J Clin Neurol.
2008 Dec;4(4):139-147. 10.3988/jcn.2008.4.4.139.
Circulating Endothelial Progenitor Cells in Cerebrovascular Disease
- Affiliations
-
- 1Stroke & Stem Cell Laboratory, Clinical Research Institute, Stem Cell Research Center, Department of Neurology, Seoul National University Hospital, Program in Neuroscience, Neuroscience Research Institute of SNUMRC, Seoul National University College of Me
- KMID: 2287666
- DOI: http://doi.org/10.3988/jcn.2008.4.4.139
Abstract
- Stroke is associated with high disability and mortality burdens worldwide, but there are few effective and widely available therapies. There is therefore a need to develop treatments that promote the repair and regeneration of ischemic brain tissue. In this regard, a population of adult stem cells-called endothelial progenitor cells (EPCs)-has been identified in peripheral blood that could provide novel approaches in regenerative medicine for curing patients with acute ischemic stroke. There is accumulating evidence that EPCs can repair damaged endothelia and attenuate the development and progression of atherosclerosis. Also, EPCs can be recruited in response to acute ischemic events and participate in reparative vasculogenesis. Most studies related to EPCs have involved patients with cardiovascular diseases, and there is emerging evidence that EPCs represent a risk marker and a potential therapeutic agent in cerebrovascular disease. Here we review the characteristics and biology of EPCs in cerebrovascular disease and discuss the challenges that must be addressed to clarify the role and therapeutic applicability of EPCs in cerebrovascular disease.
Keyword
MeSH Terms
Figure
Cited by 2 articles
-
Levels of Soluble Receptor for Advanced Glycation End Products in Acute Ischemic Stroke without a Source of Cardioembolism
Hyun-Young Park, Kyeong Ho Yun, Do-Sim Park
J Clin Neurol. 2009;5(3):126-132. doi: 10.3988/jcn.2009.5.3.126.Retraction
J Clin Neurol. 2012;8(2):160-160. doi: 10.3988/jcn.2012.8.2.160.
Reference
-
1. Murray CJ, Lopez AD. Alternative projections of mortality and disability by cause 1990-2020: Global Burden of Disease Study. Lancet. 1997. 349:1498–1504.
Article2. Hurtado O, Pradillo JM, Alonso-Escolano D, Lorenzo P, Sobrino T, Castillo J, et al. Neurorepair versus neuroprotection in stroke. Cerebrovasc Dis. 2006. 21:Suppl 2. 54–63.
Article3. Asahara T, Murohara T, Sullivan A, Silver M, van der Zee R, Li T, et al. Isolation of putative progenitor endothelial cells for angiogenesis. Science. 1997. 275:964–967.
Article4. Hill JM, Zalos G, Halcox JP, Schenke WH, Waclawiw MA, Quyyumi AA, et al. Circulating endothelial progenitor cells, vascular function, and cardiovascular risk. N Engl J Med. 2003. 348:593–600.
Article5. Asahara T, Takahashi T, Masuda H, Kalka C, Chen D, Iwaguro H, et al. VEGF contributes to postnatal neovascularization by mobilizing bone marrow-derived endothelial progenitor cells. EMBO J. 1999. 18:3964–3972.
Article6. Murohara T, Ikeda H, Duan J, Shintani S, Sasaki K, Eguchi H, et al. Transplanted cord blood-derived endothelial precursor cells augment postnatal neovascularization. J Clin Invest. 2000. 105:1527–1536.
Article7. Takahashi T, Kalka C, Masuda H, Chen D, Silver M, Kearney M, et al. Ischemia- and cytokine-induced mobilization of bone marrow-derived endothelial progenitor cells for neovascularization. Nat Med. 1999. 5:434–438.
Article8. Vasa M, Fichtlscherer S, Aicher A, Adler K, Urbich C, Martin H, et al. Number and migratory activity of circulating endothelial progenitor cells inversely correlate with risk factors for coronary artery disease. Circ Res. 2001. 89:E1–E7.
Article9. Schatteman GC, Hanlon HD, Jiao C, Dodds SG, Christy BA. Blood-derived angioblasts accelerate blood-flow restoration in diabetic mice. J Clin Invest. 2000. 106:571–578.
Article10. Tepper OM, Galiano RD, Capla JM, Kalka C, Gagne PJ, Jacobowitz GR, et al. Human endothelial progenitor cells from type II diabetics exhibit impaired proliferation, adhesion, and incorporation into vascular structures. Circulation. 2002. 106:2781–2786.
Article11. Fadini GP, Miorin M, Facco M, Bonamico S, Baesso I, Grego F, et al. Circulating endothelial progenitor cells are reduced in peripheral vascular complications of type 2 diabetes mellitus. J Am Coll Cardiol. 2005. 45:1449–1457.
