Epidural Steroid Injection in Korean Pain Physicians: A National Survey
- Affiliations
-
- 1Department of Anesthesiology and Pain Medicine, Seoul National University Hospital, Seoul, Korea. jymoon0901@gmail.com
- 2Department of Anesthesiology and Pain Medicine, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea.
- 3Department of Anesthesiology and Pain Medicine, Zein Pain Treatment Clinic, Seoul, Korea.
- 4Department of Anesthesiology & Pain Medicine, Chung Ang University Hospital, Seoul, Korea.
- 5Department of Anesthesiology & Pain Medicine, Konkuk University Medical Center, Seoul, Korea.
- 6Department of Anesthesiology & Pain Medicine, Wonkwang University School of Medicine, Iksan, Korea.
- 7Department of Anesthesiology & Pain Medicine, Soonchunhyang University Seoul Hospital, Seoul, Korea.
- KMID: 2278200
- DOI: http://doi.org/10.3344/kjp.2014.27.1.35
Abstract
- BACKGROUND
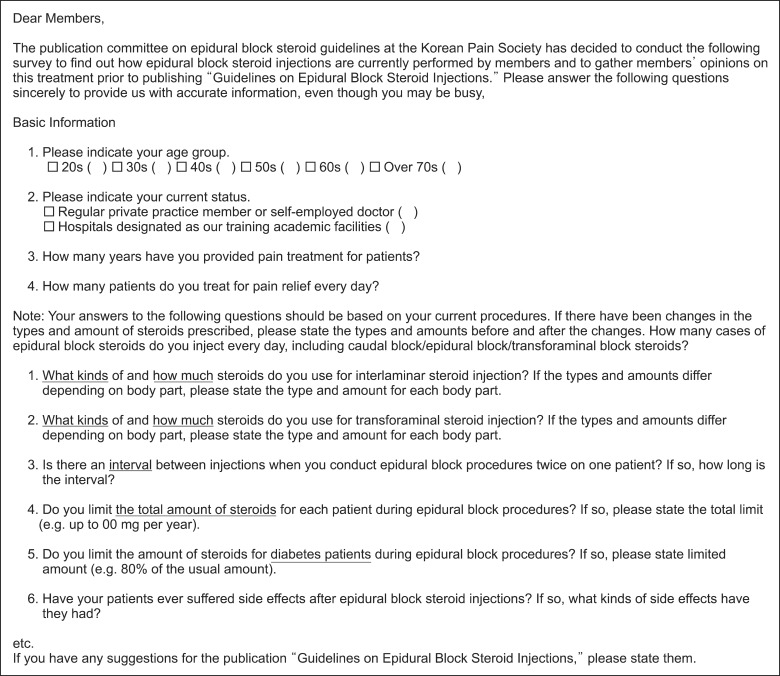
Epidural steroid injection (ESI) is one of the most common procedures for patients presenting low back pain and radiculopathy. However, there is no clear consensus on what constitutes appropriate steroid use for ESIs. To investigate optimal steroid injection methods for ESIs, surveys were sent to all academic pain centers and selected private practices in Korea via e-mail.
METHODS
Among 173 pain centers which requested the public health insurance reimbursements for their ESIs and were enrolled in the Korean Pain Society, 122 completed questionnaires were returned, for a rate of 70.5%; also returned were surveys from 39 academic programs and 85 private practices with response rates of 83.0% and 65.9%, respectively.
RESULTS
More than half (55%) of Korean pain physicians used dexamethasone for ESIs. The minimum interval of subsequent ESIs at the academic institutions (3.1 weeks) and the private practices (2.1 weeks) were statistically different (P = 0.01).
CONCLUSIONS
Although there was a wide range of variation, there were no significant differences between the academic institutions and the private practices in terms of the types and single doses of steroids for ESIs, the annual dose of steroids, or the limitations of doses in the event of diabetes, with the exception of the minimum interval before the subsequent ESI.
