Diabetes Metab J.
2012 Jun;36(3):222-229. 10.4093/dmj.2012.36.3.222.
Influence of the Duration of Diabetes on the Outcome of a Diabetes Self-Management Education Program
- Affiliations
-
- 1Division of Endocrinology & Metabolism, Department of Internal Medicine, The Catholic University of Korea College of Medicine, Seoul, Korea. ybahn@catholic.ac.kr
- 2Department of Preventive Medicine, The Catholic University of Korea College of Medicine, Seoul, Korea.
- KMID: 2281403
- DOI: http://doi.org/10.4093/dmj.2012.36.3.222
Abstract
- BACKGROUND
Diabetes education and lifestyle modification are critical components in controlling blood glucose levels of people with type 2 diabetes. Until now, available data on the effectiveness of education with respect to the duration of diabetes are limited. We investigated whether adherence to lifestyle behavior modification prompted by diabetes education was influenced by the duration of diabetes.
METHODS
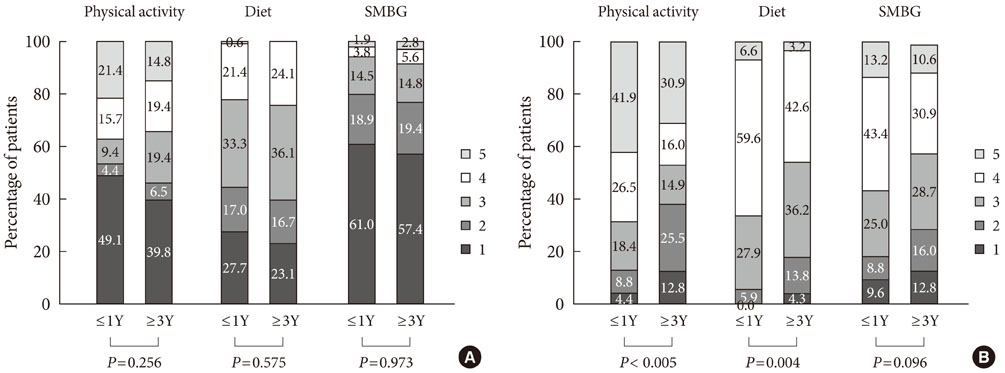
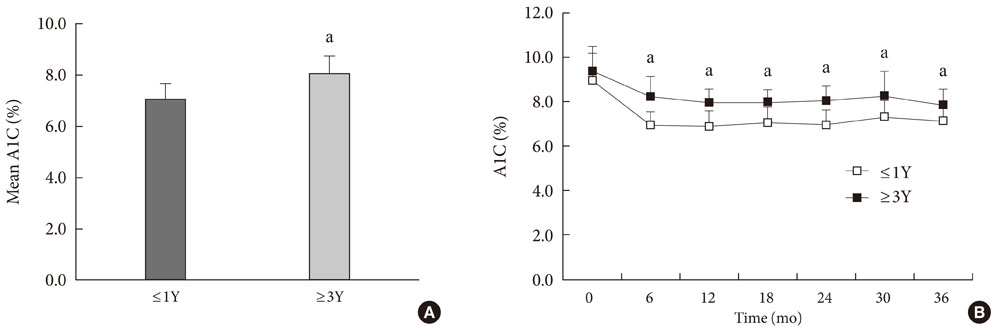
Two hundred and twenty-five people with type 2 diabetes were recruited for an intensive, collaborative, group-based diabetes education program with annual reinforcement. We divided the patients into two groups based on the duration of their diabetes prior to the education program (< or =1 year [< or =1Y] vs. > or =3 years [> or =3Y]). Dietary habits, physical activity, and the frequency of blood glucose self-monitoring were evaluated with a questionnaire prior to education and at the follow-up endpoint.
RESULTS
The mean follow-up period was 32.2 months. The mean hemoglobin A1c (A1C) value was significantly lower in the < or =1Y group. Self-care behaviors, measured by scores for dietary habits (P=0.004) and physical activity (P<0.001), were higher at the endpoint in the < or =1Y group than in the > or =3Y group. Logistic regression analysis revealed that a longer diabetes duration before education was significantly associated with mean A1C levels greater than or equal to 7.0% (53 mmol/mol).
