Korean J Crit Care Med.
2015 Feb;30(1):34-37. 10.4266/kjccm.2015.30.1.34.
Effective Postoperative Use of Dexmedetomidine in a Child with Severe Pulmonary Arterial Hypertension Secondary to Congenital Ventricular Septal Defect
- Affiliations
-
- 1Department of Thoracic and Cardiovascular Surgery, Inje University Seoul Paik Hospital, Seoul, Korea. lukeykim@yahoo.com
- KMID: 2227699
- DOI: http://doi.org/10.4266/kjccm.2015.30.1.34
Abstract
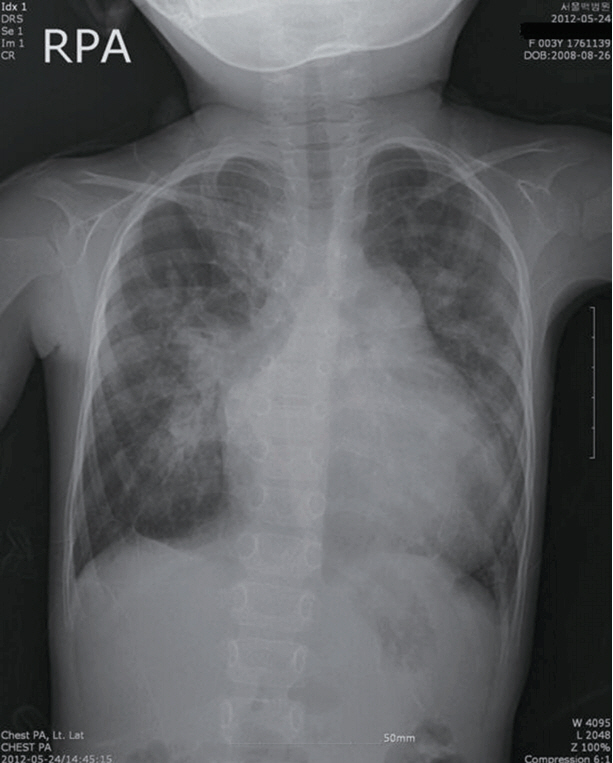
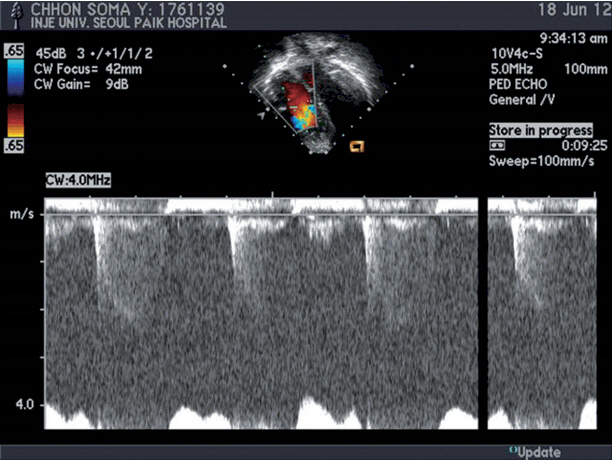
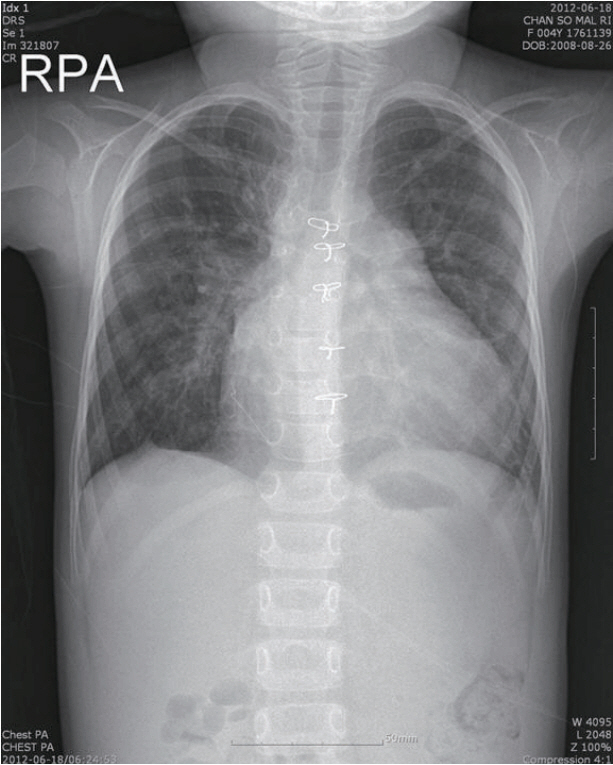
- Although alpha2-adrenoceptor agonists are widely used as postoperative sedatives in adults, the postoperative effects in pediatric patients with secondary pulmonary arterial hypertension (PAH) due to congenital heart disease are not well known. We experienced a case of successful ventilator weaning with continuous intravenous administration of dexmedetomidine (DEX) after surgical correction in a 46-month-old child with congenital ventricular septal defect (VSD) with severe PAH. She underwent VSD closure on cardiopulmonary bypass (CPB). After successful weaning from the CPB, hemodynamics and oxygenation were stabilized on DEX and nitroglycerin in the intensive care unit. The patient was successfully weaned from the ventilator 46 hours after surgery. The transthoracic echocardiogram two weeks after surgery showed a closed VSD with no residual shunt and trivial tricuspid regurgitation (Vmax = 2.5 m/sec) without PAH.