Article12. Schmidt-Lucke C, Rössig L, Fichtlscherer S, Vasa M, Britten M, Kämper U, et al. Reduced number of circulating endothelial progenitor cells predicts future cardiovascular events: proof of concept for the clinical importance of endogenous vascular repair. Circulation. 2005. 111:2981–2987.
Article13. Werner N, Kosiol S, Schiegl T, Ahlers P, Walenta K, Link A, et al. Circulating endothelial progenitor cells and cardiovascular outcomes. N Engl J Med. 2005. 353:999–1007.
Article14. Taguchi A, Matsuyama T, Moriwaki H, Hayashi T, Hayashida K, Nagatsuka K, et al. Circulating CD34-positive cells provide an index of cerebrovascular function. Circulation. 2004. 109:2972–2975.
Article15. Ghani U, Shuaib A, Salam A, Nasir A, Shuaib U, Jeerakathil T, et al. Endothelial progenitor cells during cerebrovascular disease. Stroke. 2005. 36:151–153.
Article16. Lau KK, Chan YH, Yiu KH, Li SW, Tam S, Lau CP, et al. Burden of carotid atherosclerosis in patients with stroke: relationships with circulating endothelial progenitor cells and hypertension. J Hum Hypertens. 2007. 21:445–451.
Article17. Sobrino T, Hurtado O, Moro MA, Rodríguez-Yáñez M, Castellanos M, Brea D, et al. The increase of circulating endothelial progenitor cells after acute ischemic stroke is associated with good outcome. Stroke. 2007. 38:2759–2764.
Article18. Yip HK, Chang LT, Chang WN, Lu CH, Liou CW, Lan MY, et al. Level and value of circulating endothelial progenitor cells in patients after acute ischemic stroke. Stroke. 2008. 39:69–74.
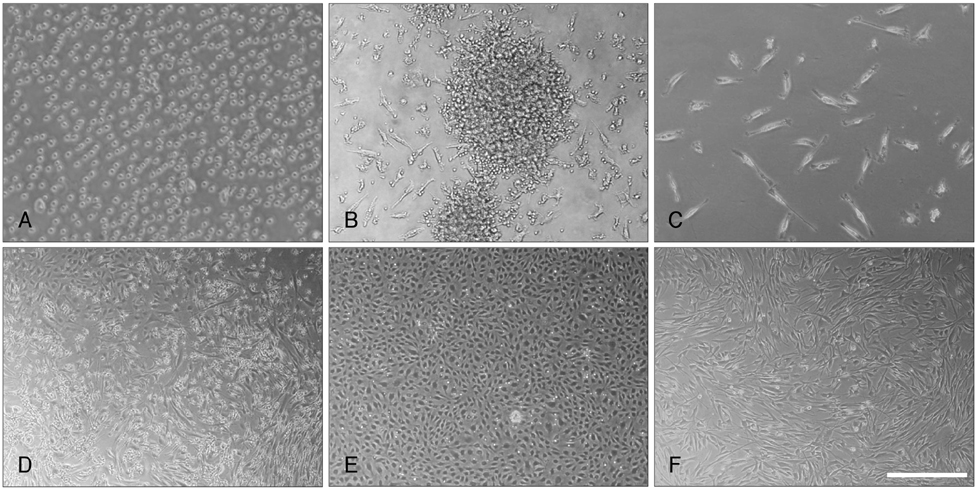
Article19. Jung KH, Chu K, Lee ST, Song EC, Sinn DI, Kim JM, et al. Identification of neuronal outgrowth cells from peripheral blood of stroke patients. Ann Neurol. 2008. 63:312–322.
Article20. Chu K, Jung KH, Lee ST, Park HK, Sinn DI, Kim JM, et al. Circulating endothelial progenitor cells as a new marker of endothelial dysfunction or repair in acute stroke. Stroke. 2008. 39:1441–1447.
Article21. Petersen BE, Bowen WC, Patrene KD, Mars WM, Sullivan AK, Murase N, et al. Bone marrow as a potential source of hepatic oval cells. Science. 1999. 284:1168–1170.
Article22. Orlic D, Kajstura J, Chimenti S, Jakoniuk I, Anderson SM, Li B, et al. Bone marrow cells regenerate infarcted myocardium. Nature. 2001. 410:701–705.
Article23. Brazelton TR, Rossi FM, Keshet GI, Blau HM. From marrow to brain: expression of neuronal phenotypes in adult mice. Science. 2000. 290:1775–1779.
