Allergy Asthma Respir Dis.
2015 Jan;3(1):86-89. 10.4168/aard.2015.3.1.86.
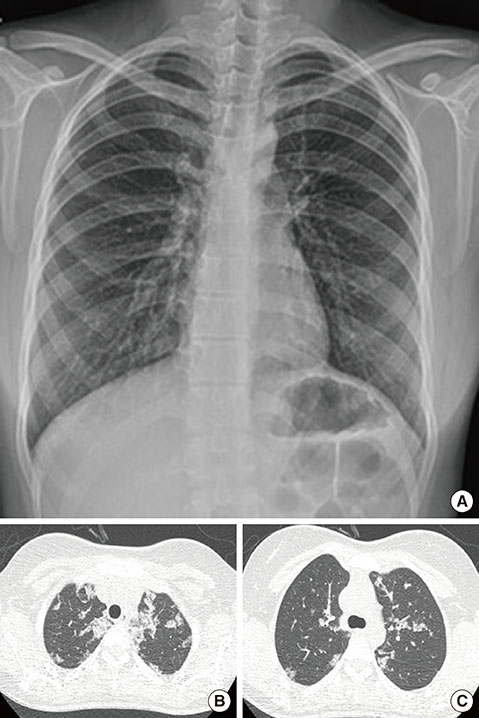
Pulmonary alveolar proteinosis in a 15-year-old girl
- Affiliations
-
- 1Department of Pediatrics, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea. kmaped@skku.edu
- 2Department of Thoracic Surgery, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea.
- 3Department of Pathology, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea.
- KMID: 2262285
- DOI: http://doi.org/10.4168/aard.2015.3.1.86
Abstract
- Pulmonary alveolar proteinosis (PAP) is a diffuse lung disease characterized by the accumulation of lipoproteins derived from surfactants in the distal air space. The lack of granulocyte macrophage colony-stimulating factor is believed to contribute to macrophage dysfunction and the impaired processing of surfactants. Because the prevalence of PAP in the general population is less than 1 in 200,000, and the typical age at presentation is 35 to 50 years, PAP is a very rare disease in children. To the best of our knowledge, there has been no Korean report on PAP in children. We describe here a patient who was diagnosed with PAP at the aged 15 years.
Keyword
MeSH Terms
Figure
Reference
-
1. Trapnell BC, Whitsett JA, Nakata K. Pulmonary alveolar proteinosis. N Engl J Med. 2003; 349:2527–2539.
Article2. Carey B, Trapnell BC. The molecular basis of pulmonary alveolar proteinosis. Clin Immunol. 2010; 135:223–235.
Article3. Froudarakis ME, Koutsopoulos A, Mihailidou HP. Total lung lavage by awake flexible fiberoptic bronchoscope in a 13-year-old girl with pulmonary alveolar proteinosis. Respir Med. 2007; 101:366–369.
Article4. Byun MK, Kim DS, Kim YW, Chung MP, Shim JJ, Cha SI, et al. Clinical features and outcomes of idiopathic pulmonary alveolar proteinosis in Korean population. J Korean Med Sci. 2010; 25:393–398.
Article5. Suzuki T, Sakagami T, Rubin BK, Nogee LM, Wood RE, Zimmerman SL, et al. Familial pulmonary alveolar proteinosis caused by mutations in CSF2RA. J Exp Med. 2008; 205:2703–2710.
Article6. Woo DH, Park JE, Ryu YH, Kim HJ, Shin KC, Chung JH, et al. A case of pulmonary alveolar proteinosis. Yeungnam Univ J Med. 2010; 27:57–62.
Article7. Rosen SH, Castleman B, Liebow AA. Pulmonary alveolar proteinosis. N Engl J Med. 1958; 258:1123–1142.
Article8. Stanley E, Lieschke GJ, Grail D, Metcalf D, Hodgson G, Gall JA, et al. Granulocyte/macrophage colony-stimulating factor-deficient mice show no major perturbation of hematopoiesis but develop a characteristic pulmonary pathology. Proc Natl Acad Sci U S A. 1994; 91:5592–5596.
Article9. Kitamura T, Tanaka N, Watanabe J, Uchida , Kanegasaki S, Yamada Y, et al. Idiopathic pulmonary alveolar proteinosis as an autoimmune disease with neutralizing antibody against granulocyte/macrophage colony-stimulating factor. J Exp Med. 1999; 190:875–880.
Article10. Suzuki T, Sakagami T, Young LR, Carey BC, Wood RE, Luisetti M, et al. Hereditary pulmonary alveolar proteinosis: pathogenesis, presentation, diagnosis, and therapy. Am J Respir Crit Care Med. 2010; 182:1292–1304.11. Ceruti M, Rodi G, Stella GM, Adami A, Bolongaro A, Baritussio A, et al. Successful whole lung lavage in pulmonary alveolar proteinosis secondary to lysinuric protein intolerance: a case report. Orphanet J Rare Dis. 2007; 2:14.
Article12. Wang BM, Stern EJ, Schmidt RA, Pierson DJ. Diagnosing pulmonary alveolar proteinosis. A review and an update. Chest. 1997; 111:460–466.13. Seymour JF, Presneill JJ, Schoch OD, Downie GH, Moore PE, Doyle IR, et al. Therapeutic efficacy of granulocyte-macrophage colony-stimulating factor in patients with idiopathic acquired alveolar proteinosis. Am J Respir Crit Care Med. 2001; 163:524–531.
Article14. Song JW, Park SH, Kang KW. A case of idiopathic pulmonary alveolar proteinosis treated with granulocyte-macrophage colony stimulating factor (GM-CSF) after partial response to whole lung lavage. Tuberc Respir Dis. 2009; 67:569–573.
Article15. Tazawa R, Trapnell BC, Inoue Y, Arai T, Takada T, Nasuhara Y, et al. Inhaled granulocyte/macrophage-colony stimulating factor as therapy for pulmonary alveolar proteinosis. Am J Respir Crit Care Med. 2010; 181:1345–1354.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Anesthetic Management for Whole-Lung Lavage in a Patient with Pulmonary Alveolar Proteinosis
- Anesthetic Management for Sequential Bronchoalveolar Lavage in a Patient with Pulmonary Alveolar Proteinosis: A case report
- Bilateral Sequential Bronchopulmonary Lavage in One Stage for Recurred Pulmonary Alveolar Proteinosis: A case report
- Anesthetic Management of Lung Lavage in Patient with Pulmonary Alveolar Proteinosis Related to Pneumoconiosis: A case report
- Whole Lung Lavage and Extracorporeal Membrane Oxygenation in a Patient with Pulmonary Alveolar Proteinosis and Lung Cancer