Ann Dermatol.
2014 Dec;26(6):727-732. 10.5021/ad.2014.26.6.727.
Clinical Characteristics of Pruritus in Patients with Scalp Psoriasis and Their Relation with Intraepidermal Nerve Fiber Density
- Affiliations
-
- 1Department of Dermatology, Pusan National University School of Medicine, Busan, Korea. dockbs@pusan.ac.kr
- 2Biomedical Research Institute, Pusan National University Hospital, Busan, Korea.
- 3Research Institute for Convergence of Biomedical Science and Technology, Pusan National University Yangsan Hospital, Yangsan, Korea.
- KMID: 2264868
- DOI: http://doi.org/10.5021/ad.2014.26.6.727
Abstract
- BACKGROUND
The scalp is frequently affected in psoriasis patients, and pruritus can adversely affect the quality of life of affected patients. Few studies have assessed pruritus in scalp psoriasis.
OBJECTIVE
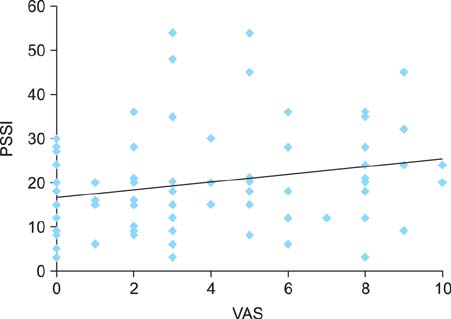
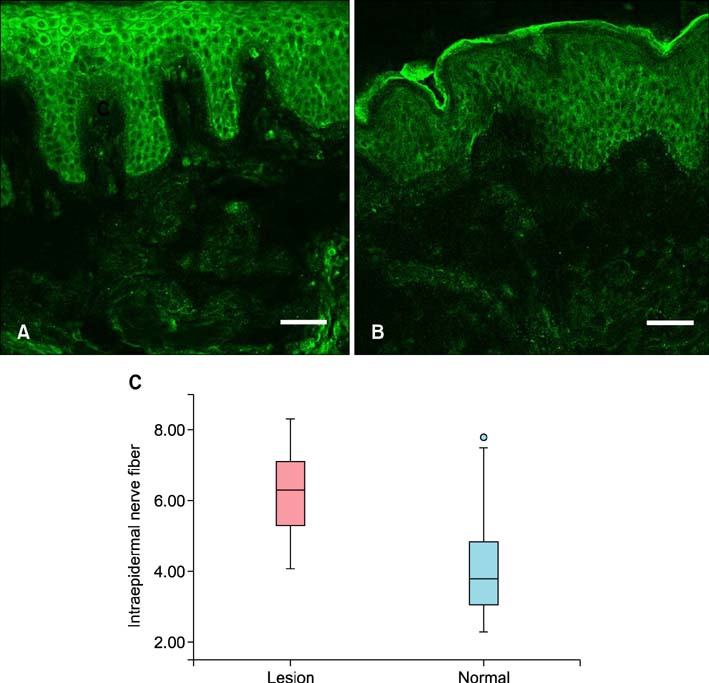
To determine the correlation among the clinical characteristics of pruritus, psoriasis scalp severity index (PSSI), and intraepidermal nerve fiber (IENF) density in psoriatic scalp lesions.
METHODS
Eighty patients (53 men, 27 women; mean age, 46.4 years; mean PSSI, 19.9) with scalp psoriasis were evaluated by using the PSSI and the Leuven itch scale. Biopsies were obtained from the lesional and nonlesional skin of 19 patients (10 men, 9 women; mean age, 37.8 years; mean PSSI, 25.8). Immunofluorescence staining of protein gene product 9.5 was performed to determine the IENF density.
RESULTS
Sixty-four patients (80%) complained of pruritus associated with scalp psoriasis, which negatively affected their quality of life to varying degrees. A moderate positive relation between PSSI score and pruritus intensity was identified (r=0.225 and p=0.044). The IENF density in psoriatic lesions was significantly higher than that in the nonlesional scalp (6.2+/-1.2 vs. 4.2+/-1.6, p<0.001). However, the correlations between IENF density and PSSI score, and IENF density and pruritus intensity were insignificant.
CONCLUSION
These results indicate that pruritus prevalence is high in patients with scalp psoriasis, and pruritus considerably influences the patients' daily lives and quality of life. In addition, high IENF density in psoriatic scalp lesions may play a role in the development of pruritus in scalp psoriasis.