MeSH Terms
-
Administration, Intravenous
Adult
Cardiopulmonary Bypass
Child*
Child, Preschool
Dexmedetomidine*
Heart Defects, Congenital
Heart Septal Defects, Ventricular*
Hemodynamics
Humans
Hypertension*
Hypnotics and Sedatives
Intensive Care Units
Nitroglycerin
Oxygen
Tricuspid Valve Insufficiency
Ventilator Weaning
Ventilators, Mechanical
Weaning
Dexmedetomidine
Hypnotics and Sedatives
Nitroglycerin
Oxygen
Figure
Reference
-
References
1. Carmosino MJ, Friesen RH, Doran A, Ivy DD. Perioperative complications in children with pulmonary hypertension undergoing noncardiac surgery or cardiac catheterization. Anesth Analg. 2007; 104:521–7.
Article2. Bloor BC, Ward DS, Belleville JP, Maze M. Effects of intravenous dexmedetomidine in humans. II. Hemodynamic changes. Anesthesiology. 1992; 77:1134–42.3. Belleville JP, Ward DS, Bloor BC, Maze M. Effects of intravenous dexmedetomidine in humans. I. Sedation, ventilation, and metabolic rate. Anesthesiology. 1992; 77:1125–33.4. Hall JE, Uhrich TD, Barney JA, Arain SR, Ebert TJ. Sedative, amnestic, and analgesic properties of small dose dexmedetomidine infusions. Anesth Analg. 2000; 90:699–705.5. Isik B, Arslan M, Tunga AD, Kurtipek O. Dexmedetomidine decreases emergence agitation in pediatric patients after sevoflurane anesthesia without surgery. Paediatr Anaesth. 2006; 16:748–53.
Article6. Mukhtar AM, Obayah EM, Hassona AM. The use of dexmedetomidine in pediatric cardiac surgery. Anesth Analg. 2006; 103:52–6.
Article7. Nemoto S, Sasaki T, Ozawa H, Katsumata T, Asano M, Kusaka Y, et al. Dexmedetomidine enables not only optimal sedation but also minimizing life-threatening morbidities in intensive care management after pediatric cardiovascular surgery. Crit Care Med. 2011; 39:238.8. Buck ML, Willson DF. Use of dexmedetomidine in the pediatric intensive care unit. Pharmacotherapy. 2008; 28:51–7.
Article9. Bejian S, Valasek C, Nigro JJ, Cleveland DC, Willis BC. Prolonged use of dexmedetomidine in the paediatric cardiothoracic intensive care unit. Cardiol Young. 2009; 19:98–104.
Article10. Shehabi Y, Ruettimann U, Adamson H, Innes R, Ickeringill M. Dexmedetomidine infusion for more than 24 hours in critically ill patients: sedative and cardiovascular effects. Intensive Care Med. 2004; 30:2188–96.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The Effects of Hemodynamic Findings on Development of Pulmonary Vascular Changes in Patients with Ventricular Septal Defect
- Pulmonary Arterial Thrombosis in a Patient With an Atrial Septal Defect and Eisenmenger Syndrome
- Large Atrial Septal Defect Closure in a Patient with Severe Pulmonary Arterial Hypertension
- The effect of perioperative inhaled iloprost on congenital heart disease with severe pulmonary arterial hypertension
- Unidirectional Valve Patch Closure for Ventricular Septal Defect with Severe Pulmonary Hypertension: A Case Report