J Clin Neurol.
2014 Apr;10(2):162-165. 10.3988/jcn.2014.10.2.162.
Ocular Dipping in Creutzfeldt-Jakob Disease
- Affiliations
-
- 1Department of Neurology, Hospital Universitario 12 de Octubre, Madrid, Spain. fsierra.hdoc@salud.madrid.org
- 2Instituto de Investigacion Hospital 12 de Octubre (i+12), Madrid, Spain.
- KMID: 2287535
- DOI: http://doi.org/10.3988/jcn.2014.10.2.162
Abstract
- BACKGROUND
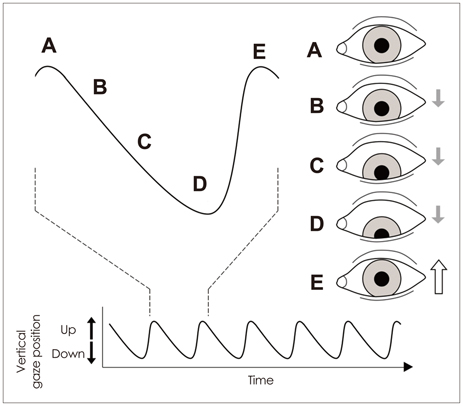
Ocular dipping (OD), or inverse ocular bobbing, consists of slow, spontaneous downward eye movements with rapid return to the primary position. It has been mainly reported following hypoxic-ischemic encephalopathy, but has also been described in association with other types of diffuse or multifocal encephalopathies and structural brainstem damage.
CASE REPORT
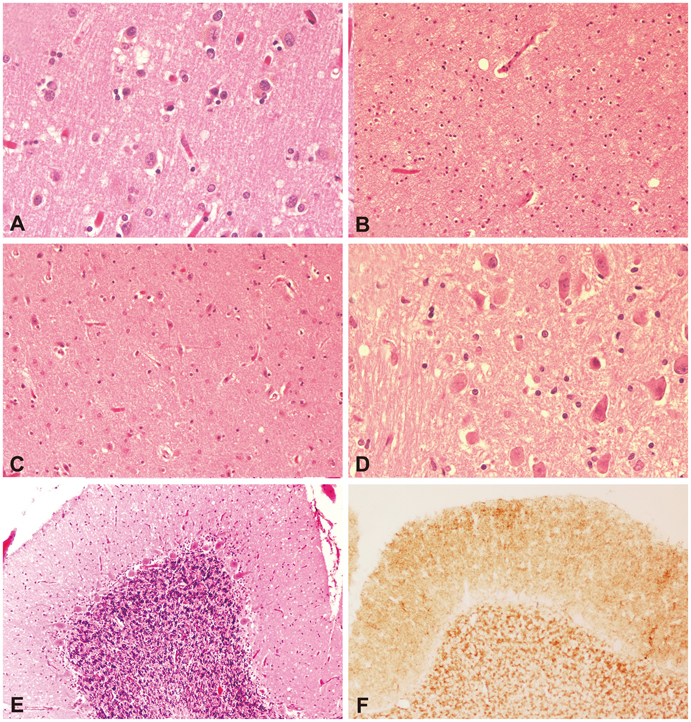
We report the case of a previously asymptomatic 66-year-old woman who presented with confusion, recent memory disturbances, and abnormal involuntary movements, followed by a coma. Abnormal spontaneous vertical eye movements consistent with OD developed from the fourth day after admission, and the patient died 20 days later. The pathological examination of the brain confirmed the diagnosis of Creutzfeldt-Jakob disease.
CONCLUSIONS
The precise location of damage causing OD is unknown. In contrast to ocular bobbing, OD has no localizing value itself, but structural brainstem damage is likely when it appears combined with other spontaneous vertical eye movements.