CONCLUSION
Diabetes duration influenced the effectiveness of diabetes education on lifestyle behavior modification and glycemic control. More-intense, regular, and sustained reinforcement with encouragement may be required for individuals with longstanding type 2 diabetes.
MeSH Terms
Figure
Cited by 2 articles
-
Moderate diet-induced weight loss is associated with improved insulin sensitivity in middle-aged healthy obese Korean women
Hye-Ok Lee, Jung-Eun Yim, Young-Seol Kim, Ryowon Choue
Nutr Res Pract. 2014;8(4):469-475. doi: 10.4162/nrp.2014.8.4.469.The Well-Being and Treatment Satisfaction of Diabetic Patients in an Outpatient Setting at a General Hospital in Korea
Hwa-Sun Park, Sin Na Lee, Min Young Baek, Seung Hee Yu, Young Sil Eom, Sihoon Lee, Ki Young Lee, Yeun Sun Kim, Byung Joon Kim, Kwang Won Kim, Ie Byung Park
J Korean Diabetes. 2016;17(2):123-133. doi: 10.4093/jkd.2016.17.2.123.
Reference
-
1. American Diabetes Association. Standards of medical care in diabetes: 2011. Diabetes Care. 2011. 34:Suppl 1. S11–S61.2. Assal JP, Muhlhauser I, Pernet A, Gfeller R, Jorgens V, Berger M. Patient education as the basis for diabetes care in clinical practice and research. Diabetologia. 1985. 28:602–613.3. Norris SL, Lau J, Smith SJ, Schmid CH, Engelgau MM. Self-management education for adults with type 2 diabetes: a meta-analysis of the effect on glycemic control. Diabetes Care. 2002. 25:1159–1171.4. Polonsky WH, Earles J, Smith S, Pease DJ, Macmillan M, Christensen R, Taylor T, Dickert J, Jackson RA. Integrating medical management with diabetes self-management training: a randomized control trial of the Diabetes Outpatient Intensive Treatment program. Diabetes Care. 2003. 26:3048–3053.5. Gillett M, Dallosso HM, Dixon S, Brennan A, Carey ME, Campbell MJ, Heller S, Khunti K, Skinner TC, Davies MJ. Delivering the diabetes education and self management for ongoing and newly diagnosed (DESMOND) programme for people with newly diagnosed type 2 diabetes: cost effectiveness analysis. BMJ. 2010. 341:c4093.6. Rubin RR, Peyrot M, Saudek CD. Effect of diabetes education on self-care, metabolic control, and emotional well-being. Diabetes Care. 1989. 12:673–679.7. Tankova T, Dakovska G, Koev D. Education and quality of life in diabetic patients. Patient Educ Couns. 2004. 53:285–290.8. Ko GT, Li JK, Kan EC, Lo MK. Effects of a structured health education programme by a diabetic education nurse on cardiovascular risk factors in Chinese type 2 diabetic patients: a 1-year prospective randomized study. Diabet Med. 2004. 21:1274–1279.9. Clark CM Jr, Fradkin JE, Hiss RG, Lorenz RA, Vinicor F, Warren-Boulton E. The National Diabetes Education Program, changing the way diabetes is treated: comprehensive diabetes care. Diabetes Care. 2001. 24:617–618.10. Norris SL, Engelgau MM, Narayan KM. Effectiveness of self-management training in type 2 diabetes: a systematic review of randomized controlled trials. Diabetes Care. 2001. 24:561–587.11. Look AHEAD Research Group. Wing RR. Long-term effects of a lifestyle intervention on weight and cardiovascular risk factors in individuals with type 2 diabetes mellitus: four-year results of the Look AHEAD trial. Arch Intern Med. 2010. 170:1566–1575.12. Ko SH, Song KH, Kim SR, Lee JM, Kim JS, Shin JH, Cho YK, Park YM, Jeong JH, Yoon KH, Cha BY, Son HY, Ahn YB. Long-term effects of a structured intensive diabetes education programme (SIDEP) in patients with type 2 diabetes mellitus: a 4-year follow-up study. Diabet Med. 2007. 