Keyword
MeSH Terms
Figure
Cited by 6 articles
-
Cervical Meningomyelitis After Lumbar Epidural Steroid Injection
Yujin Lee, Joon-Sung Kim, Ji Yeon Kim
Ann Rehabil Med. 2015;39(3):504-507. doi: 10.5535/arm.2015.39.3.504.A survey of patients’ perspectives of steroid injection (ppyeojusa) in Korea
Bo-Mi Shin, Sung Jun Hong, Yun Hee Lim, Jae Hun Jeong, Ho Sik Moon, Hey Ran Choi, Sun Kyung Park, Richard Jin Woo Han, Jae Hun Kim
Korean J Pain. 2019;32(3):187-195. doi: 10.3344/kjp.2019.32.3.187.Quantitative assessment of steroid amount in the tissue after epidural steroid injection: a new rabbit model
Jungheum Cho, Joon Woo Lee, Eugene Lee, Yusuhn Kang, Ha Ra Cho, Dong Yoon Kim, Myoung Jin Ho, Myung Joo Kang, Yong Seok Choi
Korean J Pain. 2019;32(4):264-270. doi: 10.3344/kjp.2019.32.4.264.Effectiveness of virtual reality immersion on procedure-related pain and anxiety in outpatient pain clinic: an exploratory randomized controlled trial
Young Joo, Eun-Kyung Kim, Hyun-Gul Song, Haesun Jung, Hanssl Park, Jee Youn Moon
Korean J Pain. 2021;34(3):304-314. doi: 10.3344/kjp.2021.34.3.304.Analgesia after Epidural Dexamethasone is Further Enhanced by IV Dipyrone, but Not IV Parecoxibe Following Minor Orthopedic Surgery
Gabriela R Lauretti, Claudia CF Righeti, Antonio T Kitayama
Korean J Pain. 2014;27(4):345-352. doi: 10.3344/kjp.2014.27.4.345.Sufficient explanation of management affects patient satisfaction and the practice of post-treatment management in spinal pain, a multicenter study of 1007 patients
Jae Yun Kim, Jae Hang Shim, Sung Jun Hong, Jong Yeun Yang, Hey Ran Choi, Yun Hee Lim, Ho Sik Moon, Jaemoon Lee, Jae Hun Kim
Korean J Pain. 2017;30(2):116-125. doi: 10.3344/kjp.2017.30.2.116.
Reference
-
1. Cho NH, Jung YO, Lim SH, Chung CK, Kim HA. The prevalence and risk factors of low back pain in rural community residents of Korea. Spine (Phila Pa 1976). 2012; 37:2001–2010. PMID: 22588379.
Article2. Baek SR, Lim JY, Lim JY, Park JH, Lee JJ, Lee SB, et al. Prevalence of musculoskeletal pain in an elderly Korean population: results from the Korean Longitudinal Study on Health and Aging (KLoSHA). Arch Gerontol Geriatr. 2010; 51:e46–e51. PMID: 20005585.
Article3. Son KM, Cho NH, Lim SH, Kim HA. Prevalence and risk factor of neck pain in elderly Korean community residents. J Korean Med Sci. 2013; 28:680–686. PMID: 23678258.
Article4. Koh MJ, Park SY, Woo YS, Kang SH, Park SH, Chun HJ, et al. Assessing the prevalence of recurrent neck and shoulder pain in Korean high school male students: a cross-sectional observational study. Korean J Pain. 2012; 25:161–167. PMID: 22787546.
Article5. Henschke N, Maher CG, Refshauge KM, Herbert RD, Cumming RG, Bleasel J, et al. Prognosis in patients with recent onset low back pain in Australian primary care: inception cohort study. BMJ. 2008; 337:a171. PMID: 18614473.
Article6. El Sissi W, Arnaout A, Chaarani MW, Fouad M, El Assuity W, Zalzala M, et al. Prevalence of neuropathic pain among patients with chronic low-back pain in the Arabian Gulf Region assessed using the leeds assessment of neuropathic symptoms and signs pain scale. J Int Med Res. 2010; 38:2135–2145. PMID: 21227019.
