Clin Nutr Res.
2012 Jul;1(1):94-98. 10.7762/cnr.2012.1.1.94.
A Case of Protein Supplement Effect in Protein-Losing Enteropathy
- Affiliations
-
- 1Department of Dietetics, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul 135-710, Korea.
- 2Division of Gastroenterology, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul 135-710, Korea. do.chang@samsung.com
- KMID: 2279757
- DOI: http://doi.org/10.7762/cnr.2012.1.1.94
Abstract
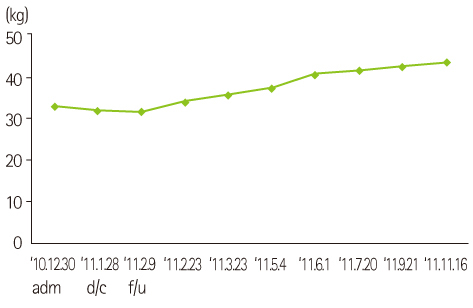
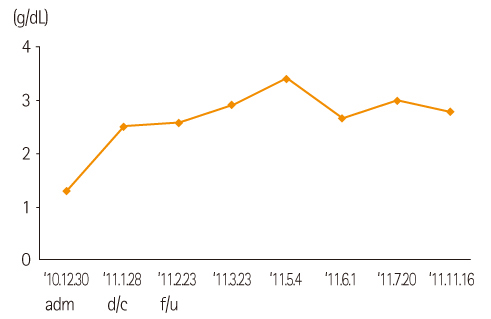
- The objective of this article is to report improvement of nutritional status by protein supplements in the patient with protein-losing enteropathy. The patient was a female whose age was 25 and underwent medical treatment of Crohn's disease, an inflammatory bowl disease, after diagnosis of cryptogenic multifocal ulcerous enteritis. The weight was 33.3 kg (68% of IBW) in the severe underweight and suffered from ascites and subcutaneous edema with hypoalbuminemia (1.3 g/dL) at the time of hospitalization. The patient consumed food restrictively due to abdominal discomfort. Despite various attempts of oral feeding, the levels of calorie and protein intake fell into 40-50% of the required amount, which was 800-900 kcal/d (24-27 kcal/kg/d) for calorie and 34 g/d (1 g/kg/d) for protein. It was planned to supplement the patient with caloric supplementation (40-50 kcal/kg) and protein supplementation (2.5 g/kg) to increase body weight and improve hypoproteinemia. It was also planned to increase the level of protein intake slowly to target 55 g/d in about 2 weeks starting from 10 g/d and monitored kidney load with high protein supplementation. The weight loss was 1.0 kg when the patient was discharged from the hospital (hospitalization periods of 4 weeks), however, serum albumin was improved from 1.3 g/dL to 2.5 g/dL and there was no abdominal discomfort. She kept supplement of protein at 55 g/d for 5 months after the discharge from the hospital and kept it at 35 g/d for about 2 months and then 25 g/d. The body weight increased gradually from 32.3 kg (65% of IBW) to 44.0 kg (89% of IBW) by 36% for the period of F/u and serum albumin was kept above 2.8 g/dL without intravenous injection of albumin. The performance status was improved from 4 points of 'very tired' to 2 points of 'a little tired' out of 5-point scale measurement and the use of diuretic stopped from the time of 4th month after the discharge from the hospital owing to improvement in edema and ascites. During this period, the results of blood test such as BUN, Cr, and electrolytes were within the normal range. In conclusion, hypoproteinemia and weight loss were improved by increasing protein intake through utilization of protein supplements in protein-losing enteropathy.
Keyword
MeSH Terms
-
Ascites
Body Weight
Crohn Disease
Diagnosis
Edema
Electrolytes
Enteritis
Female
Hematologic Tests
Hospitalization
Humans
Hypoalbuminemia
Hypoproteinemia
Inflammatory Bowel Diseases
Injections, Intravenous
Kidney
Nutritional Status
Protein-Losing Enteropathies*
Reference Values
Serum Albumin
Thinness
Ulcer
Weight Loss
Electrolytes
Serum Albumin
Figure
Reference
-
1. Han SH, Lee OY, Eun CS, Roh BJ, Sohn W, Baeg SS, Yoon BC, Choi HS. A case of protein-losing enteropathy associated with small bowel villous atrophy. Korean J Gastroenterol. 2007. 49:31–36.2. Escott-Stump S. Nutrition and diagnosis-related care. 2002. 5th ed. Philadelphia: Lippincott Williams & Wilkins.3. Lee HL, Han DS, Kim JB, Jeon YC, Sohn JH, Hahm JS. Successful treatment of protein-losing enteropathy induced by intestinal lymphangiectasia in a liver cirrhosis patient with octreotide: a case report. J Korean Med Sci. 2004. 19:466–469.
Article4. Ferrante M, Penninckx F, De Hertogh G, Geboes K, D'Hoore A, Noman M, Vermeire S, Rutgeerts P, Van Assche G. Protein-losing enteropathy in Crohn’s disease. Acta Gastroenterol Belg. 2006. 69:384–389.5. Ungaro R, Babyatsky MW, Zhu H, Freed JS. Protein-losing enteropathy in ulcerative colitis. Case Rep Gastroenterol. 2012. 6:177–182.
Article6. Baert D, Wulfrank D, Burvenich P, Lagae J. Lymph loss in the bowel and severe nutritional disturbances in Crohn's disease. J Clin Gastroenterol. 1999. 29:277–279.
Article7. Valentini L, Schaper L, Buning C, Hengstermann S, Koernicke T, Tillinger W, Guglielmi FW, Norman K, Buhner S, Ockenga J, Pirlich M, Lochs H. Malnutrition and impaired muscle strength in patients with Crohn's disease and ulcerative colitis in remission. Nutrition. 2008. 24:694–702.
Article8. Umar SB, DiBaise JK. Protein-losing enteropathy: case illustrations and clinical review. Am J Gastroenterol. 2010. 105:43–49.
Article9. Braamskamp MJ, Dolman KM, Tabbers MM. Clinical practice. Protein-losing enteropathy in children. Eur J Pediatr. 2010. 169:1179–1185.10. Nelms MN. Nutrition therapy and pathophysiology. 2002. 2nd ed. Belmont: Wadsworth.11. Ballinger AB, Farthing MJ. Octreotide in the treatment of intestinal lymphangiectasia. Eur J Gastroenterol Hepatol. 1998. 10:699–702.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A case of systemic lupus erythematosus with chylothorax, chronic interstitial cystitis and protein-losing enteropathy
- Primary protein-losing enteropathy : report of a case (idiopathic intestinal lymphangiectasia)
- A Case of Primary Sjogren's Syndrome with Protein-losing Enteropathy
- A Case of Idiopathic Protein-losing Enteropathy
- A case of constrictive pericarditis presenting with protein-losing enteropathy