J Clin Neurol.
2015 Jan;11(1):87-91. 10.3988/jcn.2015.11.1.87.
Paraneoplastic Limbic Encephalitis in a Male with Squamous Cell Carcinoma of the Lung
- Affiliations
-
- 1Department of Medical Oncology, Catalan Institute of Oncology (ICO), Girona, Spain. rporta@iconcologia.net
- 2Girona Biomedical Research Institute (IDIBGi), Girona, Spain.
- 3Department of Medical Sciences, School of Medicine, University of Girona, Girona, Spain.
- 4Cancer Registry of Girona, Girona, Spain.
- 5Department of Neurology, Dr. Josep Trueta University Hospital, Girona, Spain.
- 6Department of Neuroradiology, Vall d'Hebron University Hospital, Barcelona, Spain.
- KMID: 2179577
- DOI: http://doi.org/10.3988/jcn.2015.11.1.87
Abstract
- BACKGROUND
Paraneoplastic limbic encephalitis (PLE) is a rare syndrome characterized by memory impairment, symptoms of hypothalamic dysfunction, and seizures. It commonly precedes the diagnosis of cancer. Small-cell lung cancer is the neoplasm that is most frequently reported as the etiology underlying PLE.
CASE REPORT
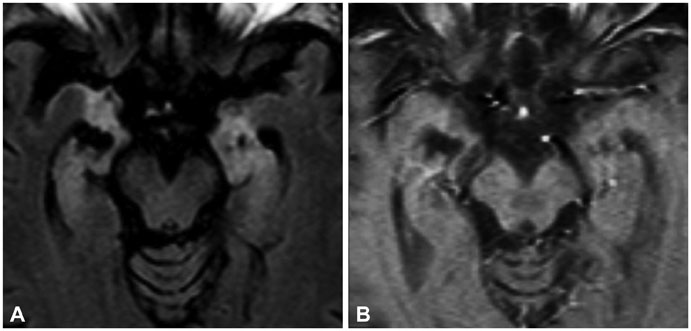
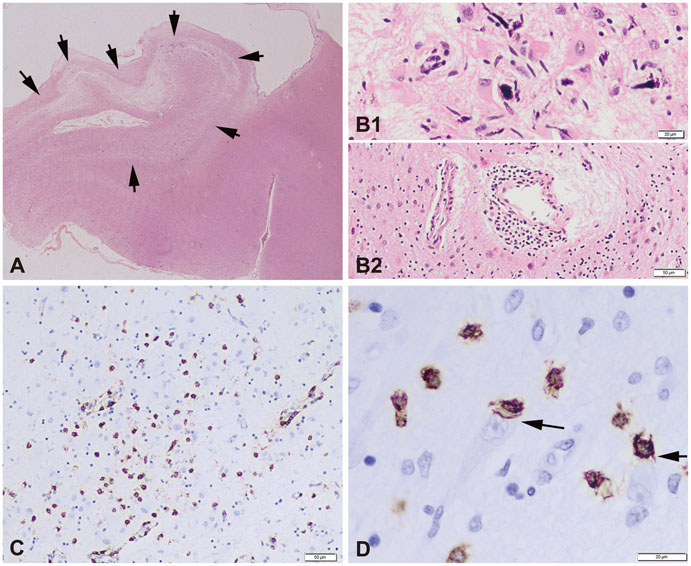
This report describes a male patient who presented with neurologic symptoms consistent with anterograde amnesia, apathy, and disorientation. MRI revealed diffuse hyperintensities located predominantly in the medial bitemporal lobes, basal ganglia, frontal lobes, and leptomeninges on fluid attenuated inversion recovery images, suggesting PLE. Study of the primary tumor revealed squamous cell carcinoma of the lung. The patient was treated with neoadjuvant chemotherapy followed by surgery and adjuvant chemoradiotherapy, which resulted in his neurologic symptoms gradually improving.
CONCLUSIONS
PLE might be a rare debut of squamous cell carcinoma of the lung. Treatment of the primary tumor may improve the neurologic symptoms.