Article7. Kaki AM, El-Yaski AZ, Youseif E. Identifying neuropathic pain among patients with chronic low-back pain: use of the Leeds Assessment of Neuropathic Symptoms and Signs pain scale. Reg Anesth Pain Med. 2005; 30:422–428. PMID: 16135345.
Article8. Beith ID, Kemp A, Kenyon J, Prout M, Chestnut TJ. Identifying neuropathic back and leg pain: a cross-sectional study. Pain. 2011; 152:1511–1516. PMID: 21396774.
Article9. Lievre JA, Bloch-Michel H, Pean G, Uro J. L'hydrocortisone en injection locale. Rev Rhum Mal Osteoartic. 1953; 20:310–311.10. Manchikanti L, Pampati V, Falco FJ, Hirsch JA. Growth of spinal interventional pain management techniques: analysis of utilization trends and Medicare expenditures 2000 to 2008. Spine (Phila Pa 1976). 2013; 38:157–168. PMID: 22781007.11. Benzon HT. Epidural steroid injections for low back pain and lumbosacral radiculopathy. Pain. 1986; 24:277–295. PMID: 3008063.
Article12. Wilkinson IM, Cohen SP. Epidural steroid injections. Curr Pain Headache Rep. 2012; 16:50–59. PMID: 22090263.
Article13. Wilkinson I, Cohen SP. Epidural steroids for spinal pain and radiculopathy: a narrative, evidence-based review. Curr Opin Anaesthesiol. 2013; [in press].14. Devor M, Govrin-Lippmann R, Raber P. Corticosteroids suppress ectopic neural discharge originating in experimental neuromas. Pain. 1985; 22:127–137. PMID: 4047699.
Article15. Johansson A, Hao J, Sjölund B. Local corticosteroid application blocks transmission in normal nociceptive C-fibres. Acta Anaesthesiol Scand. 1990; 34:335–338. PMID: 2167604.
Article16. Diwan S, Manchikanti L, Benyamin RM, Bryce DA, Geffert S, Hameed H, et al. Effectiveness of cervical epidural injections in the management of chronic neck and upper extremity pain. Pain Physician. 2012; 15:E405–E434. PMID: 22828692.17. Stafford MA, Peng P, Hill DA. Sciatica: a review of history, epidemiology, pathogenesis, and the role of epidural steroid injection in management. Br J Anaesth. 2007; 99:461–473. PMID: 17704089.
Article18. Parr AT, Manchikanti L, Hameed H, Conn A, Manchikanti KN, Benyamin RM, et al. Caudal epidural injections in the management of chronic low back pain: a systematic appraisal of the literature. Pain Physician. 2012; 15:E159–E198. PMID: 22622911.19. Quraishi NA. Transforaminal injection of corticosteroids for lumbar radiculopathy: systematic review and meta-analysis. Eur Spine J. 2012; 21:214–219. PMID: 21892774.
Article20. Jacobs S, Pullan PT, Potter JM, Shenfield GM. Adrenal suppression following extradural steroids. Anaesthesia. 1983; 38:953–956. PMID: 6314836.
Article21. Munck A. Glucocorticoid inhibition of glucose uptake by peripheral tissues: old and new evidence, molecular mechanisms, and physiological significance. Perspect Biol Med. 1971; 14:265–269. PMID: 5546253.
Article22. Tiso RL, Cutler T, Catania JA, Whalen K. Adverse central nervous system sequelae after selective transforaminal block: the role of corticosteroids. Spine J. 2004; 4:468–474. PMID: 15246308.
Article23. Glaser SE, Falco F. Paraplegia following a thoracolumbar transforaminal epidural steroid injection. Pain Physician. 2005; 8:309–314. PMID: 16850088.24. Lestner JM, Smith PB, Cohen-Wolkowiez M, Benjamin DK Jr, Hope WW. Antifungal agents and therapy for infants and children with invasive fungal infections: a pharmacological perspective. Br J Clin Pharmacol. 2013; 75:1381–1395. PMID: 23126319.
