Korean Circ J.
2009 Sep;39(9):382-385. 10.4070/kcj.2009.39.9.382.
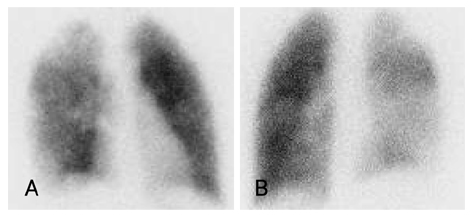
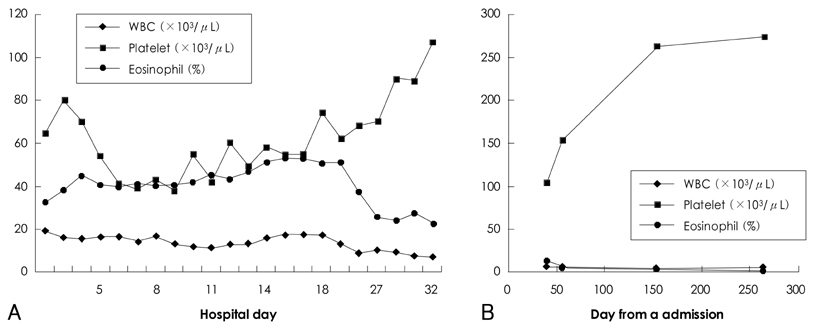
A Case of Pulmonary Thromboembolism Associated With Hypereosinophilia in a Child
- Affiliations
-
- 1Department of Pediatrics, Seoul National University Children's Hospital, Seoul National University College of Medicine, Seoul, Korea. eunjbaek@snu.ac.kr
- KMID: 2225675
- DOI: http://doi.org/10.4070/kcj.2009.39.9.382
Abstract
- Pulmonary thromboembolism is a very rare event in children, but the mortality rate is reported to be approximately 10%. The majority of children with thromboemboli have multiple risk factors, such as a catheter-related thrombosis, an infection, and a congenital prothrombotic disorder. Hypereosinophilia is very rarely associated with pulmonary emboli in adults; however, this condition has not been reported in children. We present a 12-year-old boy who had a pulmonary thromboembolism and deep vein thrombosis associated with hypereosinophilia and thrombocytopenia. The thromboembolism was managed with anticoagulant therapy and the hypereosinophilia resolved spontaneously.
Keyword
MeSH Terms
Figure
Reference
-
1. Goldenberg NA, Bernard TJ. Venous thromboembolism in children. Pediatr Clin North Am. 2008. 55:305–322. vii2. Stein PD, Kayali F, Olson RE. Incidence of venous thromboembolism in infants and children: data from the National Hospital Discharge Survey. J Pediatr. 2004. 145:563–565.3. Biss TT, Brandao LR, Kahr WH, Chan AK, Williams S. Clinical features and outcome of pulmonary embolism in children. Br J Haematol. 2008. 142:808–818.4. van Ommen CH, Heijboer H, Buller HR, Hirasing RA, Heijmans HS, Peters M. Venous thromboembolism in childhood: a prospective two-year registry in The Netherlands. J Pediatr. 2001. 139:676–681.5. Browse NL, Thomas ML. Source of non-lethal pulmonary emboli. Lancet. 1974. 1:258–259.6. Moon HJ, Rhim CY, Kim GW, et al. Risk factors of deep vein thrombosis and pulmonary embolism in Korean. Korean Circ J. 2005. 35:474–479.7. Sato Y, Fukunaga T, Hayashi T, Asada Y. Hypereosinophilic syndrome associated with occlusive coronary thrombosis and right ventricular thrombus. Pathol Int. 2008. 58:138–141.8. Uemura K, Nakajima M, Yamauchi N, Fukayama M, Yoshida K. Sudden death of a patient with primary hypereosinophilia, colon tumours, and pulmonary emboli. J Clin Pathol. 2004. 57:541–543.9. Sherer Y, Salomon O, Livneh A, Pras M, Langevitz P. Thromboembolism in a patient with transient eosinophilia and thrombocytopenia. Clin Lab Haematol. 2000. 22:247–249.10. Weller PF, Bubley GJ. The idiopathic hypereosinophilic syndrome. Blood. 1994. 83:2759–2779.11. Ribeiro A, Lindmarker P, Juhlin-Dannfelt A, Johnsson H, Jorfeldt L. Echocardiography Doppler in pulmonary embolism: right ventricular dysfunction as a predictor of mortality rate. Am Heart J. 1997. 134:479–487.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Pulmonary thromboembolism occurred immediately after leg elevation under induction of general anesthesia in a patient with femur fracture : A case report
- Fatal Pulmonary Thromboembolism Caused by Popliteal Vein Aneurysm
- Thromboembolism in Pulmonary Arteries Following Knee Arthroscopy under Spinal Anesthesia
- Clinical Year in Review of Venous Thromboembolism
- Pulmonary Artery Intimal Sarcoma Involving the Peripheral Pulmonary Artery, Initially Misdiagnosed as Pulmonary Artery Thromboembolism and Vasculitis: A Case Report