24:55–62.13. Charman D. Burnout and diabetes: reflections from working with educators and patients. J Clin Psychol. 2000. 56:607–617.14. Muhlhauser I, Bruckner I, Berger M, Cheta D, Jorgens V, Ionescu-Tirgoviste C, Scholz V, Mincu I. Evaluation of an intensified insulin treatment and teaching programme as routine management of type 1 (insulin-dependent) diabetes. The Bucharest-Dusseldorf Study. Diabetologia. 1987. 30:681–690.15. The Diabetes Prevention Program Research Group. The Diabetes Prevention Program. Design and methods for a clinical trial in the prevention of type 2 diabetes. Diabetes Care. 1999. 22:623–634.16. Cronin FJ, Shaw AM, Krebs-Smith SM, Marsland PM, Light L. Developing a food guidance system to implement the dietary guidelines. J Nutr Educ. 1987. 19:281–302.17. Mensing C, Boucher J, Cypress M, Weinger K, Mulcahy K, Barta P, Hosey G, Kopher W, Lasichak A, Lamb B, Mangan M, Norman J, Tanja J, Yauk L, Wisdom K, Adams C. National standards for diabetes self-management education. Task force to review and revise the national standards for diabetes self-management education programs. Diabetes Care. 2000. 23:682–689.18. Franciosi M, Pellegrini F, De Berardis G, Belfiglio M, Cavaliere D, Di Nardo B, Greenfield S, Kaplan SH, Sacco M, Tognoni G, Valentini M, Nicolucci A. QuED Study Group. The impact of blood glucose self-monitoring on metabolic control and quality of life in type 2 diabetic patients: an urgent need for better educational strategies. Diabetes Care. 2001. 24:1870–1877.19. Funnell MM, Brown TL, Childs BP, Haas LB, Hosey GM, Jensen B, Maryniuk M, Peyrot M, Piette JD, Reader D, Siminerio LM, Weinger K, Weiss MA. National standards for diabetes self-management education. Diabetes Care. 2010. 33:Suppl 1. S89–S96.20. Peterson U, Demerouti E, Bergstrom G, Samuelsson M, Asberg M, Nygren A. Burnout and physical and mental health among Swedish healthcare workers. J Adv Nurs. 2008. 62:84–95.21. Asberg M, Nygren A, Leopardi R, Rylander G, Peterson U, Wilczek L, Kallmen H, Ekstedt M, Akerstedt T, Lekander M, Ekman R. Novel biochemical markers of psychosocial stress in women. PLoS One. 2009. 4:e3590.22. Lindstrom C, Aman J, Norberg AL. Increased prevalence of burnout symptoms in parents of chronically ill children. Acta Paediatr. 2010. 99:427–432.23. Eom YS, Park HS, Kim SH, Yang SM, Nam MS, Lee HW, Lee KY, Lee S, Kim YS, Park IB. Evaluation of stress in Korean patients with diabetes mellitus using the Problem Areas in Diabetes-Korea questionnaire. Diabetes Metab J. 2011. 35:182–187.24. Weinger K, Beverly EA, Lee Y, Sitnokov L, Ganda OP, Caballero AE. The effect of a structured behavioral intervention on poorly controlled diabetes: a randomized controlled trial. Arch Intern Med. 2011. 171:1990–1999.25. Song MS, Song KH, Ko SH, Ahn YB, Kim JS, Shin JH, Cho YK, Yoon KH, Cha BY, Son HY, Lee DH. The long-term effect of a structured diabetes education program for uncontrolled type 2 diabetes mellitus patients: a 4-year follow-up. J Korean Diabetes Assoc. 2005. 29:140–150.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Role of Diabetes Educators and Effectiveness of Diabetes Education
- Developing Strategies for Diabetes Education Program
- Medical Insurance Coverage for Diabetes Education
- Research Review: Effective of Self-Management Education in Diabetes Patients
- Special Considerations in Diabetes Self-Management Education for Older Adults with Diabetes: A Study Focusing on Community Senior Welfare Centers