Article25. Even JL, Crosby CG, Song Y, McGirt MJ, Devin CJ. Effects of epidural steroid injections on blood glucose levels in patients with diabetes mellitus. Spine (Phila Pa 1976). 2012; 37:E46–E50. PMID: 21540770.
Article26. Cluff R, Mehio AK, Cohen SP, Chang Y, Sang CN, Stojanovic MP. The technical aspects of epidural steroid injections: a national survey. Anesth Analg. 2002; 95:403–408. PMID: 12145061.
Article27. Hirata F, Schiffmann E, Venkatasubramanian K, Salomon D, Axelrod J. A phospholipase A2 inhibitory protein in rabbit neutrophils induced by glucocorticoids. Proc Natl Acad Sci U S A. 1980; 77:2533–2536. PMID: 6930649.
Article28. Cohen SP, Bicket MC, Jamison D, Wilkinson I, Rathmell JP. Epidural steroids: a comprehensive, evidence-based review. Reg Anesth Pain Med. 2013; 38:175–200. PMID: 23598728.29. Kim D, Brown J. Efficacy and safety of lumbar epidural dexamethasone versus methylprednisolone in the treatment of lumbar radiculopathy: a comparison of soluble versus particulate steroids. Clin J Pain. 2011; 27:518–522. PMID: 21562412.
Article30. Dreyfuss P, Baker R, Bogduk N. Comparative effectiveness of cervical transforaminal injections with particulate and nonparticulate corticosteroid preparations for cervical radicular pain. Pain Med. 2006; 7:237–242. PMID: 16712623.
Article31. Park CH, Lee SH, Kim BI. Comparison of the effectiveness of lumbar transforaminal epidural injection with particulate and nonparticulate corticosteroids in lumbar radiating pain. Pain Med. 2010; 11:1654–1658. PMID: 20807343.
Article32. El-Yahchouchi C, Geske JR, Carter RE, Diehn FE, Wald JT, Murthy NS, et al. The noninferiority of the nonparticulate steroid dexamethasone vs the particulate steroids betamethasone and triamcinolone in lumbar transforaminal epidural steroid injections. Pain Med. 2013; 14:1650–1657. PMID: 23899304.
Article33. Meikle AW, Tyler FH. Potency and duration of action of glucocorticoids. Effects of hydrocortisone, prednisone and dexamethasone on human pituitary-adrenal function. Am J Med. 1977; 63:200–207. PMID: 888843.34. Olmarker K, Larsson K. Tumor necrosis factor alpha and nucleus-pulposus-induced nerve root injury. Spine (Phila Pa 1976). 1998; 23:2538–2544. PMID: 9854752.35. Bicket MC, Gupta A, Brown CH 4th, Cohen SP. Epidural injections for spinal pain: a systematic review and meta-analysis evaluating the "control" injections in randomized controlled trials. Anesthesiology. 2013; 119:907–931. PMID: 24195874.36. Manchikanti L, Boswell MV, Singh V, Benyamin RM, Fellows B, Abdi S, et al. Comprehensive evidence-based guidelines for interventional techniques in the management of chronic spinal pain. Pain Physician. 2009; 12:699–802. PMID: 19644537.37. Manchikanti L. Role of neuraxial steroids in interventional pain management. Pain Physician. 2002; 5:182–199. PMID: 16902669.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Persistent Hiccup after Epidural Steroid Injection: Case reports
- Epidural Steroid Injection
- Pneumocephalus after Epidural Steroid Injection: A case report
- Comparison of Transforaminal Epidural Steroid Injection and Lumbar/Caudal Epidural Steroid Injection for the Treatment of Lumbosacral Radiculopathy
- Selective Epidural Steroid Injection in a Patient with Refractory Radicular Leg Pain: A case report