Article24. Keller G. Marshak DR, Gardner RL, Gottlieb D, editors. The hemangioblast. Stem Cell Biology. 2001. Cold Spring Harbor, New York: Cold Spring Harbor Laboratory Press.25. Rafii S. Circulating endothelial precursors: mystery, reality, and promise. J Clin Invest. 2000. 105:17–19.
Article26. Abbott JD, Huang Y, Liu D, Hickey R, Krause DS, Giordano FJ. Stromal cell-derived factor-1alpha plays a critical role in stem cell recruitment to the heart after myocardial infarction but is not sufficient to induce homing in the absence of injury. Circulation. 2004. 110:3300–3305.
Article27. Asahara T, Masuda H, Takahashi T, Kalka C, Pastore C, Silver M, et al. Bone marrow origin of endothelial progenitor cells responsible for postnatal vasculogenesis in physiological and pathological neovascularization. Circ Res. 1999. 85:221–228.
Article28. Shintani S, Murohara T, Ikeda H, Ueno T, Honma T, Katoh A, et al. Mobilization of endothelial progenitor cells in patients with acute myocardial infarction. Circulation. 2001. 103:2776–2779.
Article29. Gill M, Dias S, Hattori K, Rivera ML, Hicklin D, Witte L, et al. Vascular trauma induces rapid but transient mobilization of VEGFR2(+)AC133(+) endothelial precursor cells. Circ Res. 2001. 88:167–174.
Article30. Khan SS, Solomon MA, McCoy JP Jr. Detection of circulating endothelial cells and endothelial progenitor cells by flow cytometry. Cytometry B Clin Cytom. 2005. 64:1–8.
Article31. Yin AH, Miraglia S, Zanjani ED, Almeida-Porada G, Ogawa M, Leary AG, et al. AC133, a novel marker for human hematopoietic stem and progenitor cells. Blood. 1997. 90:5002–5012.
Article32. Peichev M, Naiyer AJ, Pereira D, Zhu Z, Lane WJ, Williams M, et al. Expression of VEGFR-2 and AC133 by circulating human CD34+ cells identifies a population of functional endothelial precursors. Blood. 2000. 95:952–958.
Article33. Ingram DA, Caplice NM, Yoder MC. Unresolved questions, changing definitions, and novel paradigms for defining endothelial progenitor cells. Blood. 2005. 106:1525–1531.
Article34. George J, Shmilovich H, Deutsch V, Miller H, Keren G, Roth A. Comparative analysis of methods for assessment of circulating endothelial progenitor cells. Tissue Eng. 2006. 12:331–335.
Article35. Hur J, Yoon CH, Kim HS, Choi JH, Kang HJ, Hwang KK, et al. Characterization of two types of endothelial progenitor cells and their different contributions to neovasculogenesis. Arterioscler Thromb Vasc Biol. 2004. 24:288–293.
Article36. Lin Y, Weisdorf DJ, Solovey A, Hebbel RP. Origins of circulating endothelial cells and endothelial outgrowth from blood. J Clin Invest. 2000. 105:71–77.
Article37. Verma S, Anderson TJ. Fundamentals of endothelial function for the clinical cardiologist. Circulation. 2002. 105:546–549.
Article38. Perticone F, Ceravolo R, Pujia A, Ventura G, Iacopino S, Scozzafava A, et al. Prognostic significance of endothelial dysfunction in hypertensive patients. Circulation. 2001. 104:191–196.
Article39. Fadini GP, Coracina A, Baesso I, Agostini C, Tiengo A, Avogaro A, et al. Peripheral blood CD34+KDR+ endothelial progenitor cells are determinants of subclinical atherosclerosis in a middle-aged general population. Stroke. 2006. 37:2277–2282.
Article40. Taguchi A, Ohtani M, Soma T, Watanabe M, Kinosita N. Therapeutic angiogenesis by autologous bone-marrow transplantation in a general hospital setting. Eur J Vasc Endovasc Surg. 2003. 25:276–278.
Article41. Tateishi-Yuyama E, Matsubara H, Murohara T, Ikeda U, Shintani S, Masaki H, et al. Therapeutic angiogenesis for patients with limb ischaemia by autologous transplantation of bone-marrow cells: a pilot study and a randomised controlled trial. Lancet. 2002. 360:427–435.
Article42. Hamano K, Nishida M, Hirata K, Mikamo A, Li TS, Harada M, Miura T, et al. Local implantation of autologous bone marrow cells for therapeutic angiogenesis in patients with ischemic heart disease: clinical trial and preliminary results. Jpn Circ J. 2001. 65:845–847.
Article43. Beck H, Voswinckel R, Wagner S, Ziegelhoeffer T, Heil M, Helisch A, et al. Participation of bone marrow-derived cells in long-term repair processes after experimental stroke. J Cereb Blood Flow Metab. 2003. 23:709–717.
