J Korean Ophthalmol Soc.
2013 May;54(5):818-822. 10.3341/jkos.2013.54.5.818.
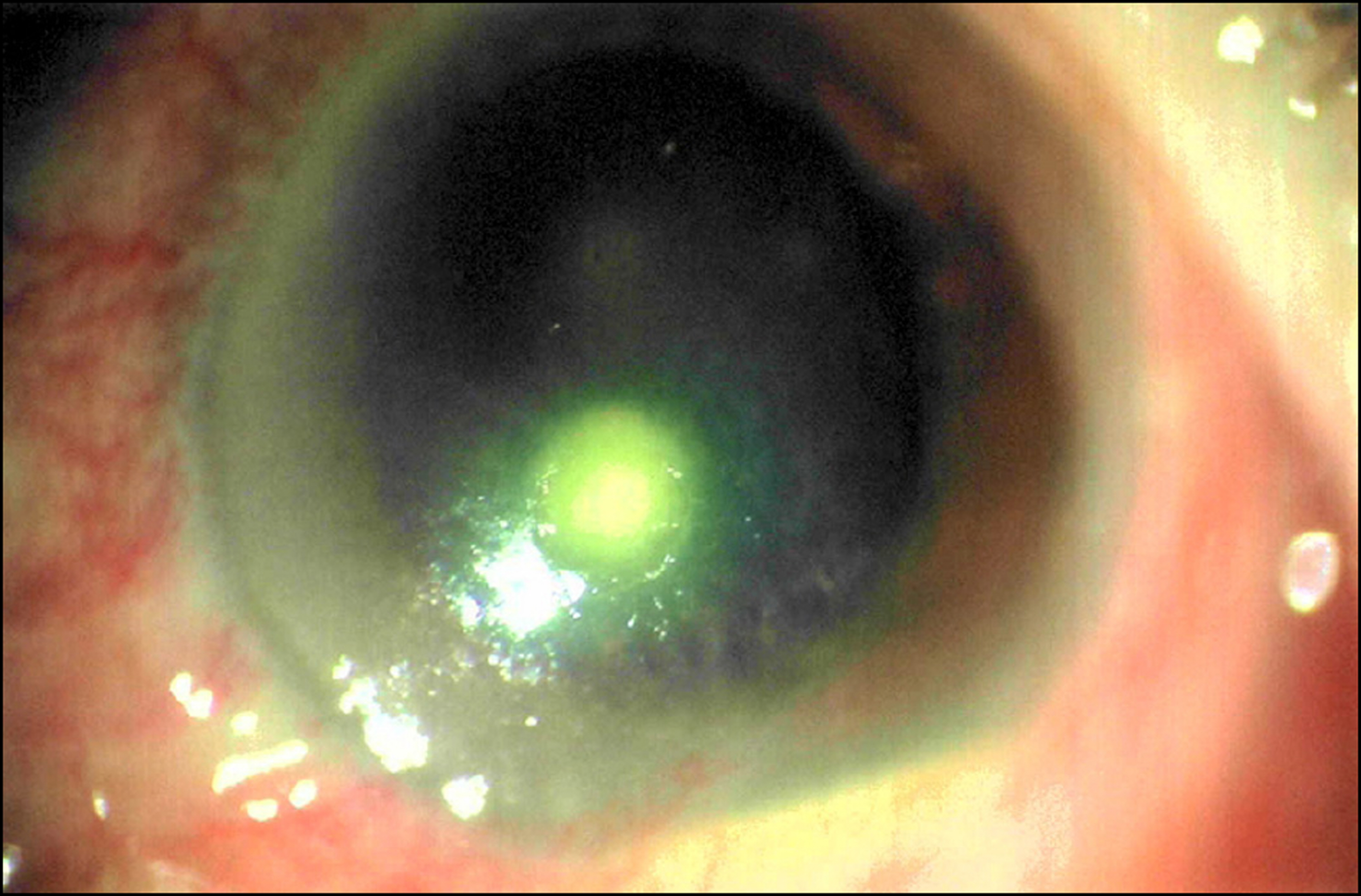
A Report of Five Cases of Mixed Candida and Bacterial Keratitis
- Affiliations
-
- 1Department of Ophthalmology, Chonbuk National University Medical School, Jeonju, Korea. You2ic@paran.com
- KMID: 2217053
- DOI: http://doi.org/10.3341/jkos.2013.54.5.818
Abstract
- PURPOSE
To report the clinical manifestations and prognoses in 5 cases of mixed Candida and bacterial keratitis and present a literature review on mixed fungal and bacterial keratitis.
CASE SUMMARY
Five eyes of 5 patients (1 male, 4 female) diagnosed as mixed Candida and bacterial keratitis by corneal smear and culture were included in the present study. Patient mean age was 62.80 years. All patients had preexisting ocular or systemic conditions as predisposing factors for mixed Candida and bacterial keratitis. The most common Candida species isolated was Candida albicans (3 eyes, 60%), while Staphylococcus (3 eyes, 60%) was the most common mixed bacterial species. The average size of ulceration was 7.02 mm2. In 2 eyes (40%), the lesions were located at the corneal center. The depth of the infiltration was significant in all cases, and hypopyon was present in 2 eyes (40%). On the initial visit, the visual acuity was counting fingers or worse in all cases. Four eyes (80%) unresponsive to the topical and systemic treatment underwent surgical intervention but only 1 eye (20%), which had responded to the topical and systemic treatment, showed acuity improvement of more than 1 line on the final visit.
CONCLUSIONS
In managing chronically compromised cornea, the possibility of mixed infections with Candida and bacterial organisms should be considered as keratitis shows poor prognosis.
Keyword
MeSH Terms
Figure
Reference
-
References
1. Hassan HM, Papanikolaou T, Mariatos G, et al. Candida albicans keratitis in an immunocompromised patient. Clin Ophthalmol. 2010; 4:1211–5.
Article2. Sun RL, Jones DB, Wilhelmus KR. Clinical characteristics and outcome of Candida keratitis. Am J Ophthalmol. 2007; 143:1043–5.
Article3. Ahn M, Yoon KC, Ryu SK, et al. Clinical aspects and prognosis of mixed microbial (bacterial and fungal) keratitis. Cornea. 2011; 30:409–13.
Article4. Kim JH, Shin HH, Song JS, Kim HM. Infectious keratitis caused by Stenotrophomonas maltophilia and yeast simultaneously. Cornea. 2006; 25:1234–6.
Article5. Kim JY, Yoon KC, Park YG, et al. Age-related clinical analysis of infectious keratitis in two tertiary centers. J Korean Ophthalmol Soc. 2010; 51:927–34.
Article6. Sun HJ, Lee JY, Kim SY, Jung MS. Clinical features of infectious keratitis in west coast area of chungcheongnam-do, Korea. J Korean Ophthalmol Soc. 2010; 51:658–63.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Efficacy of Fluconazole in The Treatment of Candida albicans Keratitis in Rabbits
- Moxifloxacin Mixed Augmented Amniotic Membrane Transplantation for Perforating Infectious Keratitis
- The Effect of Ketoconazole in the Treatment of Candida albicans Keratitis in Rabbits
- Analysis on Inpatients With Infectious Keratitis: Causative Organisms, Clinical Aspects and Risk Factors
- Excimer Laser Phototherapeutic Keratectomy for Experimental Fungal Keratitis