MeSH Terms
Figure
Reference
-
1. Graus F, Delattre JY, Antoine JC, Dalmau J, Giometto B, Grisold W, et al. Recommended diagnostic criteria for paraneoplastic neurological syndromes. J Neurol Neurosurg Psychiatry. 2004; 75:1135–1140.
Article2. Bataller L, Kleopa KA, Wu GF, Rossi JE, Rosenfeld MR, Dalmau J. Autoimmune limbic encephalitis in 39 patients: immunophenotypes and outcomes. J Neurol Neurosurg Psychiatry. 2007; 78:381–385.
Article3. Dropcho EJ. Update on paraneoplastic syndromes. Curr Opin Neurol. 2005; 18:331–336.
Article4. Dirr LY, Elster AD, Donofrio PD, Smith M. Evolution of brain MRI abnormalities in limbic encephalitis. Neurology. 1990; 40:1304–1306.
Article5. Lawn ND, Westmoreland BF, Kiely MJ, Lennon VA, Vernino S. Clinical, magnetic resonance imaging, and electroencephalographic findings in paraneoplastic limbic encephalitis. Mayo Clin Proc. 2003; 78:1363–1368.
Article6. Brierley JB, Corsellis JA, Hierons R, Nevin S. Subacute encephalitis of later adult life. Mainly affecting the limbic areas. Brain. 1960; 83:357–368.
Article7. Corsellis JA, Goldberg GJ, Norton AR. "Limbic encephalitis" and its association with carcinoma. Brain. 1968; 91:481–496.
Article8. Burton GV, Bullard DE, Walther PJ, Burger PC. Paraneoplastic limbic encephalopathy with testicular carcinoma. A reversible neurologic syndrome. Cancer. 1988; 62:2248–2251.
Article9. Dögel D, Beuing O, Koenigsmann M, Diete S. [Paraneoplastic limbic encephalitis resulting from non-Hodgkin-lymphoma: two case reports]. Fortschr Neurol Psychiatr. 2008; 76:41–46.
Article10. Alamowitch S, Graus F, Uchuya M, Reñé R, Bescansa E, Delattre JY. Limbic encephalitis and small cell lung cancer. Clinical and immunological features. Brain. 1997; 120(Pt 6):923–928.
Article11. Rajappa S, Digumarti R, Immaneni SR, Parage M. Primary renal lymphoma presenting with paraneoplastic limbic encephalitis. J Clin Oncol. 2007; 25:3783–3785.
Article12. Howe MC, Chapman A, Kerr K, Dougal M, Anderson H, Hasleton PS. Neuroendocrine differentiation in non-small cell lung cancer and its relation to prognosis and therapy. Histopathology. 2005; 46:195–201.
Article13. Dabbeche C, Guyon D, Loubes-Lacroix F, Manelfe C. [Paraneoplastic limbic encephalitis associated with epidermoid lung carcinoma]. J Neuroradiol. 2005; 32:278–280.14. Voltz R. Paraneoplastic neurological syndromes: an update on diagnosis, pathogenesis, and therapy. Lancet Neurol. 2002; 1:294–305.
Article15. Gultekin SH, Rosenfeld MR, Voltz R, Eichen J, Posner JB, Dalmau J. Paraneoplastic limbic encephalitis: neurological symptoms, immunological findings and tumour association in 50 patients. Brain. 2000; 123(Pt 7):1481–1494.
Article16. Schüller M, Jenne D, Voltz R. The human PNMA family: novel neuronal proteins implicated in paraneoplastic neurological disease. J Neuroimmunol. 2005; 169:172–176.
Article17. Darnell RB, Posner JB. Paraneoplastic syndromes involving the nervous system. N Engl J Med. 2003; 349:1543–1554.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Anti-Ma2-Associated Encephalitis with Axonal Sensorimotor Polyneuropathy
- A Case of Limbic Encephalitis Associated with Small Cell Lung Cancer: About Diagnostic MRI Findings
- A Case of Paraneoplastic Limbic Encephalitis Associated with Immature Ovarian Teratoma
- A Case of Paraneoplastic Limbic Encephalitis Associated with Primary Adenocarcinoma of Lung
- Non-paraneoplastic Autoantibody-negative Limbic Encephalitis Characterized by Mild Memory Impairment: A Case Report