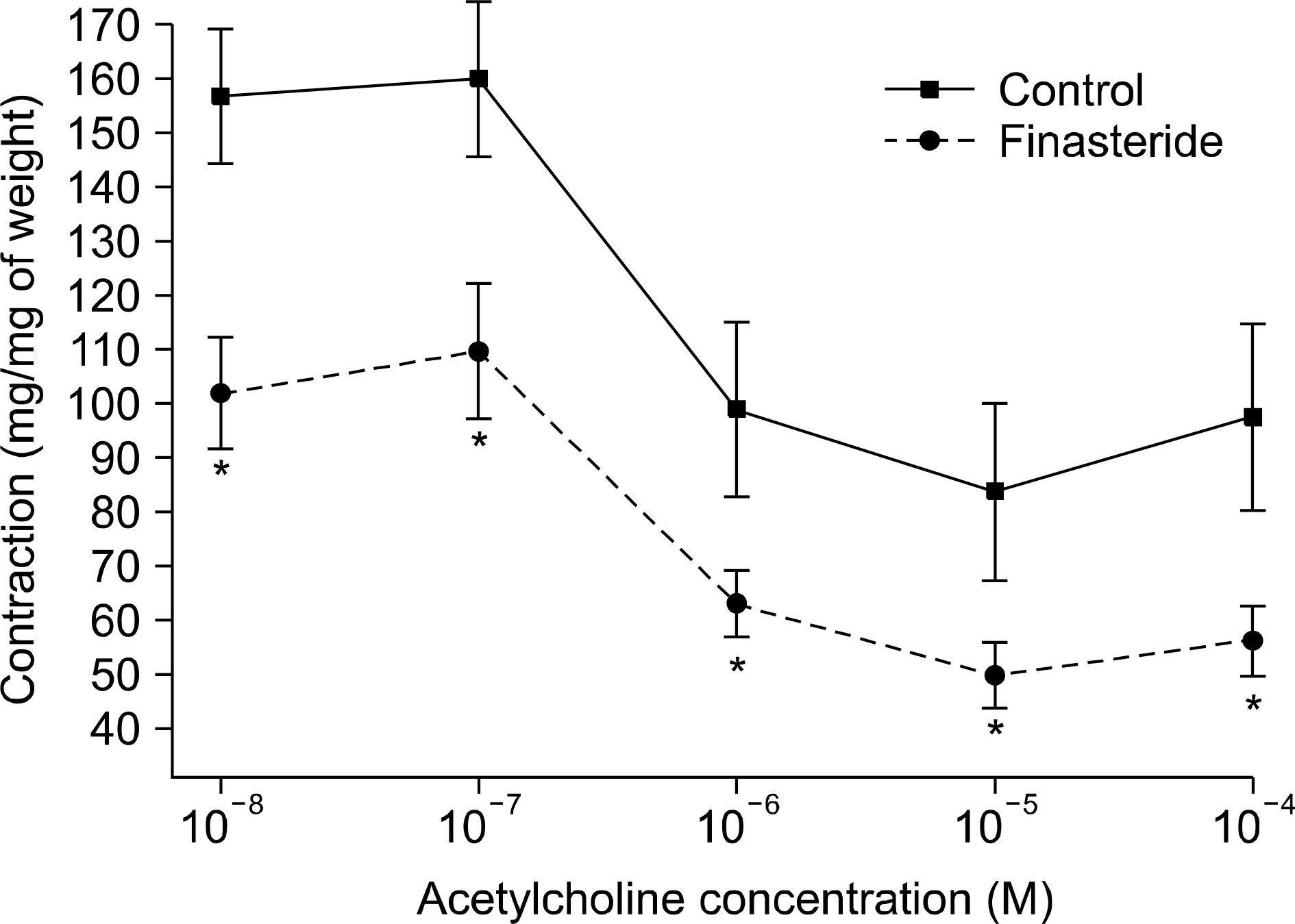
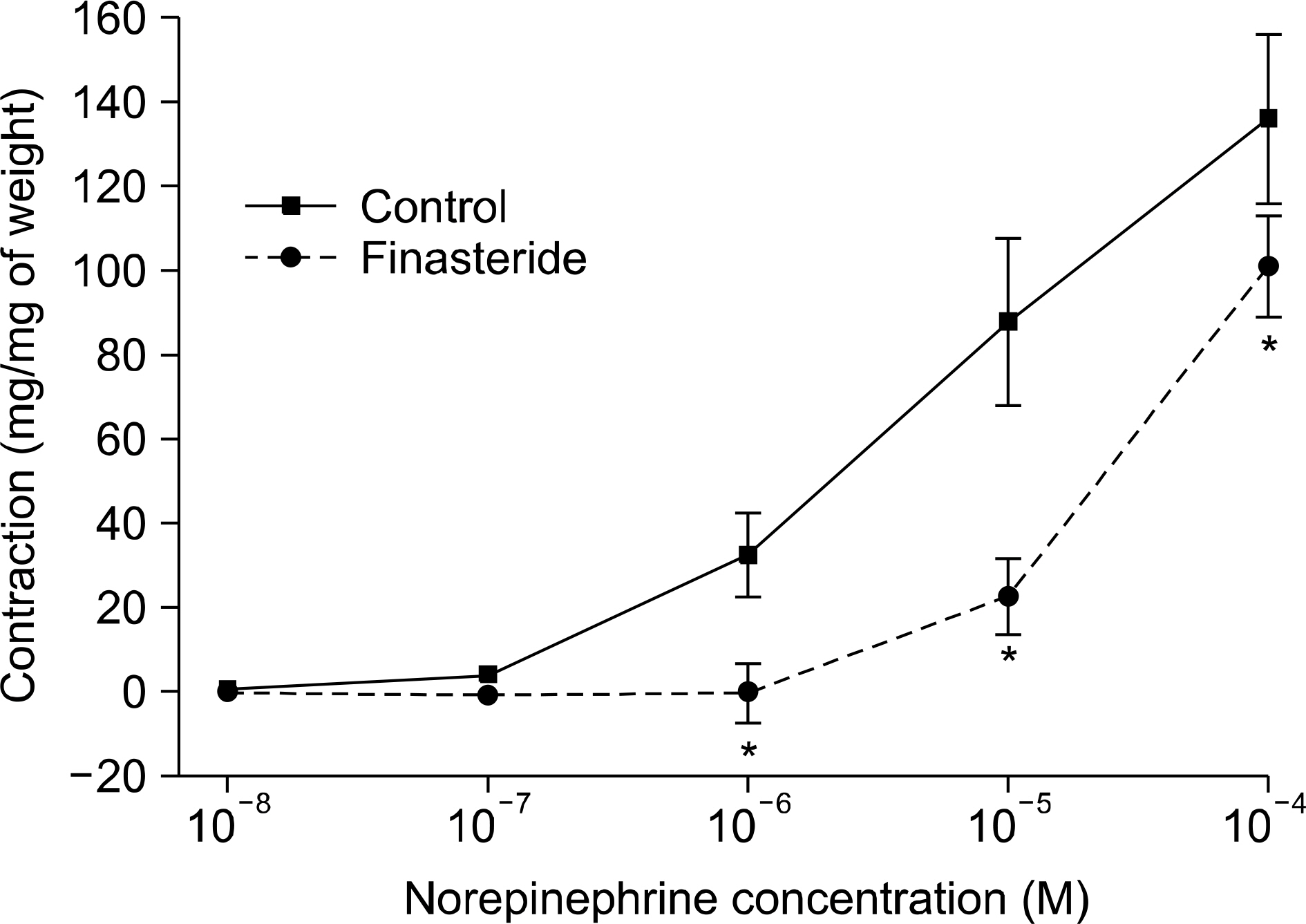
Semen magnesium (14.2 vs 5.1 mg/dl) and protein (2.2 vs 1.6 g/dl) concentrations were significantly lower in the 5ARI group than in the control group. The concentrations of other parameters such as electrolytes (Na/K/Cl), fructose, and citrate did not differ between the 2 groups. The contractile responses to norepinephrine (NE) significantly increased in the 5ARI group compared to the control group and the relaxation responses to acetylcholine (ACh) or sodium nitroprusside (SNP) also increased in the 5ARI group. The contractile responses of the seminal vesicular strips to NE significantly decreased in the 5ARI group compared with the control group.
CONCLUSIONS
The results suggest that finasteride may decrease contraction of seminal vesicle tissue and alter semen parameters. The effect of finasteride on erectile tissue was double-faced; enhancing both contraction and relaxation. Further study is needed in this respect.
MeSH Terms
-
5-alpha Reductase Inhibitors
Acetylcholine
Adult
Citric Acid
Contracts
Ejaculation
Electrolytes
