Korean J Hematol.
2008 Jun;43(2):77-82. 10.5045/kjh.2008.43.2.77.
Patterns of Obesity during Anti-cancer Chemotherapy in Children with Acute Lymphoblastic Leukemia
- Affiliations
-
- 11Department of Pediatrics, Hanyang University College of Medicine, Seoul, Korea. heagori@hanmail.net
- 21Department of Pediatrics, Dong-A University College of Medicine, Busan, Korea.
- KMID: 2252199
- DOI: http://doi.org/10.5045/kjh.2008.43.2.77
Abstract
-
BACKGROUND: We evaluated the pattern as well as the predictive factors of obesity in children with acute lymphoblastic leukemia (ALL) according to body mass index (BMI) changes that occur during anticancer chemotherapy.
METHODS
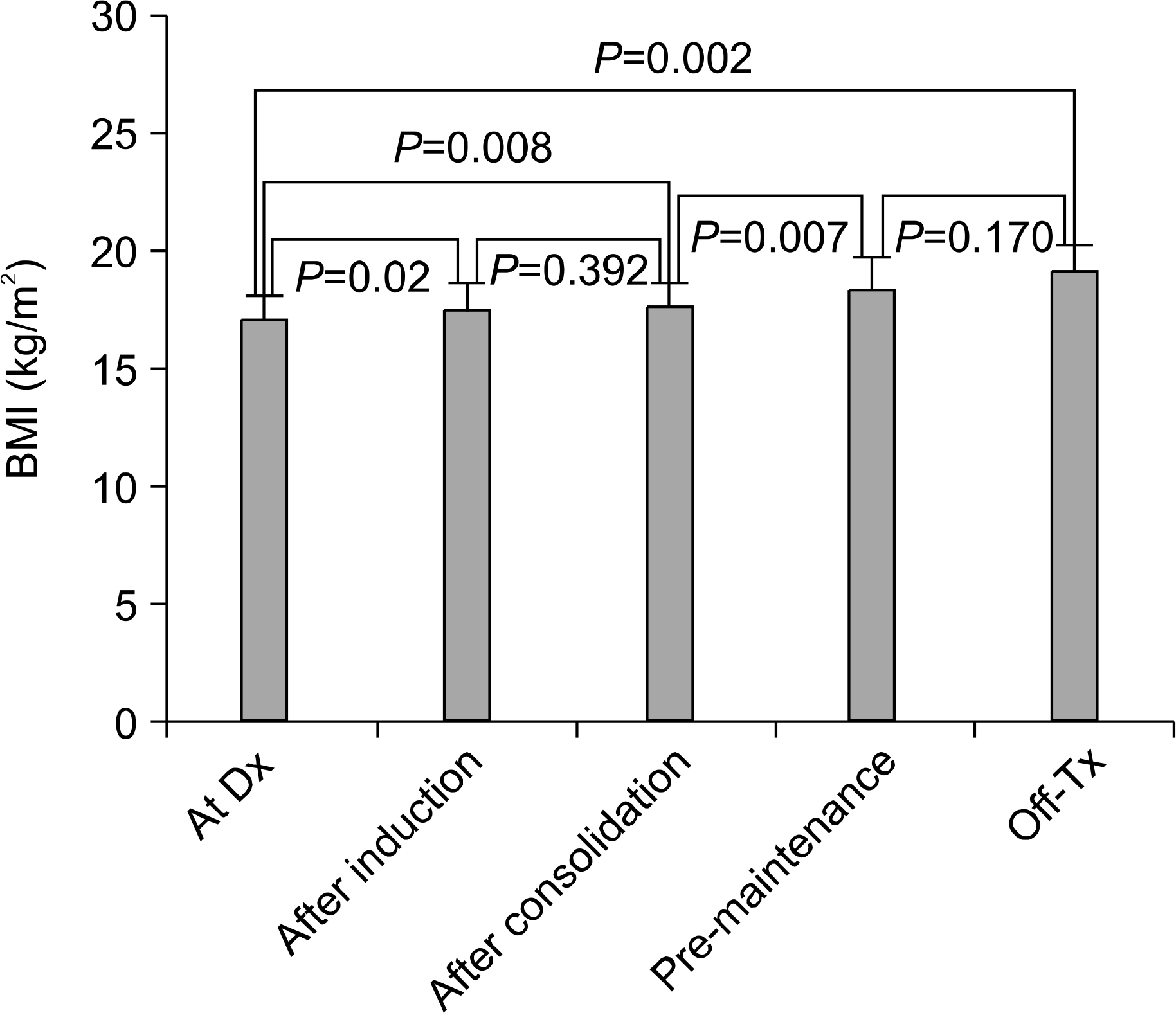
We reviewed the medical records of 58 patients who were diagnosed with ALL between 1995 and 2006 at the Department of Pediatrics at Hanyang University Hospital and Dong-A University Hospital. Five relapsed cases were excluded. The heights and weights of 55 children were measured at diagnosis, after induction, after consolidation, before maintenance and at the end of therapy. We analyzed the body mass index (BMI, kg/m(2)) for each treatment phase and evaluated the BMI differences for patients who received or did not receive cranial radiotherapy.
RESULTS
The BMI increased in five children (10.4%) among the 48 children who were not obese at diagnosis. According to the treatment phase, the BMI of study patients significantly increased during induction and during chemotherapy. Even though the BMI also significantly increased according to the treatment phases in the children who underwent cranial radiotherapy, the BMI differences between patients that received or did not receive cranial radiotherapy were not statistically significant.
