Ann Dermatol.
2015 Aug;27(4):398-403. 10.5021/ad.2015.27.4.398.
Antibiotic Susceptibility of Staphylococcus aureus in Atopic Dermatitis: Current Prevalence of Methicillin-Resistant Staphylococcus aureus in Korea and Treatment Strategies
- Affiliations
-
- 1Department of Dermatology, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea. junmo.yang@samsung.com
- KMID: 2171496
- DOI: http://doi.org/10.5021/ad.2015.27.4.398
Abstract
- BACKGROUND
Staphylococcus aureus is a well-known microbe that colonizes or infects the skin in atopic dermatitis (AD). The prevalence of methicillin-resistant S. aureus (MRSA) in AD has recently been increasing.
OBJECTIVE
This study aimed to determine the antimicrobial susceptibility patterns in AD skin lesions and evaluate the prevalence of MRSA in Korea. We also recommend proper first-line topical antibiotics for Korean patients with AD.
METHODS
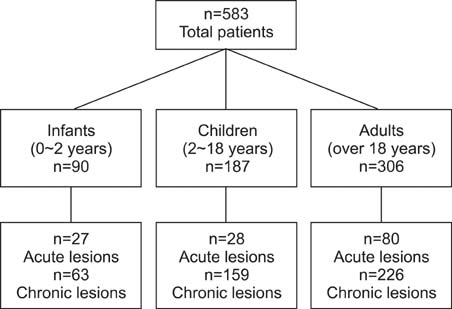
We studied S. aureus-positive skin swabs (n=583) from the lesional skin of infants, children, and adults who presented to our outpatient clinic with AD from July 2009 to April 2012.
RESULTS
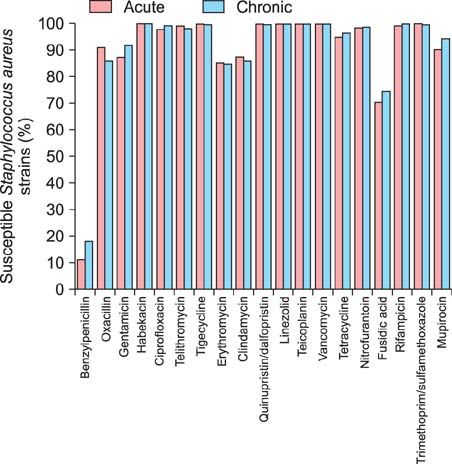
S. aureus exhibited high susceptibility against most antimicrobial agents. However, it exhibited less susceptibility to benzylpenicillin, erythromycin, clindamycin, and fusidic acid. The prevalence of MRSA was 12.9% among 583 S. aureus isolates, and the susceptibility to oxacillin was significantly lower in infants in both acute and chronic AD lesions.
CONCLUSION
S. aureus from AD has a high prevalence of MRSA and multidrug resistance, especially in infants. In addition, the rate of fusidic acid resistance is high among all age groups, and mupirocin resistance increases with age group regardless of lesional status. This is the first study comparing the antimicrobial susceptibility rates of S. aureus isolates from AD cases with respect to age and lesion status in Korea.
Keyword
MeSH Terms
-
Adult
Ambulatory Care Facilities
Anti-Bacterial Agents
Anti-Infective Agents
Child
Clindamycin
Colon
Dermatitis, Atopic*
Drug Resistance, Multiple
Erythromycin
Fusidic Acid
Humans
Infant
Korea*
Methicillin Resistance*
Methicillin-Resistant Staphylococcus aureus*
Mupirocin
Oxacillin
Penicillin G
Prevalence*
Skin
Staphylococcus aureus*
Staphylococcus*
Anti-Bacterial Agents
Anti-Infective Agents
Clindamycin
Erythromycin
Fusidic Acid
Mupirocin
Oxacillin
Penicillin G
Figure
Reference
-
1. Breuer K, HAussler S, Kapp A, Werfel T. Staphylococcus aureus: colonizing features and influence of an antibacterial treatment in adults with atopic dermatitis. Br J Dermatol. 2002; 147:55–61.
Article2. Gong JQ, Lin L, Lin T, Hao F, Zeng FQ, Bi ZG, et al. Skin colonization by Staphylococcus aureus in patients with eczema and atopic dermatitis and relevant combined topical therapy: a double-blind multicentre randomized controlled trial. Br J Dermatol. 2006; 155:680–687.
Article3. Higaki S, Morohashi M, Yamagishi T, Hasegawa Y. Comparative study of staphylococci from the skin of atopic dermatitis patients and from healthy subjects. Int J Dermatol. 1999; 38:265–269.
Article4. Barrett FF, McGehee RF Jr, Finland M. Methicillin-resistant Staphylococcus aureus at Boston City Hospital. Bacteriologic and epidemiologic observations. N Engl J Med. 1968; 279:441–448.
Article5. Park SY, Kim SM, Park SD. The prevalence, genotype and antimicrobial susceptibility of high- and low-level mupirocin resistant methicillin-resistant Staphylococcus aureus. Ann Dermatol. 2012; 24:32–38.
Article6. Dukic VM, Lauderdale DS, Wilder J, Daum RS, David MZ. Epidemics of community-associated methicillin-resistant Staphylococcus aureus in the United States: a meta-analysis. PLoS One. 2013; 8:e52722.