Erectile Dysfunction
Finasteride
Fructose
Humans
Libido
Magnesium
Male
Muscle, Smooth
Nitroprusside
Norepinephrine
Oxidoreductases
Rabbits
Relaxation
Semen
Seminal Vesicles
5-alpha Reductase Inhibitors
Acetylcholine
Citric Acid
Electrolytes
Finasteride
Fructose
Magnesium
Nitroprusside
Norepinephrine
Oxidoreductases
Figure
Reference
-
1). Gormley GJ. Evaluation of men on finasteride. Semin Urol Oncol. 1996; 14:139–44.2). Boyle P, Gould AL, Roehrborn CG. Prostate volume predicts outcome of treatment of benign prostatic hyperplasia with finasteride: meta-analysis of randomizes clinical trials. Urology. 1996; 48:398–405.3). McConnell JD, Bruskewitz R, Walsh P, Andriole G, Lieber M, Holtgrewe HL, et al. The effect of finasteride on the risk of acute urinary retention and the need for surgical treatment among men with benign prostatic hyperplasia. Finasteride Long-Term Efficacy and Safety Study Group. New Engl J Med. 1998; 338:557–63.4). Lepor H, Williford WO, Barry MJ, Brawer MK, Dixon CM, Gormley G, et al. The efficacy of terazosin, finasteride, or both in benign prostatic hyperplasia. New Engl J Med. 1996; 335:553–9.