CONCLUSION
We suggest that the risk for obesity in children with ALL should be considered even during chemotherapy. Physical activities, including physiotherapy, should be encouraged to prevent obesity, particularly during the long-term use of corticosteroids and during hospital admission.
MeSH Terms
Figure
Reference
-
1). Friedman DL., Meadows AT. Late effects of childhood cancer therapy. Pediatr Clin North Am. 2002. 49:1083–106.
Article2). Sklar CA., Mertens AC., Walter A, et al. Changes in body mass index and prevalence of overweight in survivors of childhood acute lymphoblastic leukemia: role of cranial irradiation. Med Pediatr Oncol. 2000. 35:91–5.
Article3). Reilly JJ., Brougham C., Montgomery C., Richardson F., Kelly RA., Gibson BE. Effect of glucocorticoid therapy on energy intake in children treated for acute lymphoblastic leukemia. J Clin Endocrinol Metab. 2001. 86:3742–5.
Article4). Chong PK., Jung RT., Scrimgeour CM., Rennie MJ. The effect of pharmacological dosages of glucocorticoids on free living total energy expenditure in man. Clin Endocrinol (Oxf). 1994. 40:577–81.
Article5). Warner JT., Bell W., Webb DK., Gregory JW. Daily energy expenditure and physical activity in survivors of childhood malignancy. Pediatr Res. 1998. 43:607–13.
Article6). Kang YJ., Hong CH., Hong YJ. The prevalence of childhood and adolescent obesity over the last 18 years in Seoul area. Korean J Nutrition. 1997. 30:832–9.7). Kim HM., Park J., Kim HS., Kim DH., Park SH. Obesity and cardiovascular risk factors in Korean children and adolescents aged 10-18 years from the Korean National Health and Nutrition Examination Survey. 1998 and 2001. Am J Epidemiol. 2006. 164:787–93.
Article8). Zee P., Chen CH. Prevalence of obesity in children after therapy for acute lymphoblastic leukemia. Am J Pediatr Hematol Oncol. 1986. 8:294–9.
Article9). Oeffinger KC., Buchanan GR., Eshelman DA, et al. Cardiovascular risk factors in young adult survivors of childhood acute lymphoblastic leukemia. J Pediart Hemaol Oncol. 2001. 23:424–30.
Article10). Chow EJ., Pihoker C., Hunt K., Wilkinson K., Friedman DL. Obesity and hypertension among children after treatment for acute lymphoblastic leukemia. Cancer. 2007. 110:2313–20.
Article11). Rogers PC., Meacham LR., Oeffinger KC., Henry DW., Lange BJ. Obesity in pediatric oncology. Pediatr Blood Cancer. 2005. 45:881–91.
Article12). Lee YJ., Kim YH., Hah JO. Prevalence of obesity and cardiovascular risk factors in survivors of childhood acute lymphoblastic leukemia. Korean J Pediatr Hematol-Oncol. 2003. 10:198–205.13). Oeffinger KC., Mertens AC., Sklar CA, et al. Obesity in adult survivors of childhood acute lymphoblastic leukemia: a report from the childhood cancer survivors study. J Clin Oncol. 2003. 21:1359–65.14). Willox JC., Corr J., Shaw J., Richardson M., Calman KC., Drennan M. Prednisolone as an appetite stimulant in patients with cancer. Br Med J (Clin Res Ed). 1984. 288:27.
Article15). Razzouk BI., Rose SR., Hongeng S, et al. Obesity in survivors of childhood acute lymphoblastic leukemia and lymphoma. J Clin Oncol. 2007. 25:1183–9.
Article16). Reilly JJ., Ventham JC., Ralston JM., Donaldson M., Gibson B. Reduced energy expenditure in preobese children treated for acute lymphoblastic leukemia. Pediatr Res. 1998. 44:557–62.
Article17). Zeltzer LK., Chen E., Weiss R, et al. Comparision of psychologic outcome in adult survivors of childhood acute lymphoblastic leukemias vs sibling controls: a cooperative Children's Cancer Group and National Institute of Health study. J Clin Oncol. 1997. 15:547–56.18). Nysom K., Holm K., Michaelsen KF., Hertz H., Müller J., Molggard C. Degree of fatness after treatment for acute lymphoblastic leukemia in childhood. J Clin Endocrinol Metab. 1999. 84:4591–6.19). Reilly JJ., Blacklock CJ., Dale E., Donaldson M., Gibson BE. Resting metabolic rate and obesity in childhood acute lymphoblascitc leukemia. Int J Obes Relat Metab Disord. 1996. 20:1130–2.20). Field AE., Laird N., Steinberg E., Fallon E., Semega-Janneh M., Yanovski JA. Which metric of relative weight best captures body fatness in children? Obse Res. 2003. 11:1345–52.
Article21). Lee JH., Seo HJ., Kim JY., Ko CW., Lee KS. Late endocrine complications in childhood cancer survivors. Korean J Pediatr Hematol-Oncol. 2005. 12:55–62.22). Sklar CA. Growth and neuroendocrine dysfunction following therapy for childhood cancer. Pediatr Clin North Am. 1997. 44:489–503.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Norovirus Infection in Children with Acute Lymphoblastic Leukemia
- A Case of Pneumocystis carinii Pneumonia with Febrile Neutropenia in Acute Lymphoblastic Leukemia
- Pancreatitis Induced by 6-mercaptopurine and 6-thioguanine in Childhood Acute Lymphoblastic Leukemia
- Chemotherapy of Acute Lymphoblastic Leukemia in Children
- Precursor B-Cell Acute Lymphoblastic Leukemia in Two Patients with a History of Cytotoxic Therapy