Article7. Bratu S, Landman D, Gupta J, Trehan M, Panwar M, Quale J. A population-based study examining the emergence of community-associated methicillin-resistant Staphylococcus aureus USA300 in New York City. Ann Clin Microbiol Antimicrob. 2006; 5:29.
Article8. Popovich KJ, Hota B, Aroutcheva A, Kurien L, Patel J, Lyles-Banks R, et al. Community-associated methicillinresistant Staphylococcus aureus colonization burden in HIV-infected patients. Clin Infect Dis. 2013; 56:1067–1074.
Article9. Calfee DP. Methicillin-resistant Staphylococcus aureus and vancomycin-resistant enterococci, and other Gram-positives in healthcare. Curr Opin Infect Dis. 2012; 25:385–394.
Article10. Mediavilla JR, Chen L, Mathema B, Kreiswirth BN. Global epidemiology of community-associated methicillin resistant Staphylococcus aureus (CA-MRSA). Curr Opin Microbiol. 2012; 15:588–595.
Article11. Moran GJ, Krishnadasan A, Gorwitz RJ, Fosheim GE, McDougal LK, Carey RB, et al. EMERGEncy ID Net Study Group. Methicillin-resistant S. aureus infections among patients in the emergency department. N Engl J Med. 2006; 355:666–674.
Article12. Moet GJ, Jones RN, Biedenbach DJ, Stilwell MG, Fritsche TR. Contemporary causes of skin and soft tissue infections in North America, Latin America, and Europe: report from the SENTRY Antimicrobial Surveillance Program (1998-2004). Diagn Microbiol Infect Dis. 2007; 57:7–13.
Article13. Hill SE, Yung A, Rademaker M. Prevalence of Staphylococcus aureus and antibiotic resistance in children with atopic dermatitis: a New Zealand experience. Australas J Dermatol. 2011; 52:27–31.
Article14. Hoeger PH. Antimicrobial susceptibility of skin-colonizing S. aureus strains in children with atopic dermatitis. Pediatr Allergy Immunol. 2004; 15:474–477.
Article15. Niebuhr M, Mai U, Kapp A, Werfel T. Antibiotic treatment of cutaneous infections with Staphylococcus aureus in patients with atopic dermatitis: current antimicrobial resistances and susceptibilities. Exp Dermatol. 2008; 17:953–957.
Article16. Tang CS, Wang CC, Huang CF, Chen SJ, Tseng MH, Lo WT. Antimicrobial susceptibility of Staphylococcus aureus in children with atopic dermatitis. Pediatr Int. 2011; 53:363–367.
Article17. Chung HJ, Jeon HS, Sung H, Kim MN, Hong SJ. Epidemiological characteristics of methicillin-resistant Staphylococcus aureus isolates from children with eczematous atopic dermatitis lesions. J Clin Microbiol. 2008; 46:991–995.
Article18. Park HY, Kim CR, Huh IS, Jung MY, Seo EY, Park JH, et al. Staphylococcus aureus colonization in acute and chronic skin lesions of patients with atopic dermatitis. Ann Dermatol. 2013; 25:410–416.
Article19. Matlow A, Forgie S, Pelude L, Embree J, Gravel D, Langley JM, et al. Canadian Nosocomial Infection Surveillance Program. National surveillance of methicillin-resistant Staphylococcus aureus among hospitalized pediatric patients in Canadian acute care facilities, 1995-2007. Pediatr Infect Dis J. 2012; 31:814–820.
Article20. Shah M, Mohanraj M. High levels of fusidic acid-resistant Staphylococcus aureus in dermatology patients. Br J Dermatol. 2003; 148:1018–1020.
Article21. Ravenscroft JC, Layton A, Barnham M. Observations on high levels of fusidic acid resistant Staphylococcus aureus in Harrogate, North Yorkshire, UK. Clin Exp Dermatol. 2000; 25:327–330.
Article22. Andersen BM, Bergh K, Steinbakk M, Syversen G, Magnaes B, Dalen H, et al. A Norwegian nosocomial outbreak of methicillin-resistant Staphylococcus aureus resistant to fusidic acid and susceptible to other antistaphylococcal agents. J Hosp Infect. 1999; 41:123–132.
Article23. Brown EM, Thomas P. Fusidic acid resistance in Staphylococcus aureus isolates. Lancet. 2002; 359:803.24. Yun HJ, Lee SW, Yoon GM, Kim SY, Choi S, Lee YS, et al. Prevalence and mechanisms of low- and high-level mupirocin resistance in staphylococci isolated from a Korean hospital. J Antimicrob Chemother. 2003; 51:619–623.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Detection of Multidrug Resistant Patterns and Associated - genes of Methicillin Resistant Staphylococcus aureus ( MRSA ) Isolated from Clinical Specimens
- A statistical analysis of methicillin-resistant staphylococcus aureus
- A case of multiple furunculosis caused by methicillin-resistant staphylococcs aureus
- Community-associated methicillin-resistant Staphylococcus aureus (CA-MRSA)
- Colonization of Staphylococcus aureus and sensitivity to antibiotics in children with atopic dermatitis