Keyword
MeSH Terms
Figure
Cited by 1 articles
-
Histopathological Differential Diagnosis of Psoriasis and Seborrheic Dermatitis of the Scalp
Ji-Hye Park, Young Joon Park, Sue Kyoung Kim, Ji Eun Kwon, Hee Young Kang, Eun-So Lee, Jee Ho Choi, You Chan Kim
Ann Dermatol. 2016;28(4):427-432. doi: 10.5021/ad.2016.28.4.427.
Reference
-
1. Szepietowski JC, Reich A, Wi . 347;nicka B. Itching in patients suffering from psoriasis. Acta Dermatovenerol Croat. 2002; 10:221–226.2. Yosipovitch G, Goon A, Wee J, Chan YH, Goh CL. The prevalence and clinical characteristics of pruritus among patients with extensive psoriasis. Br J Dermatol. 2000; 143:969–973.
Article3. Reich A, Szepietowski JC. Mediators of pruritus in psoriasis. Mediators Inflamm. 2007; 2007:64727.
Article4. Nakamura M, Toyoda M, Morohashi M. Pruritogenic mediators in psoriasis vulgaris: comparative evaluation of itch-associated cutaneous factors. Br J Dermatol. 2003; 149:718–730.
Article5. Pergolizzi S, Vaccaro M, Magaudda L, Mondello MR, Arco A, Bramanti P, et al. Immunohistochemical study of epidermal nerve fibres in involved and uninvolved psoriatic skin using confocal laser scanning microscopy. Arch Dermatol Res. 1998; 290:483–489.
Article6. van de Kerkhof PC, de Hoop D, de Korte J, Kuipers MV. Scalp psoriasis, clinical presentations and therapeutic management. Dermatology. 1998; 197:326–334.
Article7. Bin Saif GA, Ericson ME, Yosipovitch G. The itchy scalp-scratching for an explanation. Exp Dermatol. 2011; 20:959–968.8. Haest C, Casaer MP, Daems A, De Vos B, Vermeersch E, Morren MA, et al. Measurement of itching: validation of the Leuven Itch Scale. Burns. 2011; 37:939–950.
Article9. Lauria G, Cornblath DR, Johansson O, McArthur JC, Mellgren SI, Nolano M, et al. European Federation of Neurological Societies. EFNS guidelines on the use of skin biopsy in the diagnosis of peripheral neuropathy. Eur J Neurol. 2005; 12:747–758.
Article10. Gupta MA, Gupta AK, Kirkby S, Weiner HK, Mace TM, Schork NJ, et al. Pruritus in psoriasis. A prospective study of some psychiatric and dermatologic correlates. Arch Dermatol. 1988; 124:1052–1057.
Article11. Gupta MA. Is chronic pain a variant of depressive illness? A critical review. Can J Psychiatry. 1986; 31:241–248.
Article12. Bondy B, Baghai TC, Minov C, Schüle C, Schwarz MJ, Zwanzger P, et al. Substance P serum levels are increased in major depression: preliminary results. Biol Psychiatry. 2003; 53:538–542.
Article13. Hägermark O, Hökfelt T, Pernow B. Flare and itch induced by substance P in human skin. J Invest Dermatol. 1978; 71:233–235.
Article14. Ellis CN, Berberian B, Sulica VI, Dodd WA, Jarratt MT, Katz HI, et al. A double-blind evaluation of topical capsaicin in pruritic psoriasis. J Am Acad Dermatol. 1993; 29:438–442.
Article15. Krueger G, Koo J, Lebwohl M, Menter A, Stern RS, Rolstad T. The impact of psoriasis on quality of life: results of a 1998 National Psoriasis Foundation patient-membership survey. Arch Dermatol. 2001; 137:280–284.16. Callis Duffin K, Wong B, Horn EJ, Krueger GG. Psoriatic arthritis is a strong predictor of sleep interference in patients with psoriasis. J Am Acad Dermatol. 2009; 60:604–608.
Article17. Taneda K, Tominaga M, Negi O, Tengara S, Kamo A, Ogawa H, et al. Evaluation of epidermal nerve density and opioid receptor levels in psoriatic itch. Br J Dermatol. 2011; 165:277–284.
Article18. Johansson O, Han SW, Enhamre A. Altered cutaneous innervation in psoriatic skin as revealed by PGP 9.5 immunohistochemistry. Arch Dermatol Res. 1991; 283:519–523.
Article19. Naukkarinen A, Nickoloff BJ, Farber EM. Quantification of cutaneous sensory nerves and their substance P content in psoriasis. J Invest Dermatol. 1989; 92:126–129.
Article20. Weddell G, Cowan MA, Palmer E, Ramaswamy S. Psoriatic skin. Arch Dermatol. 1965; 91:252–266.
Article