Article44. Yang GY, Pang L, Ge HL, Tan M, Ye W, Liu XH, et al. Attenuation of ischemia-induced mouse brain injury by SAG, a redox-inducible antioxidant protein. J Cereb Blood Flow Metab. 2001. 21:722–733.
Article45. Sairanen T, Carpén O, Karjalainen-Lindsberg ML, Paetau A, Turpeinen U, Kaste M, et al. Evolution of cerebral tumor necrosis factor-alpha production during human ischemic stroke. Stroke. 2001. 32:1750–1758.
Article46. Graham SH, Chen J. Programmed cell death in cerebral ischemia. J Cereb Blood Flow Metab. 2001. 21:99–109.
Article47. Kusuyama T, Omura T, Nishiya D, Enomoto S, Matsumoto R, Takeuchi K, et al. Effects of treatment for diabetes mellitus on circulating vascular progenitor cells. J Pharmacol Sci. 2006. 102:96–102.
Article48. Numaguchi Y, Sone T, Okumura K, Ishii M, Morita Y, Kubota R, et al. The impact of the capability of circulating progenitor cell to differentiate on myocardial salvage in patients with primary acute myocardial infarction. Circulation. 2006. 114:1 Suppl. I114–I119.
Article49. Döbert N, Britten M, Assmus B, Berner U, Menzel C, Lehmann R, et al. Transplantation of progenitor cells after reperfused acute myocardial infarction: evaluation of perfusion and myocardial viability with FDG-PET and thallium SPECT. Eur J Nucl Med Mol Imaging. 2004. 31:1146–1151.
Article50. Lev EI, Kleiman NS, Birnbaum Y, Harris D, Korbling M, Estrov Z. Circulating endothelial progenitor cells and coronary collaterals in patients with non-ST segment elevation myocardial infarction. J Vasc Res. 2005. 42:408–414.
Article51. Goolsby J, Marty MC, Heletz D, Chiappelli J, Taskko G, Yarnell D, et al. Hematopoietic progenitors express neural genes. Proc Natl Acad Sci U S A. 2003. 100:14926–14931.
Article52. Sanchez-Ramos JR, Song S, Kamath SG, Zigova T, Willing A, Cardozo-Pelaez F, et al. Expression of neural markers in human umbilical cord blood. Exp Neurol. 2001. 171:109–115.
Article53. Mezey E, Key S, Vogelsang G, Szalayova I, Lange GD, Crain B. Transplanted bone marrow generates new neurons in human brains. Proc Natl Acad Sci U S A. 2003. 100:1364–1369.
Article54. Carmeliet P. Mechanisms of angiogenesis and arteriogenesis. Nat Med. 2000. 6:389–395.
Article55. Yoon YS, Lee N, Scadova H. Myocardial regeneration with bone-marrow-derived stem cells. Biol Cell. 2005. 97:253–263.
Article56. Taguchi A, Soma T, Tanaka H, Kanda T, Nishimura H, Yoshikawa H, et al. Administration of CD34+ cells after stroke enhances neurogenesis via angiogenesis in a mouse model. J Clin Invest. 2004. 114:330–338.
Article57. Chen J, Sanberg PR, Li Y, Wang L, Lu M, Willing AE, et al. Intravenous administration of human umbilical cord blood reduces behavioral deficits after stroke in rats. Stroke. 2001. 32:2682–2688.
Article58. Zhang ZG, Zhang L, Jiang Q, Chopp M. Bone marrow-derived endothelial progenitor cells participate in cerebral neovascularization after focal cerebral ischemia in the adult mouse. Circ Res. 2002. 90:284–288.
Article59. Shyu WC, Lin SZ, Chiang MF, Su CY, Li H. Intracerebral peripheral blood stem cell (CD34+) implantation induces neuroplasticity by enhancing beta1 integrin-mediated angiogenesis in chronic stroke rats. J Neurosci. 2006. 26:3444–3453.
Article60. Ukai R, Honmou O, Harada K, Houkin K, Hamada H, Kocsis JD. Mesenchymal stem cells derived from peripheral blood protects against ischemia. J Neurotrauma. 2007. 24:508–520.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Circulating Vascular Progenitor Cells in Moyamoya Disease
- Journal of Clinical Neurology: Notice of Concern
- Circulating Endothelial Progenitor Cells and Vasculogenic Factors in Pterygium Pathogenesis
- Involvement of Circulating Endothelial Progenital Cells and Vasculogenic Factors in Diabetic Retinopathy
- Endothelial Progenitor Cells Correlated with Oxidative Stress after Mild Traumatic Brain Injury