Article5). Marberger MJ. Longterm effects of finasteride in patients with benign prostatic hyperplasia: a double-blind, placebo-controlled, multicenter study. Urology. 1998; 51:677–86.
Article6). Mondaini N, Gontero P, Giubilei G, Lombardi G, Cai T, Gavazzi A, et al. Finasteride 5 mg and sexual side effects: how many of these are related to a nocebo phenomenon? J Sex Med. 2007; 4:1708–12.7). Gormley GJ, Stoner E, Rittmaster RS, Gregg H, Thompson DL, Lasseter KC, et al. Effects of finasteride (MK-906), a 5 alpha-reductase inhibitor, on circulating androgens in male volunteers. J Clin Endocrinol Metab. 1990; 70:1136–41.8). Cukierski MA, Sina JL, Prahalada S, Wise LD, Antonello JM, MacDonald JS, et al. Decreased fertility in male rats administered the 5 alpha-reductase inhibitor, finasteride, is due to deficits in copulatory plug formation. Reprod Toxicol. 1991; 5:353–62.9). Iguer-Ouada M, Verstegen JP. Effect of finasteride (Proscar MSD) on seminal composition, prostate function and fertility in male dogs. J Reprod Fertil Suppl. 1997; 51:139–49.10). Armbruster DA. Prostate-specific antigen: Biochemistry, analytical methods, and clinical application. Clin Chem. 1993; 39:181–95.
Article11). Malm J, Hellman J, Magnusson H, Laurell CB, Lilja H. Isolation and characterization of the major gel proteins in human semen, semenogelin I and semenogelin II. Eur J Biochem. 1996; 238:48–53.12). Veltri R, Rodriguez R. Molecular Biology, Endocrinology, and Physiology of the Prostate and Seminal Vesicles. Wein AJ, Kavoussi LR, Novick AC, Partin AW, Peters CA, editors. Campbell-Walsh urology. 9th ed.Philadelphia: Saunders;2007. p. 2677–726.13). Umeyama T, Ishikawa H, Takeshima H, Yoshii S, Koiso K. A comparative study of seminal trace elements in fertile and infertile men. Fertil Steril. 1986; 46:494–9.
Article14). Aumüller G, Riva A. Morphology and functions of the human seminal vesicle. Andrologia. 1992; 24:183–96.
Article15). Driessen B, Bultmann R, Goncalves J, Starke K. Opposite modulation of noradrenaline and ATP release in guinea-pig vas deferens through prejunctional beta-adrenoceptors: evidence for the beta 2 subtype. Naunyn Schmiedebergs Arch Pharmacol. 1996; 353:564–71.
Article16). Gladkova AI. The regulation of male sexual behavior by the sex hormones. Usp Fiziol Nauk. 1999; 30:97–105.17). Hong JH. Endocrinologic erectile dysfunction. In: Korean society for sexual medicine and andrology. Textbook of andrology. 2nd ed.Seoul: Koonja;2010. p. 239–46.18). Li Z, Wang YX, Zheng S, Xiang ZQ, Han YF. The effects of testosterone undecanoate on relaxation of rat corpus cavernosum smooth muscle in vitro. Zhonghua Nan Ke Xue. 2002; 8:130–3.19). Lugg JA, Rajfer J, Gonzalez-Cadavid NF. Dihydrotestosterone is the active androgen in the maintenance of nitric oxide-mediated penile erection in the rat. Endocrinology. 1995; 136:1495–501.
Article20). Park KH, Kim SW, Kim KD, Paick JS. Effects of androgens on the expression of nitric oxide synthase mRNAs in rat corpus cavernosum. BJU Int. 1999; 83:327–33.
Article21). Roehrborn CG, Lee M, Meehan A, Waldstreicher J. PLESS Study Group. Effects of finasteride on serum testosterone and body mass index in men with benign prostatic hyperplasia. Urology. 2003; 62:894–9.
Article22). Waldkirch E, Uckert S, Schultheiss D, Geismar U, Bruns C, Scheller F, et al. Non-genomic effects of androgens on isolated human vascular and nonvascular penile erectile tissue. BJU Int. 2008; 101:71–5.
Article23). Corradi LS, Goes RM, Carvalho HF, Taboga SR. Inhibition of 5-alpha-reductase activity induces stromal remodeling and smooth muscle de-differentiation in adult gerbil ventral prostate. Differentiation. 2004; 72:198–208.24). Traish AM, Goldstein I, Kim NN. Testosterone and erectile function: from basic research to a new clinical paradigm for managing men with androgen insufficiency and erectile dysfunction. Eur Urol. 2007; 52:54–70.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of 5 alpha-reductase Deficiency in Infancy
- Persistent Erectile Dysfunction after Discontinuation of 5-Alpha Reductase Inhibitor Therapy in Rats Depending on the Duration of Treatment
- SEMINAL FLUID AND SEMEN ANALYSIS
- Quantitative Determination of Immunoglobulin in Serum and Seminal Fluid of Patients with Prostatitis
- Cyst of the Seminal Vesicle