MeSH Terms
Figure
Reference
-
1. Wijdicks EFM. Neurologic complications of cardiac arrest. In : Wijdicks EFM, editor. Neurologic Complications of Critical Illness. 3rd ed. New York: Oxford University Press;2009. p. 132–153.2. Mehler MF. The clinical spectrum of ocular bobbing and ocular dipping. J Neurol Neurosurg Psychiatry. 1988; 51:725–727.
Article3. Knobler RL, Somasundaram M, Schutta HS. Inverse ocular bobbing. Ann Neurol. 1981; 9:194–197.
Article4. Leigh RJ, Zee DS. Diagnosis of central disorders of ocular motility. In : Leigh RJ, Zee DS, editors. The Neurology of Eye Movements. 4th ed. New York: Oxford University Press;2006. p. 598–718.5. Herishanu YO, Abarbanel JM, Frisher S, Farkash P, Berginer J, Amir-Schechter D. Spontaneous vertical eye movements associated with pontine lesions. Isr J Med Sci. 1991; 27:320–324.6. Donahue SP, Scott WE. Inverse ocular bobbing in infancy. J Pediatr Ophthalmol Strabismus. 1996; 33:189–190.
Article7. van Weerden TW, van Woerkom TC. Ocular dipping. Clin Neurol Neurosurg. 1982; 84:221–226.
Article8. Rosenberg ML. Spontaneous vertical eye movements in coma. Ann Neurol. 1986; 20:635–637.
Article9. Kaneko A, Iwasaki S, Hamaguchi K. [A case of pontine hemorrhage presenting with abnormal vertical ocular movements]. Rinsho Shinkeigaku. 1994; 34:1036–1041.10. Oh YM, Jeong SH, Kim JS. Ocular dipping and ping-pong gaze in hypoxic encephalopathy. Neurology. 2007; 68:222.
Article11. Jeong SH, Kim SY, Park SH, Kim JS. Ocular dipping in Creutzfeldt-Jakob disease. J Neuroophthalmol. 2008; 28:293–295.
Article12. Haraguchi T, Akaura K, Yabuki S. [Creutzfeldt-Jakob disease associated with ocular dipping--a case report]. Rinsho Shinkeigaku. 1998; 38:70–73.13. Ropper AH. Ocular dipping in anoxic coma. Arch Neurol. 1981; 38:297–299.
Article14. Shimazaki H, Morita M, Nakano I, Dalmau J. Inverse ocular bobbing in a patient with encephalitis associated with antibodies to the N-methyl-D-aspartate receptor. Arch Neurol. 2008; 65:1251.
Article15. Stark SR, Masucci EF, Kurtzke JF. Ocular dipping. Neurology. 1984; 34:391–393.
Article16. Toshniwal P, Yadava R, Goldbarg H. Presentation of pinealoblastoma with ocular dipping and deafness. J Clin Neuroophthalmol. 1986; 6:128–136.17. Koyano S, Nagumo K, Kanaya K, Niwa N, Iwabuchi S. [Periodic decerebrate spasm with ocular dipping, Cheyne-Stokes respiration and hypersympathetic activity]. Rinsho Shinkeigaku. 1996; 36:881–885.18. Kawahata N, Yamaguchi T, Satomi M. [Inverse ocular bobbing associated with cerebral embolism and diabetes insipidus--a case report]. Rinsho Shinkeigaku. 1989; 29:18–22.19. Luda E. Ocular dipping. Arch Neurol. 1982; 39:67.
Article20. Titer EM, Laureno R. Inverse/reverse ocular bobbing. Ann Neurol. 1988; 23:103–104.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A case of Creutzfeldt-Jakob disease
- New Variant Creutzfeldt-Jakob Disease
- A Case of Creutzfeldt-Jakob Disease Presenting Mainly with Abnormal Eye Movements
- Creutzfeldt-Jakob Disease Mimicking a Stroke as Initial Manifestation
- A Case of Probable Creutzfeldt-Jakob Disease with Coexistence of the Features of Hashimoto Encephalopathy